Recovery of fat metabolism. Violation of fat metabolism, treatment, symptoms, folk remedies
Lipid metabolism disorders can occur as a result of violations: 1) absorption of fat in the intestine; 2) the transition of fat from the blood into the tissue; 3) deposition of fat: 4) interstitial fat metabolism.
§ 198 Fat malabsorption
For absorption of dietary fat from the intestine, it must be emulsified, broken down into glycerol and fatty acid and the formation of complex compounds with bile acids - choleinates. Therefore, the cessation of bile secretion in duodenum or a decrease in its secretion is immediately reflected in the digestion of fats. Blockage of the bile duct, inflammation of the gallbladder (cholecystitis) and some liver diseases associated with a violation of the bile secretion process cause non-emulsified fats to pass through the alimentary canal, being exposed only to a small extent. to a large extent hydrolysis. If the hydrolysis of dietary fats in this case is carried out sufficiently under the action of lipases of pancreatic and intestinal juices, then the resulting fatty acids are still not absorbed. The same happens with a decrease or complete cessation of the secretion of pancreatic enzymes, with a decrease in the function of the intestinal epithelium and with significantly increased peristalsis small intestine when the fat does not have time to be absorbed. This kind of fat absorption disorders are observed in enteritis, hypovitaminosis A and B, due to a violation of the formation of enzymes involved in the resynthesis of triglycerides in the intestinal epithelium.
The secretion of fat occurs mainly through the intestines and to a lesser extent is carried out by sebaceous and sweat glands. Only traces of fat are found in the urine. With impaired absorption of fat, feces contain a lot of undigested fat and higher fatty acids and have a characteristic grayish-white color - steatorrhea. Excretion of fat in the urine - lipuria - can occur after ingestion of very large amounts of fat with food, with fractures of tubular bones, accompanied by crushing bone marrow, trauma to large areas of adipose tissue, with lipoid nephrosis.
Excess secretion of fat sebaceous glands- seborrhea - occurs in some skin diseases - acne, eczema, beriberi, etc.
Consequences of malabsorption of fat- although fats and lipoids are easily synthesized in the body from intermediate products of carbohydrate metabolism, the complete exclusion of fats from food is unacceptable. With fats, vital fat-soluble vitamins (A, D, E, K) are introduced into the body, and therefore, with insufficient intake of fats with food, hypovitaminosis can develop in humans and animals. In addition, the composition of natural fats always includes a small amount of essential unsaturated higher fatty acids (for example, linoleic-C 18 H 32 O 2 and linolenic - C 18 H 30 O 2), which cannot be synthesized in the body from other fatty acids. In the absence of them in food, animals in the experiment develop chronic diseases skin (in the form of necrotic foci). Apparently complete absence unsaturated higher fatty acids in human food can also be the cause of more or less serious disorders exchange.
§ 199. Violation of the transition of fat from blood to tissue
Neutral fat from the gut circulates in the blood as chylomicrons (consisting of triglycerides, cholesterol esters, phospholipids, and β-lipoprotein) and α-lipoproteins. Normally, the content of neutral fats in the blood is 1-2 g / l.
A temporary transient increase in the content of chylomicrons in the blood - hyperlipemia - is observed with an increased intake of fat from food ( alimentary hyperlipemia). Hyperlipemia may be the result of increased mobilization of fat from the depot - transport hyperlipemia(Fig. 35).
Many hormones contribute to the mobilization of fat from fat depots, lungs, and bone marrow. For example, during starvation, the release of fat from its depot occurs as a result of the combined action of the growth hormone of the pituitary gland, pancreatic glucagon and adrenaline. The action of these hormones on adipose tissue is realized through the adenyl cyclase - tAMP system. The latter increases the activity of triglyceride lipase, which carries out lipolysis in tissues.
The mobilization of fat from the lungs, leading to hyperlipemia, occurs predominantly with prolonged hyperventilation of the lungs, for example, in professional singers.
Retention hyperlipemia(retentio - delay) - the result of a delay in the transition of neutral fats from the blood to the tissues, occurs mainly with a decrease in the blood content of albumin and the clarification factor (AF), specific lipoprotein lipase. Under the action of FP, the triglycerides associated with proteins are cleaved and thus the "enlightenment" of lipemic serum occurs. The resulting free fatty acids are bound by albumin (1 molecule of albumin binds 6-7 molecules of fatty acids), which contributes to the transition of fat into cells. Therefore, a lack of albumin in the blood (for example, during starvation, kidney disease - nephrosis) leads to hyperlipemia, as well as an insufficient content of FP and heparin. For example, in atherosclerosis, hyperlipemia depends on a decrease in heparin and low lipoprotein lipase (LP) activity. In diabetes, the decrease in AF in the blood depends on the lack of lipocaine.
§ 200. Excessive accumulation of fat in adipose tissue
Obesity is the result of dysregulation of fat entry into adipose tissue, its formation and utilization as an energy source.
One of the significant causes of obesity is excessive (in relation to energy costs) food intake associated with increased appetite. The latter is due to the increased excitability of the food center, in particular nerve formations hypothalamic region. It has been experimentally established that irritation of the ventro-lateral nuclei of the hypothalamus and destruction of the ventro-medial nuclei cause a lack of satiety, increased appetite, hyperphagia, followed by fat deposition (the so-called hypothalamic obesity).
The clinical analogue of this kind of obesity is diencephalic obesity, which develops as a result of infectious and toxic damage to nerve formations in the interstitial brain, as well as with tumors in this area.
A decrease in the release of fat from its depot occurs when the function is suppressed. thyroid gland and the pituitary gland, whose hormones (thyroxine, growth hormone, TSH) activate the mobilization of fat and its subsequent oxidation. Increased production of pituitary ACTH, adrenal glucocorticoids and insulin contributes to the deposition of fat and its formation from carbohydrates. A decrease in the function of the gonads leads to excessive deposition of fat if it is accompanied by a violation of the activity of the hypothalamic centers (see §§ 337, 338).
§ 201. Fatty infiltration of the liver
If the fat brought by the blood to the cells is not subjected to splitting and oxidation in them, it is not excreted and long time stays in the cells fatty infiltration(impregnation). Its combination with a violation of the protoplasmic structure is called fatty degeneration.
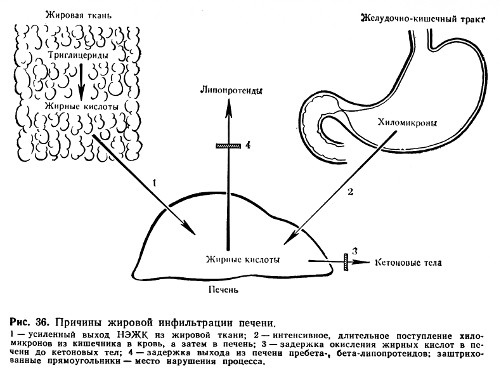
A common cause of fatty infiltration and dystrophy is the suppression of the activity of hydrolytic and oxidative enzymes of fat metabolism (Fig. 36), which can be observed in case of poisoning with phosphorus, arsenic, chloroform, viral infections, beriberi (alcoholism).
Great importance in the pathogenesis of fatty infiltration of the liver is given to a violation of the formation of phospholipids. Their sufficient content in the liver ensures fine dispersion of fat and thus its release from the cell. In the phospholipid molecule catalyzes the oxidation of fatty acids. Insufficient formation of phospholipids occurs when there is a deficiency in the body of choline, the structural part of the main phospholipid of the liver - lecithin. And the synthesis of choline, in turn, is associated with methyl groups, the donor of which is the amino acid methionine. Therefore, insufficient introduction of dietary choline into the body or insufficient formation of it due to a lack of methionine can lead to fatty infiltration of the liver. Methionine, as well as casein protein, which includes a large number of methionine, has a lipotropic effect, i.e., it helps to remove excess fat from the liver. The endogenous lipotropic factor - lipocaine (formed in the epithelium of the small ducts of the pancreas) has the same property. The lack of lipocaine in diabetes mellitus contributes to fatty infiltration of the liver.
§ 202. Violation of the intermediate metabolism of fat
Relatively stable products of the intermediate metabolism of higher fatty acids are acetone, acetoacetic and beta-hydroxybutyric acids, the so-called ketone or acetone bodies, formed mainly in the liver and oxidized to CO 2 and H 2 O in other tissues and organs (muscles, lungs, kidneys and etc.). In some pathological processes and diseases (diabetes mellitus, starvation - complete or exclusively carbohydrate, long-term infections with high temperature, hypoxia, diseases of the liver parenchyma, etc.), the content of acetone bodies in the blood can rise sharply (normally, their content does not exceed 0.02-0.04 g / l) (2-4 mg%). Acetonemia leads to the appearance of ketone and acetone bodies in the urine - aceturia. Acetone is excreted not only through the kidneys, but also through the lungs with exhaled gases and sweat. The patient smells like acetone.
Mechanisms leading to an increase ketone bodies in the blood (ketosis), are quite complex.
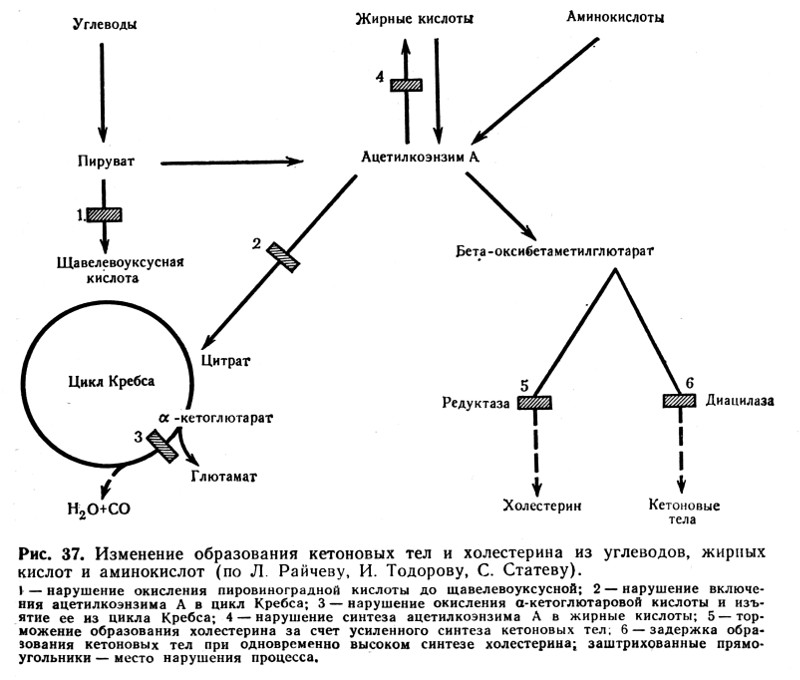
- One of the main reasons for the development of ketosis is a deficiency of carbohydrates (for example, in diabetes mellitus, starvation), which leads to depletion of the liver in glycogen and an increased intake of fat into it, where fatty acids are oxidized to acetoacetic acid. This is also facilitated by insufficient resynthesis of higher fatty acids from ketone bodies and a violation of their oxidation in the tricarboxylic (citric) cycle. Resynthesis requires the energy of glycolysis. Insufficient oxidation of ketone bodies is also associated with a deficiency of compounds formed during the intermediate metabolism of carbohydrates (pyruvic and oxaloacetic acids) and which are substrates of the tricarboxylic acid cycle (Fig. 37).
- An important pathogenetic link in the development of ketosis in diabetes mellitus is the simultaneous deficiency of lipocaine and insulin.
- With liver damage caused by toxin-infectious factors, the glycogen-forming function of the liver is impaired, which contributes to the transition of fatty acids to the liver. Here, the formation of ketone bodies largely prevails over their oxidation. The result is ketosis and fatty liver.
§ 203. Violation of the metabolism of phospholipids
Disturbances in the metabolism of phospholipids (lecithins, cephalins) are closely related to fat metabolism. So with lipemia, the level of lecithin in the blood rises.
Some hereditary pathological conditions associated with excessive deposition of phospholipids in tissues are known. For example, in Gaucher disease, cerebrosides are deposited in macrophage cells of the spleen, liver, lymph nodes and bone marrow. With Niemann-Pick disease in cells various bodies deposition of sphingomyelin phosphatide is observed. Amavrotic (from the Greek amauros - dark, blind) family idiocy is the result of the deposition of lipoids in nerve cells, which is accompanied by atrophy of the optic nerves and dementia.
§ 204. Cholesterol metabolism disorders. Atherosclerosis
Disorders of cholesterol metabolism underlie the development of atherosclerosis, cholelithiasis, lipoid nephrosis, age-related clouding of the cornea, xanthomatosis of the skin, bones and other diseases.
The Russian pathophysiologists N. P. Anichkov and S. S. Khalatov played an important role in the study of disorders of cholesterol metabolism. Back in 1911-1912. they created an experimental model of atherosclerosis by feeding cholesterol to animals. Although in the pathogenesis of human atherosclerosis the significance of exogenous (dietary) cholesterol is not so significant, but the fact that cholesterol metabolism is disturbed is beyond doubt.
Under physiological conditions, the cholesterol content in the blood of an adult is about 1.8-2.3 g / l. Some increase in blood cholesterol levels can occur after eating cholesterol-rich foods ( egg yolk, brain, liver, butter etc.), but this alimentary hypercholesterolemia in humans is rapidly passing, because with an excess of cholesterol from mast cells heparin is released into the blood, activating lipoprotein lipase, the so-called "enlightenment factor" (AF). The latter converts large molecular lipids with low density into finely dispersed, easily removed from the blood.
Changes in cholesterol metabolism may be the result of impaired cholesterol synthesis, leading to endogenous hypercholesterolemia. Cholesterol synthesis is regulated primarily by its intake from the intestine: a small intake activates cholesterol synthesis. The starting material for the synthesis of cholesterol are, in addition to acetoacetic acid, the amino acids valine and leucine, fatty acids, carbohydrates, which in the process of intermediary metabolism are converted into acetylcoenzyme A. The latter is included in the beta-hydroxy-beta-methyl-glutarylcoenzyme A cycle and contributes to the development of hypercholesterolemia.
An important factor in cholesterol metabolism is the activity of tissue enzymes that ensure the breakdown of lipids. So, it has been proven that pathological conditions predisposing to atherosclerosis (diabetes, stress, hypoxia), the lipolytic activity of the aortic wall is significantly reduced, and the cholesterol content in it increases sharply. The wall of the aorta of healthy people contains 5-50 mg of cholesterol, in the atheromatous aorta - 240 mg, with severe forms atheromatosis cholesterol content in the aorta can reach 500-1000 mg.
The cause of hypercholesterolemia can also be a change in the physicochemical state of blood proteins, due to which a stronger bond between cholesterol and β-lipoproteins is formed and release from the cholesterol complex is difficult, or, conversely, the β-protein complex breaks and the dispersion of cholesterol micelles decreases. In both cases, cholesterol is retained in the blood.
In violation of cholesterol metabolism, loss of function of the thyroid, sex glands, and adrenal glands is important. Which links of cholesterol metabolism are changed by each of these hormones is a very complicated question. They can change the rate of cholesterol transfer into and out of the cell, affect the distribution of its fractions between blood plasma and interstitial fluid, and the processes of cholesterol synthesis and breakdown.
The most important manifestation of impaired cholesterol metabolism in the human body is atherosclerosis.
Lipids- inhomogeneous chemical composition organic matter, insoluble in water, but soluble in non-polar solvents.
Typical forms of lipid metabolism pathology are obesity, malnutrition, lipodystrophy, lipidosis and dyslipoproteinemia.
Obesity
Obesity- excess accumulation lipids in the body in the form of triglycerides.
TYPES OF OBESITY
Depending on the degree of weight gain There are three degrees of obesity.
Various formulas are used to estimate the optimal body weight.
♦ The simplest is Broca's index: 100 is subtracted from the growth rate (in cm).
♦ Body mass index (BMI) is also calculated using the following formula:
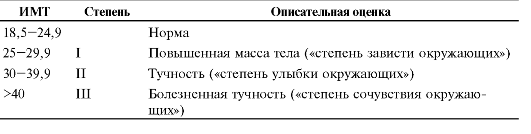
Depending on the value of the body mass index, one speaks of normal or overweight of 3 degrees (Table 10-1).
According to the predominant localization of adipose tissue There are general (uniform) and local (local lipohypertrophy) obesity. There are two types of local obesity.
♦ female type(gynoid) - excess subcutaneous fat mainly in the thighs and buttocks.
Table 10-1. Degrees of obesity
 ♦ male type(android or abdominal) - the accumulation of fat mainly in the abdomen.
♦ male type(android or abdominal) - the accumulation of fat mainly in the abdomen.
By genesis distinguish primary obesity and its secondary forms.
♦ Primary (hypothalamic) obesity is an independent disease of neuroendocrine origin, caused by a disorder in the fat metabolism regulation system.
♦ Secondary (symptomatic) obesity - a consequence various violations in the body, causing a decrease in lipolysis and activation of lipogenesis (for example, in diabetes, hypothyroidism, hypercortisolism).
ETIOLOGY
The cause of primary obesity is a malfunction of the hypothalamus-adipocyte system.
Secondary obesity develops with excess calorie content of food and reduced level energy consumption of the body (mainly with hypodynamia).
OBESITY PATHOGENESIS
Allocate neurogenic, endocrine and metabolic mechanisms of obesity.
Neurogenic variants of obesity
Centrogenic(cortical, psychogenic) mechanism - one of the variants of eating disorders (two others: anorexia nervosa and bulimia).
♦ Reason: various mental disorders, manifested by a constant, sometimes irresistible desire to eat.
♦ Possible mechanisms:
❖ activation of serotonergic, opioidergic and other systems involved in the formation of feelings of pleasure and comfort;
❖ perception of food as a strong positive stimulus (doping), which activates these systems even more. it
closes the vicious circle of the centrogenic mechanism of obesity development.
hypothalamic(diencephalic, subcortical) mechanism.
♦ Cause: damage to hypothalamic neurons (for example, after a concussion, with encephalitis, craniopharyngioma, tumor metastases in the hypothalamus).
♦ The most important links of pathogenesis:
❖ Damage or irritation of neurons in the posterolateral ventral nucleus of the hypothalamus stimulates the synthesis and secretion of neuropeptide Y and reduces sensitivity to leptin, which inhibits the synthesis of neuropeptide Y. Neuropeptide Y stimulates hunger and increases appetite.
❖ Violation of the formation of hunger due to excessive production of neurotransmitters that form a feeling of hunger and increase appetite (GABA, dopamine, β-endorphin, enkephalins). This leads to a decrease in the synthesis of neurotransmitters that form a feeling of satiety and inhibit eating behavior (serotonin, norepinephrine, cholecystokinin, somatostatin).
Endocrine variants of obesity
Endocrine mechanisms of obesity - leptin, hypothyroid, adrenal and insulin.
Leptin mechanism- Leading in the development of primary obesity.
♦ Leptin formed in fat cells. It reduces appetite and increases energy consumption by the body. Leptin inhibits the production and release of neuropeptide Y by the hypothalamus.
♦ Neuropeptide Y participates in the formation of hunger. It increases appetite and reduces energy consumption of the body.
♦ Lipostat. The "leptin-neuropeptide Y" circuit maintains the mass of adipose tissue of the body with the participation of insulin, catecholamines, serotonin, cholecystokinin, endorphins. In general, this system of biologically active substances, which provide dynamic homeostasis of energy metabolism and the mass of adipose tissue in the body, was called the lipostat system.
Hypothyroid mechanism obesity is activated when the effects of iodine-containing thyroid hormones are insufficient, which reduces the intensity of lipolysis, the rate of metabolic processes in tissues and the body's energy costs.
Adrenal(glucocorticoid, cortisol) mechanism obesity is switched on due to hyperproduction of glucocorticoids in the adrenal cortex (for example, in case of illness and syndrome
Itsenko-Cushing), which promotes lipogenesis due to hyperglycemia and the inclusion of the insulin mechanism.
insulin mechanism The development of obesity develops due to direct activation of lipogenesis by insulin in adipose tissue.
Metabolic mechanisms of obesity. The reserves of carbohydrates in the body are relatively small. In this regard, a mechanism for saving carbohydrates has been developed: with an increase in the proportion of fats in the diet, the rate of carbohydrate oxidation decreases. When the regulatory system is disturbed, a mechanism is activated that provides an increase in appetite and an increase in food intake. Under these conditions, fats do not undergo splitting and accumulate in the form of triglycerides.
exhaustion
exhaustion- pathological decline fat mass, as well as muscle and connective tissue below the norm. extreme exhaustion is cachexia.
With exhaustion, the deficit of adipose tissue is more than 20-25%, and with cachexia - more than 50%. BMI at depletion less than 19.5 kg/m 2 .
ETIOLOGY
Depletion can be caused by endogenous and exogenous causes.
Exogenous causes:
♦ Forced or conscious complete or partial starvation.
♦ Insufficient calorie content of food.
Endogenous causes of depletion are divided into primary and secondary.
♦ Cause of primary depletion: suppression of the synthesis of neuropeptide Y in the hypothalamus (in case of trauma or ischemia of the hypothalamus, severe prolonged stress) and hyposensitization of target cells to neuropeptide Y.
♦ Causes of secondary (symptomatic) depletion: malabsorption, glucocorticoid deficiency, hypoinsulinism, increased synthesis of glucagon and somatostatin, hyperproduction of TNFα by tumor cells.
PATHOGENESIS
Exogenous wasting and cachexia. The absence or significant shortage of food products leads to depletion of the fat supply, disruption of all types of metabolism, insufficiency of biological oxidation and suppression of plastic processes.
Primary endogenous forms of malnutrition
Greatest clinical significance have hypothalamic, cachectic and anorexic forms.
In the hypothalamic (diencephalic, subcortical) form of exhaustion and cachexia, there is a decrease or cessation of the synthesis and release of peptide Y into the blood by hypothalamic neurons, which disrupts the lipostat.
In the case of cachectic (or cytokine) depletion, the synthesis of TNF-α (cachectin) by adipocytes and macrophages leads to suppression of the synthesis of neuropeptide Y in the hypothalamus, inhibition of lipogenesis and activation of lipid catabolism.
anorexic form.
♦ In individuals with a predisposition to anorexia, a critical attitude to their body weight (perceived as excessive) leads to the development of neuropsychiatric disorders and long periods refusal to eat. Most often observed in adolescent girls and girls under 18 years of age.
♦ The further course of the process is associated with a decrease in the synthesis of neuropeptide Y and a significant decrease in body weight, up to cachexia.
Secondary endogenous forms exhaustion and cachexia are symptoms of other forms of pathology: malabsorption syndromes, growth of neoplasms (synthesizing TNFa), hypoinsulinism, hypocorticism, lack of effects of thymus hormones.
Lipodystrophy and lipidosis
Lipodystrophy- conditions characterized by a generalized or local loss of adipose tissue, less often by its excessive accumulation in the subcutaneous tissue.
Lipidoses- conditions characterized by disorders of lipid metabolism in cells (parenchymal lipidosis), adipose tissue (obesity, malnutrition) or walls arterial vessels(for example, atherosclerosis).
Dyslipoproteinemia
Dyslipoproteinemia- conditions characterized by a deviation from the norm of the content, structure and ratio of various drugs in the blood.
The nature of the flow and clinical manifestations dyslipoproteinemias are defined:
♦ genetic features organism (for example, the composition, ratio and level of various drugs);
♦ factors external environment(for example, a set of food products, features of the diet and mode of eating);
♦ availability concomitant diseases(eg, obesity, hypothyroidism, diabetes, kidney and liver disease).
Atherogenicity of lipoproteins
LP are divided into atherogenic (VLDL, LDL and LPPP) and anti-atherogenic (HDL).
The assessment of the potential atherogenicity of blood LP is carried out by calculating the cholesterol coefficient of atherogenicity:
total cholesterol - HDL cholesterol
HDL cholesterol
Normally, the cholesterol coefficient of atherogenicity does not exceed 3.0. With an increase in this value, the risk of developing atherosclerosis increases.
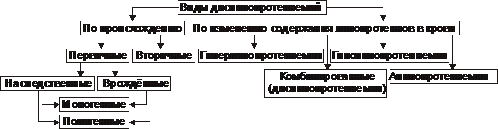
TYPES OF DISLIPOPROTEINEMIA
By origin: primary (hereditary; they can be monogenic and polygenic) and secondary.
By changing the content of lipoproteins in the blood: hyperlipoproteinemia, hypo- and alipoproteinemia, combined dyslipoproteinemia.
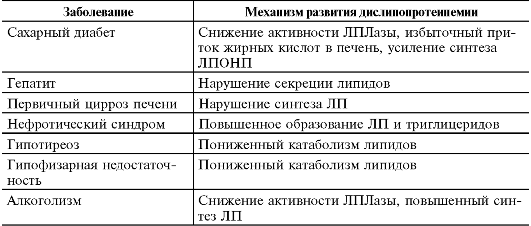
Various, as a rule, chronic diseases can lead to the development of secondary dyslipoproteinemias (Table 10-2).
Table 10-2. Diseases leading to the development of secondary dyslipoproteinemias
 Hyperlipoproteinemia
Hyperlipoproteinemia
Hyperlipoproteinemia- conditions that are manifested by a persistent increase in the content of LP in the blood plasma.
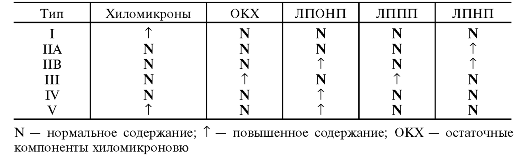
In 1967, Fredrickson et al. developed a classification of hyperlipoproteinemias. Later, this classification was revised by WHO experts (Table 10-3).
Table 10-3. Types of hyperlipoproteinemias and the content of various lipoproteins in them
 Hypolipoproteinemia
Hypolipoproteinemia
Hypolipoproteinemia- conditions that are manifested by a persistent decrease in the level of LP in the blood plasma up to their complete absence (alipoproteinemia).
Combined dyslipoproteinemias characterized by a violation of the ratio of various fractions of LP.
Atherosclerosis
Atherosclerosis- a chronic pathological process leading to changes mainly in the inner lining of the arteries of the elastic and muscular-elastic types due to the accumulation of excess lipids, the formation fibrous tissue, as well as a complex of other changes in them.
The most commonly affected arteries in atherosclerosis are the coronary, carotid, renal, mesenteric, lower extremities and the abdominal aorta.
ETIOLOGY
The reasons atherosclerosis has not been fully elucidated. There are three hypotheses explaining the occurrence of atherosclerosis: lipid, chronic endothelial injury, and monoclonal.
Risk factors. At least 250 factors are known to contribute to the emergence and development of atherosclerosis. The most significant risk factors include smoking, diabetes, arterial hypertension, obesity, autoimmune diseases, hypercholesterolemia, hypertriglyceridemia, hyperhomocysteinemia, hypodynamia, hereditary predisposition, oral contraceptives.
PATHOGENESIS
Allocate next steps atherosclerotic vascular lesions: lipid spots and stripes, the formation of atheroma and fibroatheroma, the development of complications (Fig. 10-1).
Lipid spots and stripes
Intact endothelium prevents the penetration of LP into the intima of the arteries. Under the influence of risk factors, endothelial cells are damaged, and endothelial dysfunction- trigger factor atherogenesis.
The formation of lipid spots and stripes proceeds in several stages:
♦ Migration to arterial intima areas with damaged endothelial cells a large number monocytes and T-lymphocytes.
♦ Synthesis of biologically active substances (chemotaxis factors, kinins, Pg, TNFa) and reactive oxygen species by leukocytes, which is accompanied by intensification of SPO. These factors potentiate damage to the endothelium and the penetration of LP into the vascular intima.
♦ Additional activation of peroxidation of LDL penetrating into the subendothelial layer with the formation of modified lipoproteins.
♦ Uptake of modified drugs by monocytes with the help of "scavenger receptors" (cleaner receptors) and their transformation into foam cells macrophages rich in lipids.
♦ Activation of T-lymphocytes and macrophages in the focus of damage to the artery wall with the development of aseptic inflammation.
♦ Proliferation of SMCs and fibroblasts and their synthesis of connective tissue components with the formation of lipid spots and stripes in the intima.
Formation of atheroma and fibroatheroma
The formation of atherosclerotic plaque is due to several factors:
Further damage to the endothelium mediators of inflammation, which potentiates the penetration of LDL into the intima of the vessels and the closure of the vicious circle.
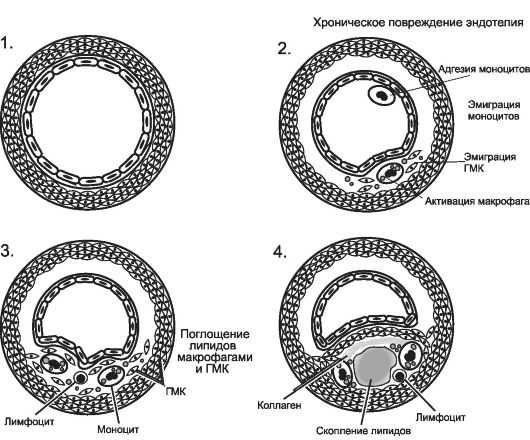 Rice. 10-1.
Successive changes in the damaged arterial wall in atherosclerosis. 1 - normal wall of the artery; 2 - adhesion of monocytes and platelets to the damaged endothelium; 3 - migration of monocytes and SMCs into the intima, lipid infiltration; 4 - proliferation of cellular elements, the formation of a lipid core and the formation of fibroatheroma. [on 4].
Rice. 10-1.
Successive changes in the damaged arterial wall in atherosclerosis. 1 - normal wall of the artery; 2 - adhesion of monocytes and platelets to the damaged endothelium; 3 - migration of monocytes and SMCs into the intima, lipid infiltration; 4 - proliferation of cellular elements, the formation of a lipid core and the formation of fibroatheroma. [on 4].
Transformation GMC into macrophage-like and activation of the synthesis by them and fibroblasts of the components of the intercellular substance of the connective tissue (proteoglycans, glycosaminoglycans, collagen and elastic fibers).
Formation of the lipid core atheroma due to the death of foam cells and the release of free lipids from them.
♦ Atheroma characterized by the presence of a significant number of cellular elements: foam cells, SMC on different stages proliferation and transformation, lymphocytes, granulocytes, platelets; the formation of a lipid core with a large amount of free cholesterol and its esters.
♦ fibroatheroma characterized by the formation of a fibrous cap over the lipid core due to the synthesis of connective tissue components and the development of a network of newly formed vessels penetrating the plaque.
Development of complications of atherosclerosis
Modification atherosclerotic plaques leads to the development of the following processes:
♦ calcifications, atherocalcinosis - accumulation of calcium compounds in plaque tissue;
♦ cracks in the lid of fibroatheroma or its ulceration, which is accompanied by the development of a parietal thrombus with the threat of obstruction of the artery or its embolism;
♦ ruptures of the walls of newly formed microvessels, leading to hemorrhages in the wall of the artery, the formation of parietal and intramural thrombi.
Clinically, complications of atherosclerosis are most often manifested by ischemia and infarctions of organs and tissues supplied with blood from the affected artery.
PRINCIPLES OF PREVENTION AND THERAPY OF ATHEROSCLEROSIS
Etiotropic. It aims to eliminate or reduce the effect of risk factors. Examples of measures: the use of lipid-lowering drugs, correction of blood pressure, smoking cessation, adherence to a certain diet.
Pathogenetic. Aimed at breaking the "chain of atherogenesis". Examples of interventions: use of antiplatelet agents and anticoagulants; the use of specific drugs that reduce inflammation in atheroma (for example, statins or monoclonal antibodies to TNF-a and other pro-inflammatory cytokines).
The term "metabolism" refers to all chemical reactions that take place in the body. Without them, life human body becomes impossible, because it is only thanks to such processes that cells exist: they grow, contact with the outside world, feed and cleanse themselves. There are quite a few types of metabolism, they involve proteins, fats, and amino acids. And in some cases, the course of such processes may be disturbed, which requires appropriate correction. Let's talk on www.site about what is a disorder of fat metabolism, consider its treatment and symptoms, as well as folk remedies that will help you deal with this problem.
The term "fat metabolism" refers to the production and breakdown of fats (lipids) within the body. The processes of splitting fats are carried out mostly in the liver, as well as in adipose tissue. And failures in normal exchange lipids can cause the development of atherosclerosis, obesity, as well as various endocrine diseases (for example, diabetes mellitus). As you know, fat metabolism is characterized by a particularly complex regulation. It is influenced by insulin, sex hormones, as well as adrenaline, thyroxine and other hormones.
About how a violation of fat metabolism manifests itself, what symptoms indicate the disease
Fat metabolism occurs in almost all cells and tissues of the body. Just for this reason, the symptoms of its disorders are difficult to localize, and it is difficult to divide them into primary or secondary.
The most basic and noticeable sign of the disorder is a noticeable increase in subcutaneous adipose tissue, which is the main depot of fat in the body. In the event that the process of such accumulation occurs with particular intensity, doctors raise the issue of obesity and consider it as an independent disease. Obesity itself makes itself felt next unpleasant symptoms. This disruption results in a reduction physical abilities, provokes shortness of breath, snoring, etc. Patients with this problem experience constant hunger, because overgrown adipose tissue require food.
Obesity can cause heart disease, obstructive sleep apnea, infertility and diabetes.
Violation of fat metabolism in the body is accompanied by the accumulation of fat not only in the subcutaneous tissue, but also in the blood. As a result of such pathological processes a person develops hyperlipidemia. In this case, the patient's blood tests show an increase in the concentration of cholesterol, triglycerides, as well as low-density lipoproteins in plasma.
Blood obesity is just as dangerous as the accumulation of fat under the skin. With an increase in the amount of lipids in the blood, their particles actively penetrate the walls of the arteries. After they are deposited on the surface of the vessels, thereby giving rise to plaques of atherosclerosis. Such formations gradually grow and can cause blockage of the lumen of the vessels. In certain cases, the patient may experience a complete cessation of blood flow - a heart attack or stroke.
It is worth noting that sometimes a violation of fat metabolism is manifested by a lack of lipids. In this case, the patient begins to become exhausted, he has a shortage fat soluble vitamins A, D, E, and K. A fault also occurs menstrual cycle and reproductive functions. In addition, lipid deficiency causes a lack of essential unsaturated fatty acids, which makes itself felt by hair loss, eczema, inflammatory lesions skin and kidney damage.
About how the violation of fat metabolism is corrected, what treatment helps
Patients with metabolic disorders are shown to eliminate risk factors, in addition, they need diet food. Sometimes only these means of conservative correction are sufficient to optimize the patient's condition. However, a person with a disability metabolic processes most often you have to comply with dietary restrictions throughout life.
The menu of such patients should contain significant amount vegetables, fruits, as well as cereals and low-fat dairy products. Physical exercise are selected on an individual basis, in addition, patients need to stop smoking, drinking alcohol and beware of stress.
If such measures do not positive effect, doctors connect drug therapy. Statins can be used a nicotinic acid and its derivatives, fibrates, antioxidants and sequestrants are sometimes the drugs of choice bile acids. Medicines can only be selected by a doctor, as well as their dosage.
Treatment of violations of fat metabolism folk remedies
For the treatment of metabolic disorders, herbal medicines can be used. So a good effect is given by the infusion of Ivan-tea. Brew thirty grams of such raw materials with half a liter of boiling water, bring the medicine to a boil and insist for half an hour. Take the resulting composition of seventy milliliters four times a day.
You can also brew forty grams of plantain leaves with two hundred milliliters of boiling water. Insist wrapped for half an hour, then strain and take thirty milliliters about twenty minutes before meals three times a day.
You can also combine fifteen grams of horsetail with two hundred milliliters of boiling water. Insist wrapped for half an hour, then strain. Take fifty milliliters four times a day.
If you suspect the development of metabolic disorders, you should seek medical help.
Lipid metabolism disorders
Lipids are chemically heterogeneous substances. There are a variety of lipids in the human body: fatty acids, phospholipids, cholesterol, triglycerides, steroids, etc. A person's need for fats ranges from 80-100 g per day.
Functions of lipids
Structural: Lipids form the basis of cell membranes.
Regulatory.
† Lipids regulate membrane permeability, colloidal state and fluidity, activity of lipid-dependent enzymes (eg, adenylate and guanylate cyclases, Na + ,K + -ATPase, Ca 2+ -ATPase, cytochrome oxidase), activity of membrane receptors (eg, for catecholamines, acetylcholine , insulin, cytokines).
† Separate lipids - biologically active substances (for example, Pg, leukotrienes, platelet activating factor, steroid hormones) - regulate the functions of cells, organs and tissues.
Energy supply. Lipids are one of the main sources of energy for striated muscles, liver, kidneys and an additional source of energy for nervous tissue.
Protective. As part of subcutaneous tissue lipids form a buffer
layer that protects soft tissues from mechanical influences.
insulating. Lipids create a thermally insulating layer in the surface tissues of the body and an electrically insulating sheath around the nerve fibers.
Typical forms of pathology
Standard forms lipid metabolism pathologies are presented in fig. 10–1.
Rice. 10–1. Typical forms of pathology of lipid metabolism.
Depending on the level of lipid metabolism disorders, disorders are distinguished:
- Digestion and absorption of lipids in the gastrointestinal tract (for example, as a result of a deficiency of pancreatic lipases, disorders of bile formation and bile secretion, disorders of cavitary and "membrane" digestion).
† Transmembrane transfer of lipids from the intestine into the blood and their utilization by cells (for example, with enteritis, circulatory disorders in the wall of the small intestine).
- Metabolism of lipids in tissues (for example, with a defect or insufficiency of lipases, phospholipases, LPLase).
Depending on the clinical manifestations, obesity, malnutrition, dyslipoproteinemia, lipodystrophy and lipidosis are distinguished.
Obesity
The normal content of adipose tissue in men is 15-20% of body weight, in women - 20-30%.
Obesity - excessive (pathological) accumulation of fat in the body in the form of triglycerides. At the same time, body weight increases by more than 20–30%.
According to WHO experts, in the developed countries of Europe, from 20 to 60% of the population are overweight, in Russia - about 60%.
In itself, an increase in the mass of adipose tissue does not pose a danger to the body, although it reduces its adaptive capabilities. However, obesity increases the risk of coronary artery disease (1.5 times), atherosclerosis (2 times), hypertension(3 times), diabetes (4 times), as well as some neoplasms (for example, breast, endometrial and prostate cancer).
Types of obesity
The main types of obesity are shown in fig. 10–2.
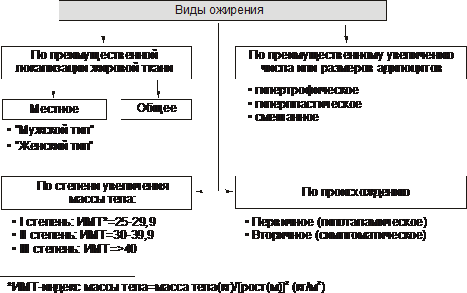
Rice. 10–2. Types of obesity. BMI - body mass index (see text).
Depending on the degree of weight gain, there are three degrees of obesity. In this case, the concept of "ideal body weight" is used.
Various formulas are used to estimate ideal body weight.
† The simplest - index Brock : subtract 100 from height (in cm).
† Body mass index is also calculated using the following formula:
Body weight is considered normal with a body mass index in the range of 18.5–24.9. If these values are exceeded, they speak of overweight (Table 10–1).
Table 10-1. Degrees of obesity
Note. BMI - body mass index
According to the predominant localization of adipose tissue, obesity is distinguished general (uniform) and local (local lipohypertrophy). Varieties of local obesity:
† Female type (gynoid) - excess subcutaneous fat mainly in the thighs and buttocks.
† Male type (android) - accumulation of fat in the abdomen.
According to the predominant increase in the number or size of fat cells, there are:
† Hyperplastic obesity (due to a predominant increase in the number of adipocytes). It is more resistant to treatment and in severe cases requires surgery to remove excess fat.
† Hypertrophic (due to a predominant increase in the mass and size of adipocytes). It is more common after 30 years of age.
† Hyperplastic-hypertrophic (mixed). Quite often comes to light and at children's age.
By genesis, primary obesity and its secondary forms are distinguished.
† Primary (hypothalamic) obesity is the result of disorders of the fat metabolism regulation system (lipostat) - an independent disease of neuroendocrine origin.
† Secondary (symptomatic) obesity is a consequence of various disorders in the body, causing:
‡ reduction of energy costs (and consequently - the consumption of triglycerides of adipose tissue),
‡ activation of lipid synthesis - lipogenesis (observed in a number of diseases, for example, in diabetes, hypothyroidism, hypercortisolism).
Causes of obesity
The cause of primary obesity is a violation of the functioning of the "adipocytes - hypothalamus" system. This is the result of a deficiency and / or insufficiency of the effects of leptin (by suppressing the production of neuropeptide Y by neurons in the hypothalamus, which increases appetite and hunger).
Secondary obesity develops with excess calorie content of food and P reduced level of energy consumption of the body. Energy consumption depends on the degree of activity (primarily physical) and the lifestyle of a person. Insufficient physical activity is one of the important reasons obesity.
The pathogenesis of obesity
Allocate neurogenic, endocrine and metabolic mechanisms of obesity.
Neurogenic variants of obesity
Neurogenic (centrogenic and hypothalamic) mechanisms of obesity are shown in Fig. 10–3.
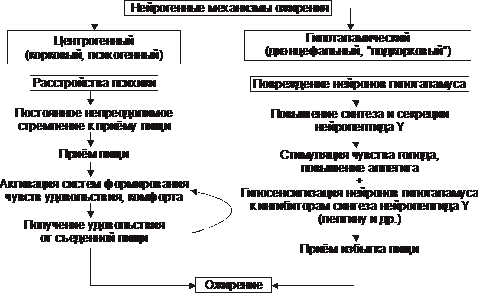
Rice. 10–3. Neurogenic mechanisms of obesity.
† Centrogenic(cortical, psychogenic) mechanism - one of the variants of eating disorders (two others: anorexia nervosa and bulimia). Reason: various mental disorders, manifested by a constant, sometimes irresistible desire to eat. Possible mechanisms:
‡ activation of serotonergic, dopaminergic, opioidergic and other systems involved in the formation of feelings of pleasure and comfort;
‡ the perception of food as a strong positive stimulus (doping), which further activates these systems - a vicious circle of the centrogenic mechanism of obesity development is closed.
† hypothalamic(diencephalic, subcortical) mechanism. Its cause is damage to the neurons of the ventromedial and paraventricular nuclei of the hypothalamus (for example, after a concussion, with encephalitis, craniopharyngioma, tumor metastases in the hypothalamus). The most important links of pathogenesis:
‡ Spontaneous (without clarified cause) increase in the synthesis and secretion of neuropeptide Y by neurons in the posterolateral ventral nucleus of the hypothalamus.
‡ Damage or irritation of the neurons of the above nucleus also stimulates the synthesis and secretion of neuropeptide Y and reduces sensitivity to factors that inhibit the synthesis of neuropeptide Y (mainly leptin).
§ Neuropeptide Y stimulates hunger and increases appetite.
§ Leptin inhibits the formation of an appetite stimulant - neuropeptide Y.
‡ Violation of the participation of the hypothalamus in the formation of hunger. This feeling is formed with a decrease in GPC, contraction of the muscles of the stomach during the evacuation of food and its emptying (feeling of food discomfort - "sucks in the pit of the stomach"). Information from peripheral sensory nerve endings is integrated into the nerve nuclei of the hypothalamus responsible for eating behavior.
‡ As a result of the above processes, the production of neurotransmitters and neuropeptides that form a feeling of hunger and increase appetite (GABA, dopamine, - endorphin, enkephalins) and / or neurotransmitters and neuropeptides that form a feeling of satiety and depress eating behavior (serotonin, norepinephrine, cholecystokinin, somatostatin) ).
Endocrine variants of obesity
Endocrine mechanisms of obesity - leptin, hypothyroid, adrenal and insulin - are shown in Fig. 10–4.
![]()
Rice. 10–4. obesity pathogenesis.
† Leptin mechanism - leading in the development of primary obesity.
‡ Leptin formed in fat cells. It reduces appetite and increases energy consumption by the body. The level of leptin in the blood is directly correlated with the amount of white adipose tissue. Many cells have leptin receptors, including neurons in the ventromedial nucleus of the hypothalamus. Leptin inhibits the production and release of neuropeptide Y by the hypothalamus.
‡ NeuropeptideY forms a feeling of hunger, increases appetite, reduces energy consumption of the body. There is a kind of negative feedback between the hypothalamus and adipose tissue: excessive food intake, accompanied by an increase in the mass of adipose tissue, leads to increased secretion of leptin. This (through inhibition of the production of neuropeptide Y) reduces the feeling of hunger. However, in obese people, this regulatory mechanism may be impaired, for example, due to increased resistance to leptin or a mutation in the leptin gene.
‡ Lipostat. The "leptin-neuropeptide Y" circuit maintains the body's adipose tissue mass - lipostat (or the body's set point in terms of the intensity of energy metabolism). In addition to leptin, the lipostat system includes insulin, catecholamines, serotonin, cholecystokinin, and endorphins.
† Hypothyroid mechanism obesity is the result of insufficient effects of iodine-containing thyroid hormones. This reduces the intensity of lipolysis, the rate of metabolic processes in tissues and the energy costs of the body.
† Adrenal(glucocorticoid, cortisol) mechanism obesity is activated due to hyperproduction of glucocorticoids in the adrenal cortex (for example, in a disease or syndrome Itsenko ‑Cushing ). Under the influence of an excess of glucocorticoids, gluconeogenesis is activated (in connection with this, hyperglycemia develops), glucose transport into adipocytes, and glycolysis (lipolytic reactions are inhibited and triglycerides accumulate).
† insulin mechanism The development of obesity develops due to direct activation of lipogenesis by insulin in adipose tissue.
† Other mechanisms. Obesity can also develop with other endocrinopathies (for example, with a deficiency of growth hormone and gonadotrophic hormones). Mechanisms for the development of obesity in these conditions are described in Chapter 27 "Endocrinopathy").
Metabolic mechanisms of obesity
† Carbohydrate stores in the body are relatively small. They are approximately equal to their daily intake with food. In this regard, a mechanism for saving carbohydrates has been developed.
† With an increase in the proportion of fat in the diet, the rate of carbohydrate oxidation decreases. This is evidenced by a corresponding decrease in the respiratory coefficient (the ratio of the rate of formation of CO 2 to the rate of consumption of O 2).
† If this does not happen (when the mechanism of inhibition of glycogenolysis is disturbed under conditions high concentration fats in the blood), a mechanism is activated that provides an increase in appetite and an increase in food intake, aimed at providing the required amount of carbohydrates in the body.
† Under these conditions, fats are stored as triglycerides. Obesity develops.
exhaustion
Wasting and cachexia - a pathological decrease in the mass of adipose tissue below normal. At the same time, the mass of muscle and connective tissue is significantly reduced.
With exhaustion, the deficit of adipose tissue can be 20-25% or more (with a body mass index below 20 kg / m 2), and with cachexia - below 50%.
Causes and types of wasting and cachexia
Distinguish between endogenous and exogenous causes of exhaustion.
Exogenous causes
† Forced or conscious complete or partial starvation (in the latter case, most often for the purpose of losing weight).
‡ Complete starvation - a state in which food does not enter the body (for example, in their absence, refusal to eat, inability to eat).
‡ Incomplete starvation is a condition characterized by a significant deficiency of plastic substances and calories in food (for example, with inadequate nutrition, quantitatively and qualitatively, homogeneous food, vegetarianism).
† Low calorie food that does not replenish the body's energy costs.
Endogenous causes
Exhaustion of endogenous genesis is divided into primary and secondary.
† Causes of primary (hypothalamic, diencephalic) wasting are discussed in Fig. 10–5.
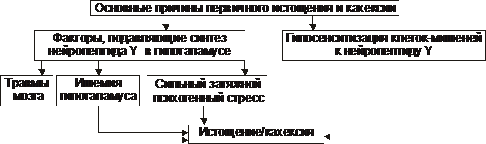
Rice. 10–5. The main causes of primary exhaustion and cachexia.
† Causes of secondary (symptomatic) wasting are shown in fig. 10–6.
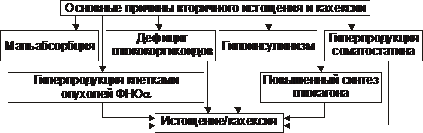
Rice. 10–6. The main causes of secondary exhaustion and cachexia.
The pathogenesis of wasting and cachexia
Exogenous wasting and cachexia. The absence or significant shortage of food products lead to the development of a chain of sequential and interdependent processes, discussed in fig. 10–7.
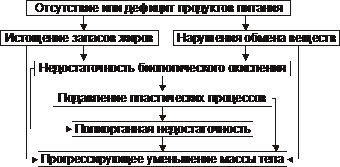
Rice. 10–7. The main links in the pathogenesis of exogenous exhaustion and cachexia.
Primary endogenous forms exhaustion and cachexia. The hypothalamic, cachectic and anorexic forms have the greatest clinical significance.
† Hypothalamic form
In the hypothalamic (diencephalic, subcortical) form of exhaustion and cachexia, there is a decrease or cessation of the synthesis and release of peptide Y into the blood by the neurons of the hypothalamus. This leads to sequential processes shown in Fig. 10–8.
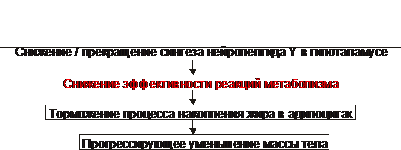
Rice. 10–8. The main links of the hypothalamic mechanism of exhaustion and cachexia.
† Cachectin form
The pathogenesis of the cachectic or cytokine form of wasting and cachexia is discussed in Fig. 10–9.
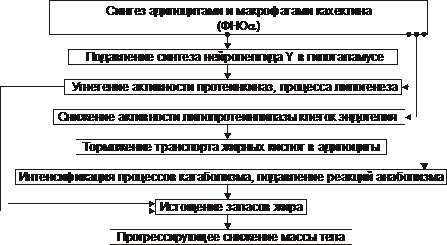
Rice. 10–9. The main links of the cachectic mechanism of exhaustion and cachexia.
† Anorexic form
The main links in the pathogenesis of anorexic malnutrition and cachexia are shown in Fig. 10–10.
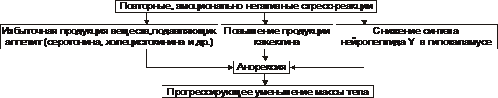
Rice. 10–10. The main links of the anorexic mechanism of exhaustion and cachexia.
‡ Individuals with a predisposition to develop anorexia have a critical attitude towards their body (perceived as having overweight) causes the development of neuropsychiatric disorders. This leads to prolonged episodes of food refusal. Most often observed in adolescent girls and girls up to 16-18 years of age.
‡ With repeated and emotionally negatively colored stress reactions, excessive formation of serotonin and cholecystokinin, which suppress appetite, is observed.
‡ The further course of the process may lead to the realization of the effects of neuropeptide Y and cachectin. These factors most likely underlie the pathogenesis of anorexia nervosa. With a protracted course of the process, a pronounced decrease in body weight develops, up to cachexia.
Secondary endogenous forms exhaustion and cachexia are important, often the main symptoms of other pathological conditions and diseases (Fig. 10-11).
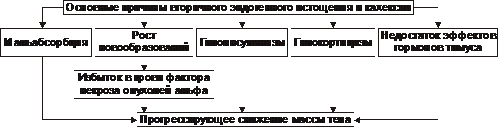
Rice. 10–11. The main causes of secondary endogenous wasting and cachexia.
Lipodystrophy
Lipodystrophy is a condition characterized by a generalized or local loss of adipose tissue, less often by its excessive accumulation in the subcutaneous tissue. The causes of lipodystrophy are varied and not always known, ranging from mutations in various genes (eg, lamins) to post-injection complications. There is a large group of hereditary and congenital syndromes of lipodystrophy, some of them are discussed in the article "Lipodystrophy" (appendix "Reference book" on CD).
Lipidoses
Lipidoses are a typical form of lipid metabolism disorder characterized by metabolic disorders of various lipids (for example, sphingolipidoses, gangliosidoses, mucolipidoses, adrenoleukodystrophy, leukodystrophy, lipofuscinosis, cerebrosidoses) in cells (parenchymal lipidosis), adipose tissue (obesity, malnutrition) or arterial vessel walls (atherosclerosis). , arteriosclerosis). These forms of lipidosis are described in this textbook (Chapter 4 "Cell Damage" in this chapter, as well as in the articles in the Glossary of Terms appendix on the CD).
Dyslipoproteinemia
Dyslipoproteinemia - conditions characterized by a deviation from the norm of the content, structure and ratio of various drugs in the blood. LP metabolism disorders are the main link in the pathogenesis of atherosclerosis, coronary artery disease, pancreatitis and other diseases.
The nature of the course and clinical manifestations of dyslipoproteinemia are determined by:
Hereditary properties of the body (for example, the composition, ratio and level of various drugs; the characteristics of their metabolism).
Environmental factors (for example, a set of foodstuffs, features of the diet and mode of eating).
The presence (or absence) of concomitant diseases (eg, obesity, hypothyroidism, diabetes, kidney and liver damage).
Characterization of lipoproteins
Various lipids circulate in the blood plasma. Free fatty acids are transported by albumins, and triglycerides, cholesterol, cholesterol esters and phospholipids, a small amount of fatty acids are transported as part of the LP. These spherical particles are composed of a hydrophobic core (contains cholesterol esters and triglycerides) and a hydrophilic shell (contains cholesterol, phospholipids and apolipoproteins). The main characteristics of different drugs are given in Table. 10–2.
Table 10-2. Types and main properties of lipoproteins
|
Chylomicrons | |||||
|
Particle size (nm) |
75–1200 | ||||
|
Density (g/cm 3 ) |
0,98–1,006 |
1,006–1,019 |
1,019–1,063 |
1,063–1,210 |
|
|
Compound (%): | |||||
|
Cholesterol | |||||
|
Triglycerides | |||||
|
Phospholipids | |||||
|
ApoLP |
B48, AI, AII, AIV, CI, CII, CIII, E |
B100, CI, CII, CIII, E |
AI, AII, AIV, CI, CII, CIII, E |
||
|
Source |
Small intestine, dietary lipids |
Liver, small intestine |
VLDL, LPPP |
Small intestine, liver |
|
|
atherogenicity |
not proven |
not proven |
Anti-atherogenic |
||
Apolipoproteins ensure the preservation of the ordered structure of LP micelles, the interaction of LP with cell receptors, and the exchange of components between LP. Detailed specifications apoLP and their defects is given in the article “Defects in apolipoproteins” (see Appendix “Reference book” on CD-ROM).
Atherogenicity of lipoproteins
LP are divided into atherogenic and anti-atherogenic (Fig. 10–12).
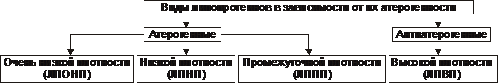
Rice. 10–12. Types of lipoproteins depending on their atherogenicity.
The antiatherogenic effect of HDL is determined by their following properties:
† The ability to remove excess cholesterol from the plasma membrane of cells, including the vascular endothelium, and transport it to the liver, where cholesterol is removed in the bile.
† Higher affinity of HDL for apoLP E and apoLP B receptors compared to LDL. It's defined high content apoLP E to HDL. As a result, HDL prevents cells from taking up particles saturated with cholesterol.
The assessment of the potential atherogenicity of blood LP is carried out by calculating the cholesterol coefficient of atherogenicity:
Normally, the cholesterol coefficient of atherogenicity does not exceed 3.0. With an increase in this value, the risk of developing atherosclerosis increases.
Types of dyslipoproteinemia
The main types of dyslipoproteinemia are shown in fig. 10–13.
Rice. 10–13. Types of dyslipoproteinemia.
More than 30% of primary dyslipoproteinemias are inherited forms of pathology (both monogenic and polygenic with multifactorial genesis).
About 70% of dyslipoproteinemias are considered acquired. Secondary (acquired) dyslipoproteinemias are symptoms of other diseases. They accompany many human diseases (Table 10-3).
Table 10-3. The most frequent pathological processes leading to the development of secondary dyslipoproteinemia
|
Disease |
Development mechanism |
|
|
Diabetes |
I, IV, V |
Decreased activity of LPLase, excessive influx of fatty acids into the liver, increased synthesis of VLDL |
|
lipid secretion disorders |
||
|
Primary cirrhosis of the liver |
Violation of LP synthesis |
|
|
nephrotic syndrome |
II, IV, V |
Increased formation of LP and triglycerides |
|
Hypothyroidism |
II, IV | |
|
Pituitary insufficiency |
Decreased lipid catabolism |
|
|
Chronic alcoholism |
IV, V |
Decreased LPLase activity, increased LP synthesis |
Various hereditary defects, as well as acquired pathological processes and diseases often lead to similar changes in the content and profile of various drugs. In this regard, a fine differentiation of their origin is required, which makes it possible to carry out their effective treatment.
Hyperlipoproteinemia
Hyperlipoproteinemia - conditions characterized by a disorder in the formation, transport and metabolism of LP and manifested by a persistent increase in plasma cholesterol and / or triglycerides.
Classification
In 1967, Fredrickson et al developed a classification of hyperlipoproteinemias (hyperlipidemias). The content data was based on total cholesterol and triglycerides in blood plasma, as well as the distribution of LP fractions during their electrophoresis and ultracentrifugation. On this basis, five types of hyperlipoproteinemias have been identified. Later, this classification was revised by WHO experts (Table 10-4).
Violations and their causes in alphabetical order:
lipid metabolism disorders
Whole line disease is caused lipid metabolism disorders. The most important among them are atherosclerosis and obesity. Diseases of cardio-vascular system, as a consequence of atherosclerosis, occupy the first place in the structure of mortality in the world. One of the most common manifestations of atherosclerosis is coronary vessels hearts. The accumulation of cholesterol in the walls of blood vessels leads to the formation of atherosclerotic plaques. They, increasing in size over time, can block the lumen of the vessel and interfere with normal blood flow. If, as a result, the blood flow is disturbed in coronary arteries, then there is angina pectoris or myocardial infarction. Predisposition to atherosclerosis depends on the concentration of transport forms of blood lipids - plasma alpha-lipoproteins.
What diseases cause a violation of lipid metabolism:
Accumulation of cholesterol (CS) in the vascular wall occurs due to an imbalance between its entry into the intima of the vessels and its exit. As a result of this imbalance, cholesterol accumulates there. In the centers of accumulation of cholesterol, structures are formed - atheromas. There are two most well-known factors that cause lipid metabolism disorders.
1. Firstly, these are changes in LDL particles (glycosylation, lipid peroxidation, phospholipid hydrolysis, apo B oxidation). Therefore, they are captured by special cells - "scavengers" (mainly macrophages). The capture of lipoprotein particles with the help of "junk" receptors proceeds uncontrollably. Unlike apo B/E - mediated endocytosis, this does not cause regulatory effects aimed at reducing the entry of cholesterol into the cell, described above. As a result, macrophages become overwhelmed with lipids, lose their waste-absorbing function, and turn into foam cells. The latter linger in the wall blood vessels and begin to secrete growth factors that accelerate cell division. Atherosclerotic cell proliferation occurs.
2. Secondly, it is the inefficient release of cholesterol from the endothelium vascular wall circulating in blood HDL.
Factors affecting elevated level LDL in humans
Gender - higher in men than in premenopausal women and lower than in postmenopausal women
- Aging
- Saturated fats in the diet
- high consumption cholesterol
- Diet low in coarse fibrous foods
- Alcohol consumption
- Pregnancy
- Obesity
- Diabetes
- Hypothyroidism
- Cushing's disease
- Uremia
- Nephrosis
- Hereditary hyperlipidemias
Lipid metabolism disorders (dyslipidemia), characterized primarily by high content blood cholesterol and triglycerides are the most important factors risk of atherosclerosis and related diseases of the cardiovascular system. Plasma concentration of total cholesterol (CH) or its fractions closely correlates with morbidity and mortality from coronary artery disease and other complications of atherosclerosis. Therefore, the characteristic of lipid metabolism disorders is prerequisite effective prevention cardiovascular diseases.
Lipid metabolism disorders can be primary and secondary and are characterized only by an increase in cholesterol (isolated hypercholesterolemia), triglycerides (isolated hypertriglyceridemia), triglycerides and cholesterol (mixed hyperlipidemia).
The primary lipid metabolism disorder is determined by single or multiple mutations of the corresponding genes, resulting in overproduction or impaired utilization of triglycerides and LDL cholesterol or overproduction and impaired HDL clearance.
Primary lipid disorders can be diagnosed in patients with clinical symptoms these violations, early start atherosclerosis (up to 60 years), in individuals with a family history of atherosclerosis or with an increase in serum cholesterol > 240 mg / dl (> 6.2 mmol / l).
Secondary lipid metabolism disorder occurs, as a rule, in the population of developed countries as a result of sedentary image life, consumption of food containing a large amount of cholesterol, saturated fatty acids.
Other causes of secondary lipid metabolism disorders can be:
1. Diabetes.
2. Alcohol abuse.
3. Chronic renal failure.
4. Hyperthyroidism.
5. Primary biliary cirrhosis.
6. Taking certain drugs (beta-blockers, antiretroviral drugs estrogens, progestins, glucocorticoids).
Hereditary disorders of lipid metabolism:
A small number of people have hereditary disorders lipoprotein metabolism, manifested in hyper- or hypolipoproteinemia. Their cause is a violation of the synthesis, transport or cleavage of lipoproteins.
In accordance with generally accepted classification, distinguish 5 types of hyperlipoproteinemia.
1. The existence of type 1 is due to insufficient activity of LPL. As a result, chylomicrons are very slowly removed from the bloodstream. They accumulate in the blood, and the level of VLDL is also higher than normal.
2. Hyperlipoproteinemia type 2 is divided into two subtypes: 2a, characterized by a high content in blood LDL, and 2b (increased LDL and VLDL). Type 2 hyperlipoproteinemia is manifested by high, and in some cases very high, hypercholesterolemia with the development of atherosclerosis and coronary disease hearts. The content of triacylglycerols in the blood is within the normal range (type 2a) or moderately elevated (type 2b). Hyperlipoproteinemia type 2 is characteristic of serious illness- hereditary hypercholesterolemia affecting young people. In the case of the homozygous form, it ends fatal in young age from myocardial infarctions, strokes and other complications of atherosclerosis. Type 2 hyperlipoproteinemia is widespread.
3. With type 3 hyperlipoproteinemia (dysbetalipoproteinemia), the conversion of VLDL to LDL is disrupted, and pathological floating LDL or VLDL appear in the blood. In the blood, the content of cholesterol and triacylglycerols is increased. This type is quite rare.
4. With type 4 hyperlipoproteinemia, the main change is an increase in VLDL. As a result, the content of triacylglycerols in the blood serum is significantly increased. It is associated with atherosclerosis of the coronary vessels, obesity, diabetes. It develops mainly in adults and is very common.
5. Type 5 hyperlipoproteinemia - an increase in the serum content of HM and VLDL, associated with moderate decreased activity lipoprotein lipases. The concentration of LDL and HDL is below normal. The content of triacylglycerols in the blood is increased, while the concentration of cholesterol is within the normal range or moderately elevated. Occurs in adults but widespread does not have.
Typing of hyperlipoproteinemias is carried out in the laboratory on the basis of a study of the blood levels of various classes of lipoproteins by photometric methods.
As a predictor of atherosclerotic lesions of the coronary vessels, the indicator of cholesterol in the composition of HDL is more informative. Even more informative is the coefficient reflecting the ratio of atherogenic drugs to anti-atherogenic drugs.
The higher this ratio, the more danger occurrence and progression of the disease. In healthy individuals, it does not exceed 3-3.5 (in men it is higher than in women). At patients with coronary artery disease it reaches 5-6 or more units.
Is diabetes a lipid metabolism disease?
The manifestations of lipid metabolism disorders are so pronounced in diabetes that diabetes is often called more disease lipid than carbohydrate metabolism. The main disorders of lipid metabolism in diabetes are an increase in lipid breakdown, an increase in the formation of ketone bodies and a decrease in the synthesis of fatty acids and triacylglycerols.
At healthy person usually 50% of incoming glucose is broken down by CO2 and H2O; about 5% is converted to glycogen, and the rest is converted to lipids in fat depots. In diabetes, only 5% of glucose is converted into lipids, while the amount of glucose decomposing into CO2 and H2O also decreases, and the amount converted into glycogen changes slightly. The result of impaired glucose intake is an increase in blood glucose levels and its removal in the urine. Intracellular glucose deficiency leads to a decrease in the synthesis of fatty acids.
In untreated patients, an increase in plasma levels of triacylglycerols and chylomicrons is observed, and the plasma is often lipemic. An increase in the level of these components causes a decrease in lipolysis in fat depots. The decrease in lipoprotein lipase activity further contributes to the reduction in lipolysis.
lipid peroxidation
feature of lipids cell membranes is their significant unsaturation. Unsaturated fatty acids are easily subjected to peroxide degradation - LPO (lipid peroxidation). The membrane's response to damage is therefore called "peroxide stress".
LPO is based on a free radical mechanism.
Free radical pathology is smoking, cancer, ischemia, hyperoxia, aging, diabetes, i.e. in almost all diseases there is an uncontrolled formation free radicals oxygen and intensification of LPO.
The cell has a system of protection against free radical damage. The antioxidant system of cells and tissues of the body includes 2 links: enzymatic and non-enzymatic.
Enzymatic antioxidants:
- SOD (superoxide dismutase) and ceruloplasmin involved in the neutralization of oxygen free radicals;
- catalase catalyzing the decomposition of hydrogen peroxide; glutathione system providing catabolism of lipid peroxides, peroxide modified nucleotides and steroids.
Even a short-term lack of non-enzymatic antioxidants, especially antioxidant vitamins (tocopherol, retinol, ascorbate), leads to persistent and irreversible damage to cell membranes.
Which doctors to contact if there is a violation of lipid metabolism:
Have you noticed a violation of lipid metabolism? Do you want to know more detailed information or do you need an inspection? You can book an appointment with a doctor– clinic Eurolaboratory always at your service! The best doctors examine you, study external signs and help identify the disease by symptoms, advise you and provide needed help. you also can call a doctor at home. Clinic Eurolaboratory open for you around the clock.symptoms of diseases and do not realize that these diseases can be life-threatening. There are many diseases that at first do not manifest themselves in our body, but in the end it turns out that, unfortunately, it is too late to treat them. Each disease has its own specific symptoms, characteristic external manifestations- so called disease symptoms. Identifying symptoms is the first step in diagnosing diseases in general. To do this, you just need to several times a year be examined by a doctor not only to prevent terrible disease but also support healthy mind in the body and the body as a whole.
If you want to ask a doctor a question, use the online consultation section, perhaps you will find answers to your questions there and read self care tips. If you are interested in reviews about clinics and doctors, try to find the information you need on. Also register for medical portal Eurolaboratory to be constantly up to date latest news and updates of information on the site, which will be automatically sent to you by mail.
The symptom map is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and how to treat it, contact your doctor. EUROLAB is not responsible for the consequences caused by the use of the information posted on the portal.
If you are interested in any other symptoms of diseases and types of disorders or you have any other questions and suggestions - write to us, we will definitely try to help you.

