Congenital heart defects in infants. Congenital heart defect
According to statistics, about 8 out of 1000 children are born with one or more heart defects. Back in the last century, the diagnosis of "congenital heart disease in newborns" (abbreviated as CHD) sounded like a sentence and meant that life could be interrupted at any moment. However modern achievements and high-tech equipment help to prolong life and make it as high quality as possible.
Congenital heart disease in newborns is a defect in the structure of the heart, observed from birth, but often formed during prenatal development. The defect either interferes with normal blood flow (for example, when the valve apparatus malfunctions), or affects the quality of blood filling with oxygen and carbon dioxide.
Facts about UPU
- CHD in newborns is one of the most common defects at birth (in second place after pathologies of the nervous system).
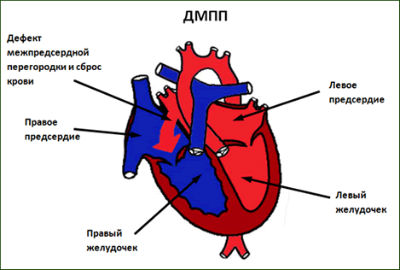
- Most frequent vices- septal defects: interventricular and interatrial.
- Not always, when a congenital heart disease is detected, an operation is required.
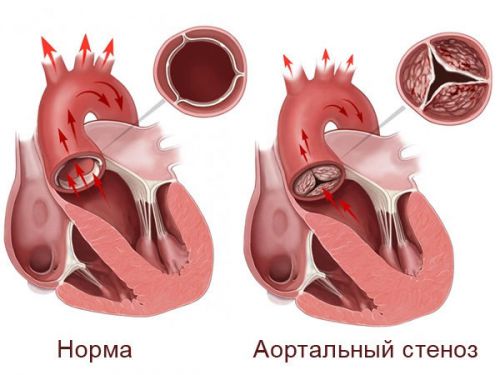
- There is a definite relationship between the type of congenital heart disease and the sex of the fetus. As a result of one study, it turned out that conditionally congenital heart defects are divided into 3 groups: male, female and neutral. For example, an open ductus arteriosus is called a "female" defect, and a prime example"male" - aortic stenosis.
Causes
Cordially- vascular system formed on early dates, from 10 to 40 days of development. That is, starting from the third week of pregnancy, when a woman in most cases still does not know about her position, and ending with the second month, the chambers and septa of the heart, the main vessels are laid in the embryo. Exactly this dangerous time in terms of the development of heart defects.
Cardiac pathologies originate at the beginning of the formation of the vascular system
A certain “seasonality” of the birth of babies with congenital heart defects was noticed, which, on the one hand, is explained by the season of viruses and colds on an epidemic scale. On the other hand, only the transferred viral diseases do not mean that the child will be born with a pathology. Influenza viruses are considered potentially dangerous herpes simplex, the rubella virus most detrimental to the fetus. Exists whole line other factors affecting the causes of pathology:
- hereditary predisposition.
- Living in an ecologically negative region.
- Work in enterprises with harmful conditions labor (work with paint and varnish products, salts heavy metals, radiation).
- Bad habits. The frequency of birth of infants with heart defects in mothers who abuse alcohol is from 30 to 50%.
- Age. The risk increases if the father and mother are over 35 years old.
- Acceptance of certain medicines in the first trimester (barbiturates, antibiotics, papaverine, hormonal preparations, narcotic analgesics).
- Some parental illnesses, such as diabetes.
- Previous pregnancies ended in stillbirth.
- Severe toxicity.
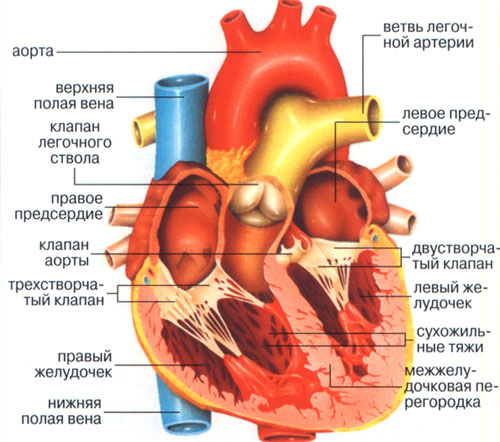
How our heart works
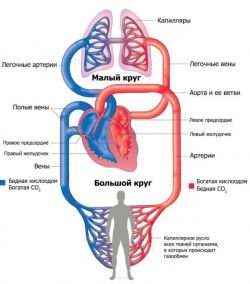
Diagram showing how the heart works
To understand the essence congenital anomalies, let's first remember how the heart muscle works. Our heart is divided into two parts. The left, like a pump, pumps oxygenated arterial blood, it is bright red. The right side promotes the movement of venous blood. Its darker burgundy hue is due to the presence of carbon dioxide. IN normal condition venous and arterial blood never mix due to the dense partition between them.
Blood circulates through our body with the help of two circulation circles where the heart plays significant role. big circle(BCC) "starts" from the aorta emerging from the left ventricle of the heart. The aorta branches into many arteries that carry oxygen-enriched blood to tissues and organs. Giving oxygen, the blood “takes” carbon dioxide and other metabolic products from the cells. So it becomes venous and rushes along the tributaries of the superior and inferior vena cava to the heart, completing the BCC, entering right atrium.
The small circle (MKC) is designed to remove carbon dioxide from the body and saturate the blood with oxygen. From the right atrium deoxygenated blood enters the right ventricle, from where it is released into the pulmonary trunk. Two pulmonary arteries deliver blood to the lungs, where the process of gas exchange takes place. Having become arterial, the blood is transported to the left atrium. This is how the ICC closes.
The valvular apparatus of the heart plays a huge role in the flawless functioning of blood circulation. Valves are located between the atria and ventricles, as well as at the entrance and exit of large vessels. Since the BCC is longer than the small one, a large load falls on the left atrium and ventricle (it is not for nothing that the muscle wall on the left side is thicker than on the right). For these reasons, defects with a bicuspid mitral valve (serving as the boundary between the left atrium and ventricle) and aortic valve (located at the border of the exit of the aorta from the left ventricle) often occur.
Classification and symptoms
There are many classifications of heart disease in newborns, among which the most famous classification by color is:
- "Pale". Pallor skin, shortness of breath, heart and headaches (defects of the interventricular and interatrial septum, stenosis).
- "Blue". The most unfavorable in terms of complications. The color of the skin becomes cyanotic, there is a mixture of arterial and venous blood (tetralogy of Fallot, transposition main vessels).
- "Neutral".
Ideally, the defect is determined by the neonatologist when listening to the child's heart. However, in practice this is not always possible, so close attention is paid to such signs as the condition of the skin and the dynamics of breathing. So, the main symptoms indicating cardiac pathologies are as follows:
- cyanosis (cyanosis) of the skin, blueness of the nasolabial triangle during feeding;
- crashes heart rate;
- heart murmurs that do not go away for a certain period;
- heart failure in a pronounced form;
- dyspnea;
- lethargy along with weakness;
- spasms peripheral vessels(limbs and tip of nose pale, cool to the touch);
- gaining weight poorly;
- puffiness.

Heart murmurs can be heard an experienced doctor immediately after birth
Even mild signs should not be ignored. Make an appointment with a cardiologist and undergo an additional examination.
Diagnostics
With the prevalence of ultrasound examinations, most CHD can be recognized as early as 18-20 weeks of gestation. This makes it possible to prepare and carry out, if necessary, surgical work immediately after birth. So children have a chance to survive with those types of vice that were previously considered incompatible with life.
Heart defects are not always detected during fetal development. However, with birth, often clinical picture is growing. Then the baby is sent to a cardiologist or cardiac surgeon for examination and diagnosis. The most common research methods are:
- Electrocardiogram (ECG). Gives general idea about the work of the heart (which departments are overloaded, the rhythm of contractions, conduction).
- Phonocardiogram (PCG). Records heart sounds on paper.
- Echocardiography. The method helps to assess the state of the valvular apparatus, cardiac muscles, determine the speed of blood flow in the cavities of the heart.
- Survey radiography of the heart.
- Pulse oximetry. Allows you to determine how oxygenated the blood is. A special sensor is attached to the fingertip. Through it, the oxygen content in the erythrocyte is determined.
- Doppler study. An ultrasonic color flow study assessing the size and anatomy of the defect, as well as determining the volume of blood flowing in the wrong direction.
- catheterization. Probes are inserted into the cavity of the heart through the vessels. The method is rarely used in complex and controversial cases.
Target diagnostic measures- answer the following questions:
- What is the anatomy of the defect, where is the blood circulation disturbed?
- How to form final diagnosis?
- In which of the three phases is the vice?
- Is there a need for surgical intervention or at this stage can be dispensed with conservative methods treatment?
- Are there any complications that need to be treated?
- What is the tactic surgical treatment And when will it be optimal?
Kinds
Although congenital malformations are found even in the womb, in most cases they do not pose a threat to the fetus, since its circulatory system is slightly different from an adult. But after birth, when the heart begins to work at full strength and two circles of blood circulation are launched, the clinical picture becomes apparent. Below are the main heart defects.
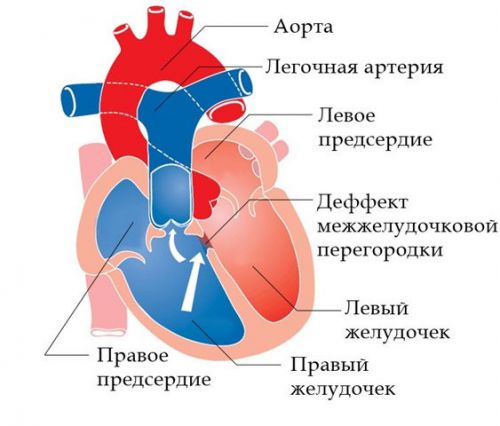
The most common pathology. Arterial blood enters through the opening from the left ventricle to the right. This increases the load on the small circle and on left side hearts.
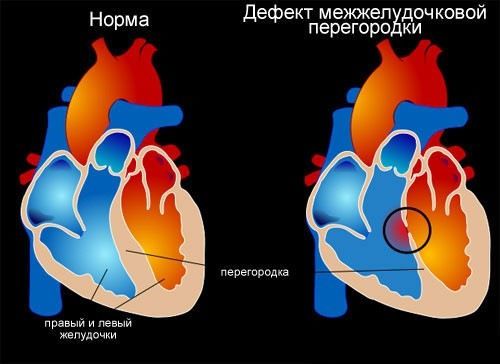
When the hole is microscopic and causes minimal changes in the circulation, the operation is not done. At large sizes holes make suturing. Patients live to old age.
Eisenmenger complex
A condition where the interventricular septum is severely damaged or absent altogether. In the ventricles, a mixture of arterial and venous blood occurs, the oxygen level drops, cyanosis of the skin is pronounced. For preschool and school age a forced position to squat is characteristic (this reduces shortness of breath). On ultrasound, an enlarged spherical heart is visible, a cardiac hump (protrusion) is noticeable.
The operation should be done without delay, because without appropriate treatment, patients in best case live up to 30 years.
Occurs when, for some reason, postpartum period the communication of the pulmonary artery and aorta remains open. The outcome is the same as in the situations described above: two types of blood mix, the small circle is overloaded with work, the right ventricle enlarges, and after a while the left ventricle. In severe cases, the disease is accompanied by cyanosis and shortness of breath.
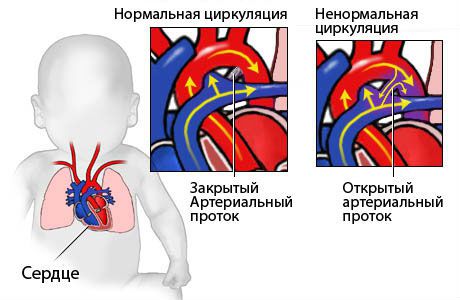
A small cleft diameter is not dangerous, while a large defect requires urgent surgical intervention.
The most severe defect, which includes four anomalies at once:
- stenosis (narrowing) of the pulmonary artery;
- defect interventricular septum;
- dextraposition of the aorta;
- enlargement of the right ventricle.
Modern techniques make it possible to treat such defects, but a child with such a diagnosis is registered with a cardiorheumatologist for life.
Stenosis is a narrowing of a vessel that blocks blood flow. It is accompanied by a tense pulse in the arteries of the arms, and a weakened pulse in the legs, a big difference between pressure on the arms and legs, burning sensation and heat in the face, numbness lower extremities.
The operation involves the installation of a transplant on the damaged area. After the measures taken, the work of the heart and blood vessels is restored and the patient lives for a long time.
Treatment
Treatment, its tactics, will depend on the severity of the defect and on what phase its development is in. In total, there are three of them: emergency, phase of compensation and decompensation.
emergency originates from the birth of a baby, when organs and systems get a kind of shake-up due to a lack of oxygen and try to adapt to extreme conditions. Vessels, lungs and heart muscles work with maximum efficiency. If the body is weak, defect, in the absence of urgent surgical care leading to the death of the infant.
Stage of compensation. If the body was able to compensate for the missing opportunities, the organs and systems are able to work more or less stably for some time, until all the forces are exhausted.
Stage of decompensation. Occurs when the body is no longer able to carry increased load, and the organs of the cardiac and pulmonary groups cease to perform their functions to the fullest. This provokes the development of heart failure.
The operation, as a rule, is carried out in the compensation phase, when the work of organs and systems is established and occurs at the expense of their reserves. With some types of defect, the operation is indicated in the emergency stage, in the first days or even hours after the birth of the crumbs, so that he can survive. In the third phase surgical intervention most of the time it's pointless.
Sometimes doctors have to do so-called intermediate surgical interventions that allow the child to live until the time when full reconstructive operation with minimal consequences. In surgical practice, minimally invasive techniques are often used, when small incisions are made using endoscopic equipment and all manipulations are visible through an ultrasound machine. Even general anesthesia is not always used.
After getting rid of the vice, the baby needs time to rebuild to live without it again. Therefore, the baby is registered with a cardiologist and regularly visits him. Important role plays the strengthening of immunity, since any cold can adversely affect the cardiovascular system and health in general.

Long walks on fresh air are simply necessary, especially for children with heart pathologies
Concerning exercise at school and kindergarten, the degree of load is determined by a cardiorheumatologist. If exemption from physical education classes is necessary, this does not mean that the child is contraindicated to move. In such cases, he does physical therapy By special program in the clinic.
Children with CHD are shown to stay outdoors for a long time, but in the absence of extreme temperatures: both heat and cold have a bad effect on vessels that work “for wear”. Salt intake is limited. In the diet, the presence of foods rich in potassium is mandatory: dried apricots, raisins, baked potatoes.
Conclusion. Vices are different. Some require immediate surgical treatment, others are under constant surveillance doctors to certain age. In any case, today medicine, including cardiac surgery, has stepped forward, and vices that were considered incurable and incompatible with life 60 years ago are now successfully operated on and children live long. Therefore, hearing terrible diagnosis, do not panic. You need to tune in to fight the disease and do everything on your part to defeat it.
Congenital heart defects are several diseases associated with the presence of anatomical pathology of the heart, its valves and blood vessels, formed during fetal development. These defects cause changes in the systemic and intracardiac circulation, heart overload.
Symptoms of the disease are due to the type of defect, most often cyanosis (cyanosis) or pallor of the skin, lag in physical development, heart murmurs, manifestation of cardiac and respiratory failure. If the doctor suspected a congenital heart disease, FKG, ECG, EchoCG, and radiography are performed.
Many types of cardiac disorders are combined with each other or other systemic pathologies in the body. CHD is much less common in adults than in childhood. Identification of violations can occur even in adulthood.
Why are heart pathologies formed?
To begin with, it is necessary to highlight the risk factors that contribute to the formation of heart anomalies:
- mother's age up to 17 years or after 40 years;
- the threat of termination of pregnancy;
- toxicosis of the first trimester;
- endocrine diseases in a pregnant woman;
- stillbirth in history;
- burdened heredity.
Causes of congenital heart defects can be the following: chromosomal abnormalities, the impact of environmental factors, gene mutations, polygenic multifactorial predisposition (heredity).
When laying chromosomes, their structural or quantitative change is possible. In this case, there are anomalies in various bodies and systems, and in the cardiovascular system as well. Trisomy of autosomes usually develops septal defects of the heart.
With mutations of single genes, congenital heart defects are usually associated with other defects of other organs. Then cardiac anomalies are part of autosomal recessive, autosomal dominant, or X-linked syndromes.
During pregnancy (up to three months) such negative factors, such as ionizing radiation, viral diseases, certain medications, occupational hazards and addictions mothers contribute to improper laying of organs.
If the fetus in utero is affected by the rubella virus, then most often the child develops a triad of anomalies - deafness, glaucoma or cataracts, a malformation of the heart.
Also, syphilis, herpes, chicken pox, mycoplasmosis, adeno viral infections, cytomegaly, diabetes, serum hepatitis, toxoplasmosis, tuberculosis, listeriosis, etc.
Scientists have found that cardiac intrauterine development is affected by various medicines: progestogens, amphetamines, lithium preparations and anticonvulsants.
Circulatory disorders
Due to the above factors in fetal development in the fetus, the natural formation of heart structures can be disrupted, which causes incomplete closure between the ventricles and atria, pathological formation valves, abnormal arrangement of vessels, etc.
After birth, some babies do not close the oval window and ductus arteriosus
Since the blood circulation inside the mother differs from the hemodynamics of the newborn, the symptoms appear almost immediately after childbirth.
How quickly congenital heart disease manifests itself depends on many factors, including individual features child's body. In some cases, the formation of gross circulatory disorders, causes respiratory infection or some other disease.
With cardiac defects of the heart, hypertension of the pulmonary circulation or hypoxemia (low oxygen content in the blood) may appear.
Approximately half of children die without appropriate care in the first year of life from manifestations of heart failure. In babies, after a year, the state of health normalizes, but persistent complications develop. Therefore, in some cases, surgery is necessary at an early age.
Classification of violations
Classification of congenital heart defects based on effects on pulmonary blood flow:
- with increased blood flow: not causing early cyanosis and causing cyanosis;
- with unchanged;
- with depleted: without cyanosis and with cyanosis;
- combined.
There is another classification by groups:
- White, which, in turn, can be with enrichment or depletion of any circle of blood circulation and without a significant violation of blood circulation.
- Blue, which come with enrichment or depletion of the small circle.
According to the ICD ( international classification diseases) congenital anomalies of the circulatory system occupy positions from Q20 to Q28, it is heart anomalies that are included in Q24.
Complications
Complications of CHD are syncope (fainting), heart failure, pulmonary hypertension, impaired cerebral circulation, angina, bacterial endocarditis, prolonged pneumonia, myocardial infarction, relative anemia and dyspnea-cyanotic attacks.
Clinical manifestations (symptoms) or how to recognize the disease?

Children refuse to breastfeed, restless, quickly get tired in the process of sucking
Symptoms of congenital heart defects depend on the type of disorders, the time of formation of hemodynamic decompensation and the nature of circulatory disorders.
In infants with a cyanotic type of disease, cyanosis of the skin and mucous membranes is observed. It becomes more pronounced with crying and sucking. White anomalies of the heart are detected by coldness of the hands and feet, pallor of the skin.
They develop tachycardia, sweating, shortness of breath, arrhythmias, pulsation and swelling of the vessels of the neck. With a prolonged violation of hemodynamics, the child lags behind in height, weight and physical development.
Usually, immediately after birth, heart murmurs are heard during auscultation.
Diagnostics
Diagnosis of congenital heart defects is carried out using comprehensive survey. The first step is to examine the child and auscultate the heart. If there is suspicion of possible anomalies, then are assigned instrumental methods diagnostics - phonocardiography, electrocardiography, echocardiography, radiography chest.
The ECG makes it possible to recognize the hypertrophy of the heart, the presence of conduction disorders and arrhythmias, after the manipulation it becomes easier to judge the severity of the violations. Daily monitoring is possible.
FCG data help to thoroughly assess the duration, nature and location of heart murmurs and tones. Radiography allows you to identify the shape, location and size of the heart, the state of the pulmonary circulation.
Through echocardiography, valves, septa and main vessels are examined, contractility myocardium.
For complex disorders and pulmonary hypertension it is possible to perform other diagnostic methods: aorto- or angiocardiography, probing and catheterization of the heart cavities, MRI of the heart, cardiography.
Treatment
Related article:
A serious problem in cardiology in children under one year old is surgical treatment congenital heart defects. If the child has no symptoms of heart failure, and cyanosis is moderate, then the operation can be postponed for more late deadline. Babies should be constantly under the supervision of a cardiac surgeon or cardiologist.
The method of treatment is selected depending on the severity and type of CHD. In case of anomalies of the septa of the heart, they are sutured or plastic, X-ray endovascular occlusion of the defect is possible.
In case of severe hypoxemia, for a temporary improvement in the condition of children, intersystemic anastomoses are first performed. As a result, the risk of complications is reduced, blood oxygenation is increased. A radical operation is performed when favorable conditions occur.
With aortic anomalies, resection of the aorta, plastic stenosis is performed. When the aortic duct is opened, it is ligated.
Treatment of complex heart defects, which cannot be completely eliminated, consists in hemodynamic correction. In some cases, the only possible method The therapy for congenital heart disease is heart transplantation.
Medical treatment includes only symptomatic therapy arrhythmias, acute left ventricular or chronic heart failure, dyspnea-cyanotic attacks, myocardial ischemia.
In addition to treatment, the child needs special attention parents: proper nutrition, prevention of viral diseases, etc.
The prognosis for early diagnosis and the possibility of treatment is relatively favorable. If it is impossible to carry out the operation - unfavorable.
It is possible to get disability after radical operation during the rehabilitation period and with symptoms of heart failure stage II B or more.
Prevention
Prevention of CHD includes careful planning of pregnancy, prenatal diagnosis, exclusion of the impact of adverse factors.
Women with heart anomalies need careful attention during pregnancy by doctors and additional consultations and examinations.
Causes of congenital heart defects

There are many various reasons occurrence of congenital heart disease (CHD).
All of them in combination affect the body of a pregnant woman, disrupting the processes of formation of organs and systems of the fetus. Seasonal fluctuations in the occurrence of CHD are mainly associated with viral epidemics. In particular, the teratogenic (i.e., causing malformations) effect on the fetus of the rubella virus has been accurately proven, cytomegalovirus infection, chicken pox. There is data of the same nature for influenza viruses, especially if the disease occurs in the first three months of pregnancy. Of course, the presence of only a viral factor for the development of CHD is doubtful. However, the combination of several teratogenic factors increases the risk of CHD. A viral agent can only become a trigger mechanism in the implementation of genetic mechanisms. A certain role in the formation of CHD is assigned to the use of alcohol during pregnancy, and we are talking not only about strong alcohol, but also low-alcohol cocktails, tonics, etc. In women who consume alcoholic beverages, children with CHD are born in 50% of cases. A large role during pregnancy is given to the general somatic health of a woman. In women suffering systemic diseases(for example, systemic lupus erythematosus), diabetes more children are born with congenital heart disease.
congenital heart defects
Congenital heart defects (CHD) are defects in the development of this organ that exist at birth. The reason is misdevelopment heart or blood vessels near the heart even before the baby is born.

The frequency of this pathology is 8 per 1000 children. This is almost 1% of newborn babies.
Despite the fact that heart defects are the main cause of death in the structure of all anomalies, with the growth of advances in the treatment of this pathology, the chances of survival in children have increased.
Causes of congenital malformations
The cause of congenital heart defects is difficult to establish. Experts believe that in 90% of cases, deficiencies are formed under the influence of the combined effect of genetic predisposition (endogenous factor) and factors environment(exogenous). In 2% of cases, only environmental factors matter.
Endogenous factors include mutations, diseases of the parents, changes in the level of gametes, too young and old age parents.
The most powerful endogenous (internal) factor are mutations that have arisen in different periods life of the parents of the unborn child at the level of germ cells (gametes) under the influence various factors. Mutations account for about 10% of heart defects.
Of these, the share of chromosomal mutations - 5-6%, rare gene defects - 3-5%. The most common of these are Down's syndrome, which in 90% of cases is accompanied by an atrial septal defect and the so-called velo-cardiofacial syndrome. Congenital heart defects can occur with a chromosomal pathology such as Down syndrome. 25% girls on the other chromosomal abnormality, so-called Shereshevsky-Turner syndrome, have an atrial membrane defect. In the case of trisomy 18 or 13, children often die from congenital heart disease, namely, ventricular septal defect and patent ductus arteriosus.
By the way, another common vascular disease, which is most often observed in children over the age of 4 years is hemorrhagic vasculitis. a disease in which the walls of small capillaries become inflamed.
A number of diseases with gene anomalies can be accompanied by anomalies of the heart. These are Marfan syndrome, Smith-Lemle-Opitts, Holt-Oram syndrome, mucopolysaccharidosis. 80% of children with Noonan syndrome and Williams syndrome are born with congenital heart disease. In 50% of cases it is a stenosis of the pulmonary artery. Other genetic syndromes this is Goldenhar's syndrome, VACTERL association (trachea, esophagus, anomalies of the spine, rectum and anus, kidneys, limbs). Most of these syndromes are diagnosed in specialized genetic centers using molecular diagnostic methods.
Some CHD have an autosomal dominant (vertical) transmission pattern. This means that in the case of a congenital heart anomaly in one of the parents, 50% of children, regardless of gender, will be born with heart anomalies. In the presence of aggravated heredity, the birth of a child is more likely in families where close relatives had similar shortcomings. If one of the parents himself suffered from congenital heart disease, the risk of having a child with similar pathology is 10%. If the family already has a child with a congenital anomaly, everyone is at risk of having a defect next child increases by 4%. If the child has been diagnosed with a chromosomal or other genetic anomaly, genetic counseling can help in prenatal diagnosis and determine the risk of heart defects in future children
TO internal factors also includes chronic diseases of the mother. The first is diabetes. causing the so-called diabetic embryopathy with CHD, phenylketonuria, epilepsy, lupus erythematosus and folic acid hypovitaminosis. In women with uncompensated diabetes, the chances of giving birth to a child with congenital heart disease increase significantly. It is believed that 3-6% of pregnant women with diabetes mellitus most often give birth to children with transposition of the great vessels. This increased risk applies to type 1 and type 2 diabetes, but does not cover gestational diabetes, which is a temporary condition that resolves after the baby is born.
External (exogenous) factors include: physical, chemical and biological. The most important for the occurrence of CHD in a child are chemical and biological.
The group of chemical factors includes medical preparations which increase the risk of having a child with congenital heart disease. These are lithium preparations, some anticonvulsants, hormonal drugs and drugs that disrupt the absorption of folic acid. Women who take an anti-inflammatory drug like ibuprofen are twice as likely to have a baby with congenital heart disease. Paracetamol is a safer alternative in this case, although the ideal is to avoid taking any medication during pregnancy, especially in the three months before conception and during the first trimester of pregnancy. If it is impossible not to take the drug, you should coordinate the drug with an experienced doctor whom you trust.
This group also includes teratogens such as alcohol, smoking and drugs. Children born with fetal alcohol syndrome often have heart problems. Typically, this is an atrial septal defect. According to research smoking women 60% more likely to give birth to children with an abnormal structure of the heart and blood vessels. The same effect has passive smoking, since a third harmful substances while being released into the environment. In a relationship narcotic substances cocaine has the same effect.
TO chemical factors also include organic solvents, which increase the risk of having a child with a defect in the heart and blood vessels three times.
From biological factors viral infections are dangerous. If a woman gets rubella during pregnancy (in the first 8-10 weeks), the risk of developing congenital heart disease increases to 35%. All women reproductive age must be vaccinated against rubella, after which they avoid pregnancy for 1 month after vaccination. Women who have had influenza in the first trimester of pregnancy are twice as likely to give birth to babies with defects in the heart and blood vessels.
Most UPUs cannot be prevented. But with diet and proper therapy chronic diseases, timely treatment intrauterine infections(rubella, toxoplasmosis), HIV infection in the mother, these problems can be avoided. To give birth to a healthy child, a woman must stop using substances such as alcohol, smoking, and the use of dangerous medicines three months before conception.
The term "congenital heart disease" is understood to mean a disorder that has arisen in utero or anatomical structure heart, or outgoing / flowing into it vessels, or valves located between the main cardiac cavities. There may be a combination of various defects among themselves or with anomalies in the development of internal organs.
There are more than 100 types of congenital heart defects (CHDs). Some of them increase the amount of blood going to the lungs, others reduce it, and others do not affect this indicator. In addition, each defect may have its own degree of severity, and this affects the course of the disease. Therefore, some anomalies of the heart and blood vessels are visible from birth and require an emergency life-saving operation, others are not so acute and are treated with medication (at least for a while). In some cases, heart defects appear suddenly and not in the first year of life.
Symptoms of heart defects range from mild to life threatening. This is usually rapid breathing, the acquisition of a bluish tint to the skin, poor weight gain, and fatigue when sucking. For heart defects, chest pain is not typical.
Some anatomy and physiology
This information will be useful to those who want to understand why a certain defect is more dangerous and why it has such symptoms.
The heart is an organ that functions as a pump. It is built from four chambers - two atria and two ventricles. They are all made of three layers. Internal - endocardium - performs partitions between the heart chambers:
- Between the atrium and ventricle, they look like valves. They open under the pressure of blood entering the atrium to pass it into the ventricle. After the blood flows into the ventricle, the valve leaflets must close and prevent blood from flowing back into the atrium. Between the left chambers of the heart is the bicuspid mitral valve, between the right ones - a valve consisting of three petals, which is called “tricuspid”.
- The two ventricles are separated by the interventricular septum, a rather dense structure 7.5-11 mm thick, in the middle of which is muscle tissue.
- The two atria are separated by an interatrial septum. It is thinner than the interventricular one, but, like the latter, should not have any holes.
The aorta emerges from the left ventricle - the largest vessel with a diameter of 25-30 mm. The aorta, branching into many branches of a smaller diameter, extending from it gradually, as internal organs appear in its path, carries oxygenated blood to them. Its last branches are iliac arteries. They feed pelvic organs, and also give away branches that go to the legs.
"Spent", poor in oxygen, but with an abundance of carbon dioxide, the blood departs from all internal organs through the venules that flow into the veins. The latter gradually also merge together:
- from the lower extremities, pelvis, abdomen are collected in the inferior vena cava (vena cava);
- from the arms, head, neck and lungs with the bronchi - into the upper vena cava.
Both vena cava from above and below flow into the right atrium. Full circle blood makes in 23-37 seconds.
This is a large circle of blood circulation. In its arteries, the pressure is higher than in the same vessels of the small circle.
The small, pulmonary circle of blood circulation serves to ensure that all the arterial blood of the large circle can be oxygenated - saturated with oxygen.
It originates from the right ventricle, which pushes blood into the pulmonary trunk, which soon branches to the right (goes to right lung) and left (goes to left lung) pulmonary artery. branching into ever smaller branches, arterial vessels reach the alveoli of the lungs. There they give off carbon dioxide, which a person exhales.
Oxygen does not enter the arterial, but the venous blood of the small circle. Venules with venous blood merge, forming veins, and the latter, in the amount of 4 pieces, flow into the left atrium. Blood describes such a path (circle) in 4-5 seconds.
Placental circulation
While the fetus is developing in the uterus, its lungs are not used, since there is no connection between the baby and the surrounding air. But oxygen is still supplied to the child, and this happens with the help of the placental circulation. It looks like this:
- oxygenated maternal blood enters intraplacentally;
- from the placenta, it goes along the umbilical vein, which is divided into 2 parts:
- one goes to the lower vena cava and mixes with the blood of the lower half of the body, which has already been left without oxygen;
- the second goes to portal vein, nourishes an important organ - the liver, and then is mixed with the blood of the inferior vena cava;
- thus, venous-arterial blood flows along the lower vena cava;
- By upper vein kava flows unoxygenated blood;
- from the two hollow veins, blood, as in a person after birth, enters the right atrium. But, unlike the extrauterine circulation, the right and left atria communicate with each other through the oval window;
- in the fetus, the oval opening is wide: almost all the blood from the right atrium enters the left, and then into the left ventricle;
- from the left ventricle, blood enters the aorta;
- small part blood is coming from the right atrium to the right ventricle;
- blood flows from the right ventricle into pulmonary trunk;
- since the lungs are collapsed, the pressure in the arteries that make up the pulmonary trunk is higher, so the blood has to be dumped into the aorta, where the pressure is still lower. This happens through a special vessel - the ductus botalis, which, after birth, must be overgrown. It flows into the aorta after the arteries depart from it to the head and upper limbs(that is, the latter receive more oxygenated blood);
- 60% of the blood flow of a large circle goes through 2 umbilical arteries (they go on both sides of umbilical vein) to the placenta;
- 40% of the blood from the large circle goes to the organs of the lower body.
It is precisely due to the peculiarities of the structure of the placental circle that the formed congenital heart disease does not lead to a significant deterioration in the condition of the child in utero.
Changes in the cardiovascular system are normal after birth
When a child is born, the foramen ovale, the communication between the atria, should close within the first year. This happens because when the lungs are expanded with air, the blood flow in the lungs increases. As a result, pressure in the left atrium increases, and this "pull" leads to closure oval window. It does not overgrow immediately: the more the child screams, cries, works on sucking (for example, when neurological problems or malformations such as cleft lip), the longer in this place does not form a strong connective tissue- "shutter".
The situation is more complicated with regard to the botallian duct. It should close on the first day after birth, but if the pulmonary artery remains high blood pressure, it remains open. This is facilitated by hypoxia suffered during childbirth, which leads to spasm of the pulmonary vessels.
In the first 5-7 days, the pressure in the pulmonary artery decreases during the contraction of the heart and should return to normal within 2 weeks after birth. Further, it continues to decrease, because the pulmonary vessels undergo changes: the thickened muscle layer, small pulmonary arteries disappear, some of the vessels straighten (previously they were tortuous). In addition, the alveoli expand in the lungs - the main areas in which oxygen is exchanged between the air that has entered the lungs and the blood.
The frequency of occurrence of congenital heart defects
Congenital heart disease in newborns occurs in 0.8-1.2%. In 2013, it was registered in 34.3 million people worldwide. It accounts for 10 to 30% of all congenital malformations and ranks second after malformations of the nervous system.
Depending on the nature of the diagnosis, congenital heart defects can be detected in 4-75 cases per 1000 live births. In 0.6-1.9%, they proceed moderately and severely. It is congenital heart defects that are the main cause of death of children from malformations. In 2013, for example, there were 323 thousand deaths worldwide, and in 1990 - 366 thousand. And if a child with a congenital defect lived to be 15 years old, then it is not necessary that he “outgrew” him, and the risk severe complications now lowered.
The most common heart defects are:
- ventricular septal defect (1/5 of all congenital defects);
- atrial septal defects (10-15% in the entire structure);
- open botallian duct (10-15% in the entire structure);
- coarctation of the aorta;
- aortic stenosis;
- stenosis of the pulmonary artery;
- transposition of the great vessels.
There are vices that are more common in boys, there are more characteristic ones for girls, but there are also those whose frequency is approximately the same in both sexes. Thus, in male infants, stenosis, coarctation of the aorta, transposition of the main vessels, general truncus arteriosus, tetralogy of Fallot, pulmonary artery stenosis. In girls, an open ductus arteriosus, defects of the interventricular and interatrial septum, Fallot's triad are detected. Information about the field of the developing fetus increases the likelihood early diagnosis characteristic vices.
The greatest concerns in terms of the possible presence of such defects are in premature babies and those who were born weighing less than 3 kg. It is these newborns that require the speedy implementation of all diagnostic measures in order to identify possible vices development as early as possible.
Why can a birth defect develop in the heart?
Often, the cause of heart disease in newborns cannot be detected. In some cases, this may be individual reasons or a combination of them (most often a combination of genetic factors and various external influences):
Genetic factors
It can be:
- chromosomal disorders (in 5% of cases): trisomy on chromosomes 21, 13 and 18;
- gene mutations (in 2% of cases): in the TBX5, NKX2-5, TBX1, MYH6, GATA genes
Most often, these mutations are sporadic, occur randomly and cannot be predicted before pregnancy. The fact that a child can be born with a congenital heart disease can be thought when there are (were) people in the family suffering from congenital heart defects, Down syndrome, Turner, Marfan, DiGeorge, Holt-Oram, Kartagener, Noonan and others. Heart disease should also be suspected if a similar syndrome is found in the fetus.
infectious diseases
suffered by a pregnant woman, especially if it happened at the beginning of pregnancy. The most dangerous for the developing heart of the fetus: rubella, viruses of the ARVI group (especially influenza and adenovirus infection), herpetic group (especially chickenpox and herpes simplex), viral hepatitis, cytomegaly, syphilis, tuberculosis, listeriosis, toxoplasmosis, mycoplasmosis.
Environmental factors
polluted air, radiation, living in mountainous areas or in places of high atmospheric pressure.
Toxic effects on the fetus if pregnant:
- takes certain medications: antibacterial and sulfa drugs, anticonvulsants and antiepileptic drugs (for example, Trimethadion), lithium preparations, painkillers and hormonal medications;
- smokes;
- takes drugs (especially toxic influence amphetamines on the fetal heart);
- works with paint and varnish products, nitrates;
- drink alcohol, especially initial weeks gestation.
Causes related to maternal metabolism:
when she suffers endocrine diseases(particularly diabetes mellitus), malnourished or, conversely, obese.
If a pregnant woman is sick with diseases such as:
systemic lupus erythematosus, phenylketonuria, rheumatism.
At risk
In addition, we can say that at risk for the development of congenital heart defects in children are such pregnant women:
- over 35 years old or under 15 years old;
- with a history of stillbirths;
- with a history of spontaneous miscarriages;
- with bad habits (alcohol is especially dangerous: the risk of congenital heart disease reaches 40%);
- if the child is conceived from a blood relative;
- when toxicosis of the first trimester is expressed;
- if the pregnancy proceeds with the threat of termination;
- in the family of which there are relatives with heart defects.
At what age does heart disease form?
The critical period when the above factors have a high chance of leading to the formation of heart disease is the first 3 months of pregnancy. At this time, cardiac structures are formed, and the influence of microbial, medicinal or industrial toxins on the fetal body can stop their development or lead to the formation of the heart “as in the previous stage of phylogenesis” (for example, as in reptiles, birds or amphibians). Cardiac structures are formed according to a well-defined plan, and changes in it lead to the formation of one or another defect.
Approximately on the 15th day of intrauterine development, the cells that give rise to the heart are located in the middle germinal layer (mesoderm) in the form of two horseshoe-shaped bands. Some cells migrate here from a section of the outer germ layer (ectoderm) called the "neural crest" - a department that supplies various nerve cells to various parts of the body.
On the 19th day, 1 pair of vascular elements is formed - endocardial tubes. They merge with each other, the cells between them undergo programmed death, and the cells of the primary heart migrate to the tube and form a ring of muscle cells around them by day 21. By day 22, the heart begins to contract and the blood begins to circulate.
At the time of 22 days, the vascular system is a bilaterally symmetrical system with paired vessels on each side of the body and the heart, represented by a primitive tube located in the middle, in the middle layer of the body. Its sections, from which the atria are formed, are located further from the head (although it should be the other way around).
From days 23 to 28, the heart tube folds and twists. Future ventricles move to the left side of the center, occupying their final location, and the atria - to the head end of the body. On the 28th day, the tissue of the heart tube expands, and in 2 weeks 4 heart cavities are formed here, separated by a primary membrane septum. If a damaging factor acts at this stage, blood will flow between the cavities of the heart.
Cells that have migrated from the neural crest give rise to the formation of the heart bulb, the main outflow pathway from the heart. The bulb should be divided into 2 parts by a growing spiral partition, and then ascending division aorta and pulmonary trunk. If the division by the septum does not end, a defect is formed - a persistent ductus arteriosus. And if the vessels are opposite, transposition of the main vessels is obtained.
The two halves of the outflow tract must take certain positions in certain ventricles. Under the influence of damaging factors at this stage, a defect is formed "astride aorta" (when the vessel comes from the interventricular septum).
Part of the cells of the primary septum dies, forming a hole. At the same time growing here muscle cells, forming a secondary septum, but the gap between the atria remains. This is an oval hole (window) - a shunt through which blood enters from the right to the left atrium. At the same stage, the ductus botalis is formed - a connecting channel between the aorta and the pulmonary artery.
Why are congenital heart defects dangerous?
Congenital cardiac defects lead to the development of the main symptoms and complications through one of two mechanisms:
- The flow of blood through the vessels is disrupted. For anomalies with valvular insufficiency or septal defects, heart compartments are overloaded with increased blood volume. If the defects involve narrowing (stenosis) of holes or vessels, then the heart is overloaded with resistance. First, from any overload, the cardiac muscle layer increases, and the strength of its contractions increases. After that, the compensation mechanisms “break down”, and the muscles of the enlarged heart become thinner. So the systemic circulation is disturbed - cardiac insufficiency develops.
- There is a violation of the systemic blood flow: either there is a lot of blood in a small circle, or there is little blood in one of the circles. Because of this, the supply of oxygen to the organs deteriorates.
With "blue" defects, less oxygen is delivered due to a violation of the rate of blood movement through the vessels. When the defect is "white", hypoxia is associated with difficulties in the release of oxygen by hemoglobin molecules.
These pathogenetic mechanisms are the basis for the classification of congenital heart defects by phases, which, in turn, is used to determine treatment tactics. So, there are 3 phases of the course of the disease:
1 phase - compensatory and adaptive. The body compensates for the violations that have arisen by increasing the saturation of the work of the myocardium.
Phase 2 is relatively compensatory. The heart muscle functions no longer so intensively. The structure and regulation of the heart is disturbed. The physical development of the child and physical activity are improving.
3 phase - terminal. It occurs when the compensatory capabilities of the heart are exhausted, which is why the myocardium and internal organs develop dystrophic changes. This stage ends with death. Hasten her advance infectious diseases, lung diseases and other pathologies.
Classification of congenital cardiac defects
There are over 100 forms of congenital heart anomalies. According to the nature of changes in blood circulation and, accordingly, the main symptoms, there are 2 main types of defects - "blue" (with them the child's skin has a bluish tint) and "white" (the baby's skin is pale). They also have their division.
"White" anomalies:
with them, arterial and venous blood do not mix. But this does not exclude the possibility of a discharge of blood from a more high pressure(from the left ventricle, that is, the large circle) to the lower region (to the right ventricle - the "source" of the pulmonary circulation):
- defects in which the volume of blood in the small circle increases. This is a functioning ductus arteriosus, atrial and ventricular septal defect, atrioventricular communication;
- anomalies associated with a decrease in the amount of blood in the small circle: for example, isolated stenosis of the pulmonary trunk;
- malformations that caused reduction (depletion) in the blood of a large circle: isolated stenosis aortic orifice, coarctation of the aorta;
- without much blood flow from right to left. This happens when the heart is arranged normally, but is not located in its place, but on the right (dextrocardia), in the middle of the chest (mesocardia), in abdominal cavity(abdominal dystopia of the heart), neck (cervical dystopia). A similar type of defect is also characteristic of the bivalve aortic valve(it must be three-leaved)
"Blue" defects, when there is a mixing of arterial and venous blood:
- when there is an enrichment of the pulmonary circulation (Eisenmenger's syndrome, transposition of the great vessels);
- with depletion of the small circle: Fallot's tetrad, Ebstein's defect.
How congenital heart disease manifests itself
Symptoms of heart disease depend on the type of pathology.
Signs of "blue" vices
Such defects as an unclosed arterial trunk, Fallot's tetralogy, congenital fusion (stenosis) of the tricuspid valve, anomaly of the connection of the pulmonary veins are manifested by the following symptoms:
- the lips and nasolabial triangle may be bluish at rest (if the malformation is severe), but this color may appear only when screaming, sucking, or physical activity;
- cyanotic fingers, which eventually take on the appearance of " drumsticks»: thin completely, but thickened in the area of the nail phalanges;
- rough murmur over the heart;
- frequent infectious diseases, pneumonia;
- weakness;
- quickening of breathing;
- delayed physical and mental development;
- short children;
- puberty occurs late.
In addition to changes in skin color, fatigue, weakness, shortness of breath, changes in heart rate, CHD should be suspected if one of these anomalies (abbreviation VACTERL) is found in a child:
- V - anomalies of the spine (vertebral);
- A - anal atresia;
- C - cardiovascular (cardiovascular) anomalies;
- T - transesophageal fistula (abnormal connections between the esophagus and other organs);
- E - esophageal (esophageal) atresia;
- R - renal (kidney) anomaly;
- L - defects in the development of limbs.
Signs of "white" vices
Such anomalies that occur with the enrichment of the pulmonary circulation, for example, a ventricular septal defect, can be suspected immediately after the birth of a child. This:
- heart murmurs and palpitations, which are usually immediately audible to a neonatologist examining a child immediately after birth;
- cyanotic skin tone, especially pronounced in the limbs;
- breathing that is more than normal;
- poor appetite;
- light weight;
- lack of appetite or a weak desire to breastfeed;
- immobility;
- the baby suckles at the breast/pacifier, but gets tired quickly and lets it go.
If the septal defect is small, and all of these signs are mild, then poor weight gain should alert parents. Minor defects may even heal by the age of 10, but treatment should be carried out to reduce pressure in the pulmonary circulation system.
Anomalies of the interatrial septum are also characterized by a violation of the heart rhythm, the appearance of a protrusion of the chest wall in the region of the heart ("heart hump").
For such an anomaly as coarctation of the aorta, a feeling of heaviness and pulsation in the head, hot flashes to the head, dizziness, and shortness of breath are characteristic. Pulsating arteries are visible in the neck. Legs feel numbness, weakness in the legs; they freeze, during exercise there are cramps in the calf muscles.
If with a "white" defect there is no mixing of arterial and venous blood, this is manifested by such signs:
- pain in the region of the heart;
- increased heart rate;
- dizziness, possibly with fainting;
- increased blood pressure;
- dyspnea;
- throbbing pains in the head.
Complications of congenital heart defects
The consequences of heart disease depend on the form of the defect and its severity. The main complications are:
- bacterial endocarditis;
- cardiac insufficiency;
- frequent inflammation of the bronchi and lungs;
- attacks with shortness of breath and blue skin;
- angina;
- myocardial infarction;
- thrombosis of peripheral veins;
- thromboembolism of cerebral vessels;
- rheumatic endocarditis;
- vascular aneurysms or their early atherosclerosis (typical for coarctation of the aorta).
Diagnostics
Some heart defects are detected even during pregnancy - with the help of fetal echocardioscopy. This study is performed at 18-24 weeks of gestation using a transabdominal or transvaginal probe.
Often, congenital heart disease can be suspected after birth - according to the characteristic appearance, fatigue, refusal of the breast. Sometimes the doctor's attention immediately attracts a heart rhythm disturbance, heart murmurs, and expansion of the boundaries of this organ.
If no pathology is detected on examination, the defect can be suspected by a routine electrocardiogram or chest x-ray performed if pneumonia is suspected. Heart disease is confirmed by echocardioscopy with dopplerography (ultrasound of the heart with the determination of blood flow in the cavities and large vessels), but the final diagnosis is made in the cardiocenter according to:
- echocardioscopy of an expert class;
- conducting catheters into the cardiac cavities in order to measure the pressure in them;
- angiocardiography.
Therapy of vices
Treatment of congenital heart defects is divided into medical and surgical. The first type is used for minor defects, as well as at the stages of preparation for the intervention and after it. It is aimed at stabilizing pressure in the pulmonary artery or systemic circulation, improving myocardial trophism and oxygen uptake. internal organs. For this, appoint:
- diuretic drugs;
- potassium salts;
- digitalis preparations;
- antiarrhythmic drugs;
- beta blockers;
- indomethacin - according to the scheme. This is the only radical drug treatment, which can completely solve the problem in the case of an open ductus arteriosus.
Some heart anomalies can stop on their own without surgical treatment, but this usually does not apply to "blue" defects.
Surgery for heart disease takes into account the type and phase of the defect:
- If the cardiac defect is within phase I, up to a year of life, emergency operation. For example, when the small circle is depleted, this is an artificial stenosis of the pulmonary artery, when the small circle is overfilled, it is the imposition of an artificial ductus arteriosus.
- In phase II, planned operation which is carried out after careful preparation, in different times(usually before puberty).
- In case of decompensation, when the defect is detected already in the third phase, only such type of intervention can be carried out that will slightly improve the quality of life of the child.
If a cardiac anomaly was detected before birth, then some types of operations can already be performed in utero. In the case when this is not possible, and the defect is a life-threatening anomaly, the woman is delivered in a specialized hospital, after which the necessary intervention is performed immediately after the birth of the child. For some serious defects, a heart transplant is possible.
Forecast
Congenital heart disease - how long do they live with it? This is based on the shape of the anomaly:
- With a functioning ductus arteriosus, septal anomalies, or stenosis of the pulmonary artery, mortality in the first year of life without treatment is 8-11%.
- Tetralogy (a combination of 4 defects) of Fallot and pathologies of the structure of the myocardium cause a mortality of 24-36% in a child under one year old.
- Coarctation, aortic stenosis, and aortic dextroposition lead to 36-52% mortality in the first year of life. Average duration life is 12 years.
- With left ventricular hypoplasia, pulmonary atresia, common aortic trunk, 73-97% die in the first 12 months of life.
To prevent the formation of cardiac disease as far as possible, even before pregnancy, a woman should be vaccinated against rubella, add to food iodized salt And folic acid. During pregnancy, the mother should not smoke, take alcohol or drugs. At frequent cases heart defects in the family, a woman or a man should consult a geneticist and, possibly, not plan a pregnancy.
Congenital heart disease is an anatomical defect of the heart, its vessels, or valves, which occurs even in utero.
Congenital heart disease in children may not be noticeable, but may appear immediately after birth. On average, this disease occurs in 30% of cases and ranks first among diseases that cause death in newborns and children under one year old. After a year, the mortality rate falls, and at the age of 1-15l. about 5% of children die.
There are seven main types of congenital heart disease in newborns: pathology of the interventricular septum, pathology of the interatrial septum, aortic coarctation, aortic stenosis, patent ductus arteriosus, transposition of the great great vessels, pulmonary stenosis.
Reasons for the appearance
The main causes of birth defects are external influences on the fetus in the 1st trimester of pregnancy. Cause a defect in the development of the heart viral disease maternal (e.g. rubella), radiation exposure, drug exposure, drug addiction, maternal alcoholism.
The health of the child's father also plays an important role, but at the same time genetic factors on the development of congenital heart disease in children play the least role.
There are also such risk factors: toxicosis and the threat of miscarriage in the 1st trimester, the presence in the past of pregnancies ending dead birth a child, the presence of a family history of children with congenital malformations (in the immediate family), endocrine pathologies both spouses, mother's age.
Symptoms of congenital heart disease
Newborns with congenital heart disease have a bluish or blue color of the lips, auricles, skin. Also, blueness in a child may occur when he screams or sucks at the breast. A bluish skin color is characteristic of the so-called "blue heart defects", but there are also "white birth defects", in which the child has blanching of the skin, cold hands and feet.
A murmur is heard in the child's heart. This symptom is not the main one, but if it is present, additional examination should be taken care of.
There are cases when the defect is accompanied by heart failure. The prognosis is unfavorable in most cases.
Anatomical pathologies of the heart can be seen on the ECG, echocardiogram, and x-rays.
If a congenital heart defect is not noticeable immediately after birth, the child may look healthy for the first ten years of life. But after that, a deviation in physical development becomes noticeable, cyanosis or pallor of the skin appears, and shortness of breath appears during physical exertion.
Diagnosis of the disease
The doctor makes the primary diagnosis when examining the child and listening to the heart. If there are reasons to suspect congenital heart disease, the child is sent for further examination. Apply various methods diagnostics, it is also possible to examine the fetus in the womb.
Fetal echocardiography is used to examine a pregnant woman. This ultrasound diagnostics, safe for mother and fetus, allowing to identify pathology and plan the treatment of congenital heart disease.
Echocardiography is another ultrasound examination, but already born child, helps to see the structure of the heart, defects, constricted blood vessels, evaluate the work of the heart.
Electrocardiography is used to assess cardiac conduction, the work of the heart muscle.
Chest X-ray is used to determine heart failure. So you can see excess fluid in the lungs, expansion of the heart.
Another X-ray method detection of congenital heart disease is vascular catheterization. Through femoral artery inject contrast into the bloodstream and make a series x-rays. So you can assess the structure of the heart, determine the level of pressure in its chambers.
To assess the saturation of blood with oxygen, pulse oximetry is used - using a sensor worn on a child's finger, the level of oxygen is recorded.
Treatment of congenital heart disease
The method of treating a defect is chosen depending on its type. So, minimally invasive procedures with catheterization, open surgery, transplantation, and drug therapy are used.
The catheter technique allows the treatment of congenital heart defects without radical surgical intervention. A catheter is inserted through a vein in the thigh, under X-ray control it is brought to the heart, and special thin instruments are brought to the defect site.
 The operation is prescribed if it is not possible to use catheterization. This method is longer and difficult period recovery.
The operation is prescribed if it is not possible to use catheterization. This method is longer and difficult period recovery.
Sometimes surgical treatment of congenital heart defects, mainly in severe cases, is carried out in several stages.
With defects that cannot be treated, a heart transplant is indicated for the child.
Drug therapy is often used to treat adults, older children. With the help of medicines, you can improve cardiac function, ensure normal blood supply.
Disease prevention
Conditionally, the prevention of congenital heart defects is divided into the prevention of their development, the prevention of their unfavorable development and the prevention of complications.
Prevention of the occurrence of a defect lies more in medical genetic counseling at the stage of preparation for pregnancy than to any specific actions. For example, a woman should be warned about the undesirability of pregnancy in a woman whose family (or partner's family) has three or more people with congenital defects. It is not recommended to have children married couple where both partners suffer from this disease. A woman who has had rubella should be carefully examined.
To prevent the unfavorable development of the disease, it is necessary to carry out the necessary diagnostic procedures, to select and carry out the optimal treatment for the correction of the condition. A child with a congenital defect and who has undergone its treatment needs a thorough special care. Often, the mortality of children with congenital malformations under the age of one year is associated with insufficient child care.
To prevent complications of the disease, it is necessary to deal with the prevention of these complications directly.
Due to congenital heart disease, there may be: bacterial endocarditis, polycythemia ("blood clotting"), causing thrombosis, headaches, inflammation of the peripheral vessels, thromboembolism of cerebral vessels, respiratory diseases, complications from lungs and their vessels.
Video from YouTube on the topic of the article:
From the very beginning of pregnancy, future parents are relentlessly haunted by the thought: “If only the child was born healthy!”. Indeed, hardly anything can disturb and frighten more than childhood illnesses. And when it comes to such a formidable diagnosis as birth defect hearts of children, many fall into despair.
In fact, you should not give up: when timely diagnosis and properly conducted treatment, it is quite possible to save a child from a serious illness.
The phrase "congenital heart disease" is already terrifying in itself, and the mysterious abbreviations that the doctor writes on the children's card can, in this case, bring parents to panic. However, you should calm down and find out which violations are characterized by the letter combination of UPU.
The heart is one of the most important organs human, and its task is to ensure proper blood flow and, as a result, saturate the entire body with vital oxygen and nutrients. Due to the contraction of the heart muscles, venous blood saturated with carbon dioxide enters the lower chambers of the heart - the atria. Passing into the ventricles - the upper chambers of the heart, the blood is again enriched with oxygen and sent to the main arteries, through which it is delivered to organs and tissues, giving them everything useful material and taking away carbon dioxide and metabolic products. Then the blood passes through the veins and again enters the atrium. The passage of blood from the chambers and its uniform and timely exit into the arteries is regulated by muscular valves.
Blood circulation in the body occurs in two directions. The systemic circulation originates in the left atrium and ends in the right ventricle. Through this vascular pathway, the vital activity of all tissues and organs is maintained. However, the heart constantly needs oxygen, so the pulmonary circulation connects it only with the lungs, starting from the right atrium, passing through pulmonary arteries and returning to the left ventricle.
It is obvious that the heart and blood vessels are a clear, flawlessly debugged system, where insignificant details simply do not exist. The slightest error in the work of any of the components of the body can cause disturbances in the body as a whole, and in especially serious cases - even lead to lethal outcome. Therefore, malfunctioning heart chambers, valves that do not open in time, or affected large vessels and are classified as heart defects.
According to statistics, for every thousand healthy babies, there are 6-8 children with heart pathologies. Congenital heart disease in newborns is the second most common disease of cardio-vascular system.
Most often, the occurrence of pathologies of the heart and blood vessels is caused by the following reasons.
- Infectious diseases in early pregnancy. Such diseases are especially dangerous in the first trimester, between 3 and 8 weeks of pregnancy, when the heart and blood vessels of the child are formed. by the most insidious disease is rubella, which causes severe damage to the fetus.
- The age and health of the mother. With age defensive forces body gradually weaken, and during pregnancy, the endocrine and immune system are rebuilt in such a way as to maintain the health of a woman as much as possible, even to the detriment of the unborn child. Therefore, the older future mom and the more chronic diseases she has, the higher the risk of improper formation of the baby's cardiovascular system.
- non-compliance healthy lifestyle life during pregnancy - smoking, drug use, alcoholic beverages, uncontrolled intake of medications or work in hazardous production negatively affect the body, and first of all, the work of the heart.
- Heredity. Unfortunately, the tendency to heart pathologies can be transmitted at the genetic level. And if among relatives on the maternal or paternal side someone was diagnosed with a congenital heart disease, then it is necessary to monitor the pregnancy very closely, since the risk of the disease is extremely high.
No one can give a 100% guarantee that a child will not develop a heart disease. However future mother able to minimize this risk. Proper nutrition, rejection bad habits, strengthening immunity and careful planning of pregnancy will ensure normal development And correct formation all organs of the future baby.
How pathology manifests itself
Often, after the detection of cardiac pathologies in a child, parents are frightened not so much by the diagnosis itself, but by the lack of necessary information. The wording used by doctors often not only fails to clarify the situation, but inspires even more fear. Therefore, it is important to have a rough idea of what is meant by this or that diagnosis.
In total, about a hundred varieties of congenital heart defects are classified, but the following pathologies are most common.
- Hypoplasia - insufficient development of one of the ventricles. With such a violation, only part of the heart works effectively. It is not very common, but it is one of the most serious vices.
- Transposition of the great vessels (TMS) is an extremely severe heart disease, which is characterized by a mirror arrangement of the arteries. In this case, the process of enriching the blood with oxygen is disturbed.
- obstruction defects. Connected with wrong formation holes in vessels. Most often, in children with heart disease, stenosis (abnormal narrowing of blood vessels or heart valves) and atresia (partial overgrowth of the lumen of blood vessels) are determined. Especially dangerous is coarctation of the aorta - narrowing of the largest blood vessel in organism.
- Atrial septal defect (ASD) is a violation of the development of tissues between the chambers of the heart, as a result of which blood moves from one atrium to another, and the stability of blood circulation is disturbed.
- Ventricular septal defect (VSD) is the most common heart defect. It is characterized by underdevelopment of the tissue wall between the right and left ventricles, which leads to incorrect blood circulation.
Often, heart defects are combined with each other, therefore, when making a diagnosis, it is required to indicate all lesions of the heart and blood vessels. Hence the possible numerous abbreviations in children's cards that scare parents so much.

Circulatory disorders primarily affect the color of the skin. Based on this, heart defects are divided into two groups: pale and blue.
Pale, or white defects - abnormal vasoconstriction, defects in the partitions between the heart chambers. Arterial and venous blood do not mix. In children with such pathologies, unhealthy pallor of the skin is observed. Blue heart defects include transposition of the great vessels and tetralogy of Fallot (complex heart disease with vasoconstriction, septal defect and underdevelopment of one of the ventricles). With such disorders, the autonomy of all heart chambers is impaired, as a result of which arterial and venous blood is mixed. Because of this, the skin acquires a bluish or grayish tint, which is especially noticeable on the skin of the extremities and in the region of the nasolabial triangle.
In addition to an unhealthy skin tone, there are the following symptoms birth defect hearts in newborns
- severe shortness of breath;
- cardiopalmus;
- fast fatiguability;
- poor appetite, slow set weight, frequent regurgitation;
- heart murmurs when heard with a stethoscope.
Each of these symptoms individually does not yet indicate the presence of heart disease. However, the presence of more than two unfavorable signs requires immediate appeal to specialists, since any heart disease leads to serious complications. If slight disturbances in the functioning of the heart and blood vessels can lead to a slow development of the child, frequent fainting and dizziness, reduced immunity, then more severe ones at any time can lead to acute heart failure and lethal outcome. Therefore, if there is a suspicion that something is not right with the child’s heart, you should not wait: in this case, every second counts, and the examination should be carried out as soon as possible. Heart disease is especially dangerous because in the first year of life it may not manifest itself in any way. That is why ultrasound of the heart at the age of 6-9 months is included in the list of mandatory examinations for children of the first year of life.
Treatment of congenital heart disease in children
The choice of treatment for congenital heart disease in newborns depends on the results of the examination. Diagnosis of disorders in the work of the heart includes the following procedures:
- electrocardiogram - detection of cardiac arrhythmias;
- radiography of the heart - the study of vascular patency;
- ultrasound examination - detection of abnormalities in the structure of the heart;
- echocardiogram - study of the functioning of the heart;
- dopplerometry - the study of the characteristics of blood flow.
If, as a result, the child is diagnosed with a heart disease, the question of surgical intervention is raised. However, the decision on the operation can only be made by specialists - a cardiologist and a cardiac surgeon, so contacting them in a short time can save the baby's life.

In some cases, the operation may be delayed. If the blood supply to the tissues and lungs is slightly impaired and serious threat for the life of a child this moment not identified, the operation is performed at an older age, when the patient gets stronger. There are times when surgery is questionable. for a long time: sometimes the pathology corrects itself. This is especially true for the so-called oval window - an additional duct that does not close at birth for some reason. Such cases require regular monitoring by a cardiologist. However, in no case can one hope that everything will go away on its own - constant consultations with a doctor and strict implementation of all his recommendations are vital.
For severe heart defects, surgery can be performed as early as infancy. The type of intervention depends on the type of pathology. This may be a ligation or intersection of the vessel (with open ductus arteriosus), patching and plasty of the tissues of the septum between the heart chambers, catheterization to expand narrowed vessels, removal of a section of the aorta, relocation of vessels (during transposition), transplantation of heart valves and installation of a homograft (vascular prosthesis). IN difficult cases more than one operation with a break from several months to a year may be required.
In the treatment of heart disease postoperative period no less important than the operation itself. The child is prescribed painkillers and drugs to improve cardiac activity, as well as all necessary procedures. Regardless of age little patient before and after the operation, careful care and strict adherence to all medical prescriptions will be necessary.
It is necessary to take care of the health of the unborn baby even before pregnancy. Right image life and the exclusion of environmental influences dangerous for expectant mothers will increase the chances of giving birth healthy child. However, it is impossible to completely insure against diseases, unfortunately.
Methods modern diagnostics stepped far ahead. Therefore, it is possible to identify violations in the formation of the cardiovascular system even before the birth of a child. Already at the beginning of the second trimester, it is possible to determine the presence or absence of cardiac pathologies according to the results ultrasound. Regularly passing all the necessary examinations will help to identify deviations in the development of the baby as early as possible.
If no pathologies were detected on ultrasound, this is not a reason to lose vigilance, because the signs incorrect operation hearts may appear later. Even if the child is not worried about anything, doctors recommend doing an ultrasound of the heart in infancy when the baby is able to sit up.
In the case when a heart defect was nevertheless detected, there is no reason to panic: it is necessary to go through all necessary examinations and contact the experts as soon as possible. In no case should you hope for a chance: congenital heart disease is an insidious and unpredictable disease.
![]()
If surgery has been delayed, the cardiologist will provide lifestyle advice and possibly prescribe medication. All instructions must be strictly followed and the slightest sign malaise consult a doctor.
Heart surgery is often performed when the child is at a conscious age. During this period, the attention and care of parents is more important than ever for the baby. If even adults are afraid of surgery, what can we say about children, for whom it seems like a catastrophe. That's why psychological preparation child for surgery is necessary in any case.
You can tell your son or daughter about the benefits of surgery, about how doctors will help the heart work better, and even about the fact that he will soon be able to run and play sports like other children. The main thing is to feel confident: the child will sensitively catch any nervousness and begin to worry himself.
After operation if possible, you should always be nearby: the love of parents is vital for a baby tired of pain and fear. It is necessary to praise the child for perseverance and patience and emphasize in every possible way that the pain will pass, the droppers will be removed, the bandages will be removed, and soon he will feel much better. It is better to forget about pedagogy: in such a situation, any whims are allowed for children, unless, of course, they contradict the treatment regimen.
Congenital heart disease in a child today is no longer something catastrophic. Medicine is moving forward by leaps and bounds, new and effective methods treatments allow you to get rid of the disease completely. The main thing is the sensitivity and attention of parents to the health and well-being of the child. Only then will the baby be able to forget about all the ailments and live a full life.
Informative video on the topic
I like!

