The structure of the female pelvis. Female organs of the small pelvis. Possible anomalies in the development of the pelvic organs in women
Where are the muscles pelvic floor womenConsider the structure of the female pelvic organs, after all, it is the muscles of the small pelvis that we are going to strengthen with Kegel exercises, gymnastics for intimate muscles, training methods - wumbling / imbilding / intimate fitness, as well as with the help of popular vaginal simulators Jade Egg and KEGEL BALLS recommended for self-development. |
The uterus, bladder, rectum have a separate entrance (sphincter). The sphincters pass through the muscles of the pelvic floor. The pelvic organs have very elastic muscles that can contract and stretch strongly.
Observation and pelvic floor exercises during pregnancy have scientifically proven benefits for the prevention of incontinence and sexual dysfunction. To avoid further linking the association between normal delivery and sexual life in a country with a trivialized caesarean section, the specialist emphasizes that it cannot be guaranteed that C-section protects the pubic floor. Childbirth is not only about muscles, he says. For example, the Ministry of Health warns that an unplanned caesarean section increases the risk of maternal death by 120 times compared to the risk of premature birth and respiratory angiosis syndrome.
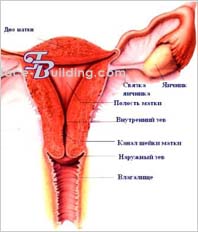
female organs small pelvis fit snugly enough to each other and are in a curved position. In this case, the uterus rests on the bladder, the bladder - on the vagina. The rectum is supported by the coccyx. This position ensures the stability and proper functioning of the pelvic organs. Especially such support is required in a standing position. If the correct position of one of the pelvic organs is violated, the entire interconnected system is disrupted, causing diseases of the pelvic organs.
For physiotherapist Elsa Baracho, every woman who has a desire to become pregnant should undergo physical therapy. According to her, at the 21st week of pregnancy, the perineal region muscle changes its shape, and this change will affect during pregnancy and after childbirth. "Typical delivery or caesarean section, the woman will have a change in the musculature of the pubic floor," he summarizes.
The difference, she says, is that - in the case of normal labor - working on this muscle helps in childbirth, during exile, the woman becomes more active in the process of childbirth, and also prevents injury. Ordinary labor is not synonymous with pubic problems. Many women still believe in the myth of a collapsed bladder if the birth is vaginal, but it can happen to those who have had a C-section, he says.
Pelvic muscles hold everything securely pelvic organs inside to anatomically correct position. Stretched like a hammock from below the pelvis, muscle layer(pubic-coccygeal muscle) consists of internal and outer layers muscles that work together to hold and normal functioning pelvic organs, and therefore women Health. Along with developing and strengthening the muscles of the small pelvis, Kegel exercises also increase blood flow to the pelvic area which stimulates enhanced cell renewal.
"Strengthening the region has helped during pregnancy, childbirth, and beyond." According to her, Brazil is undergoing major changes in obstetrics. We are the land of Caesar. For a long time, little has been put into the essence of midwifery that a woman becomes pregnant and her birth is spontaneous or at least enters into labor. Our caesarean norms unacceptable. In this context, many things have been thrown under the carpet, and the subject pelvic floor during pregnancy is one of them. But women themselves have awakened to this problem, which is real and has always existed.
Society and the medical community are also imbued with the spirit of restructuring obstetric care, and in this transition we can't stop talking about this topic. We must be able to offer a safe and adequate normal birth, including the prevention of manned sex dysfunctions. Having vaginal delivery is the end of every healthy pregnancy, every woman has that ability, he says.
Like other muscles pelvic muscles can only be kept in good shape through regular exercise.
Weakened perineal and pelvic muscles can lead to symptoms such as urinary or fecal incontinence due to poor self-control of bowel function or Bladder.
Psychologist Thais Dufles Vieira, 35, is the son of David, aged 2, and five months pregnant with Edouard. This represents an exception to the current Brazilian model of obstetric care. Although information about the importance of monitoring the muscles in the pubic cavity is not part of the medical protocol for prenatal care, she, who has always dreamed of normal birth, studied on her own during her first pregnancy, was looking for a physiotherapist to evaluate this muscle group and perform exercises indicated by a specialist.
She gave birth to her first child and guaranteed not only the integrity of the perineum. Strengthening the region helped during pregnancy, childbirth and after that. At no point did I leak urine and my delivery was very smooth, he says. The first pregnancy not only helped Eduarda deliver the baby, but also serves as a cumulative experience. For the first time, among my problems was the bladder and intercourse in the postpartum period.
Weak pelvic muscles can also lead to difficult labor due to insufficient muscle activity during labor activity, decrease sexual desire and satisfaction from intimacy, prolapse of the uterus and vagina, and even prolapse internal organs cause many dysfunctions and diseases of the pelvic organs.
Urinary and fecal incontinence and sexual dysfunctions are some of the problems that can be caused by gestation. Pelvic floor dysfunctions are multifactorial: age, excessive weight gain, multiple births, age, and menopause. Childbirth is not the only cause of lesions on the pubis, says the doctor.
She has two children who were born by caesarean section. In fact, it was my muscle that was contracting, he says. Elsa Baracho also refers to dysfunctions of the pubic floor in the posterior compartment, called coloproctolytic dysfunctions, which can be the cause of intestinal constipation or fecal incontinence. If the problem is in the middle compartment, the specialist clarifies that there is a direct connection with the vagina and the oster. Thus, the exercise of this muscle group avoids the same distraction as it improves the sensitivity of the vagina and promotes sexual pleasure.
Muscles of the vagina
The vagina is an elastic canal, an easily stretchable muscular tube that connects the vulva and uterus. The average length (depth) of the vagina is between 7 and 12 cm. The size of the vaginal canal for each woman may vary slightly.
The walls of the vaginal muscle consist of three layers: inner, middle (muscular) and outer.
Sexuality, however, is a health condition that needs to be analyzed multifactorially as well. Muscles can help, but they don't. causing factor sexual pleasure. The physiotherapist explains that sexual satisfaction has four phases - desire, arousal, orgasm, and resolution. " muscle weakness hurts the arousal phase,” she says.
Elsa Baracho further explains that pain in sexual relations may be a sign of a hypertonic muscle that prevents the fiber from relaxing. “In this case, we have to treat that muscle first and then work on increasing the strength,” he explains.
|
Muscles of the vagina are made up of smooth muscle. The muscle bundles are oriented mainly in the longitudinal direction, but there are also circular bundles. In the upper part of the vaginal muscles pass into the muscles of the body of the uterus. In the lower part of the vagina, the muscles become stronger, gradually weaving into the muscles of the perineum. The muscles of the vagina, like any smooth muscle, cannot be controlled consciously, but at the same time, the muscles of the vagina can be greatly stretched during labor. The diagnosis of dysfunction of the manned floor was made by a doctor. A physical therapist evaluates the pelvic floor musculature to determine if there is a neuromuscular deficit. This functional evaluation consists of inspection, attachment of muscle structures and tests using equipment that gives a professional parameter that helps to confirm the degree of muscle strength and measure the electrical activity of the fiber. Through appetite, a woman can be more confidently aware of the possible contraction of a certain muscle. Elsa Baracho reinforces the need for self-knowledge female anatomy, which can be the same as seeing shapes or touching. In the vast majority of cases, treatment consists of physical therapy exercises, but depending on the type of injury, you may need surgery. “The exercises are simple and consist mainly of contraction and relaxation of this muscle and can be done at home,” says Claudia Soares Laranjeira. You can control the compression of the muscles of the vaginal canal by changing the intra-abdominal pressure, increasing its strength, we get compression, and decreasing it, relaxation. |
 |
Intra-abdominal pressure is created in abdominal cavity, which is limited from below by the muscles of the pelvic floor, from above by the respiratory diaphragm, in front and sides - by the transverse muscles of the press, behind - by the muscles of the back.
This is a problem that has been bothering me for a long time. When that wasn't possible, he used absorbents to try and minimize discomfort, he says. She has learned the exercises, sees a physical therapist periodically, and is living in a different phase of life.
Free and open lectures for the public: May 13, from 5 to 6, Tourmaline room, Minascentro - preparing the body for pregnancy, childbirth and postpartum period- special care with the flap and abdomen. How important is it to maintain the function of the muscles of the floor of the leg in order to get a good sexual activity? Our teams work with pregnant women to prevent the occurrence of obstetric fistulas while looking at women with the condition and suggesting psychological support to help them rebuild their lives.
If you simultaneously strain the muscles of the pelvic floor, lower the respiratory diaphragm and retract the abdominal muscles, then intra-abdominal pressure increases and the walls of the vaginal canal (vagina) are compressed.
The vaginal compression technique is mainly used during intimacy, for stronger compression of the partner's penis along the entire length of the vagina, or to massage the walls of the vaginal canal.
While any woman can be susceptible to fistula, most cases occur in African countries. It's in to a large extent hidden problem that affects young women giving birth at home in remote and poor areas with little or no access to maternal health care.
If a woman experiences a difficult delivery and ends up with an obstetric fistula as a result, her family and community often isolate her. Because of this social stigma, a woman is less likely to receive care. What causes a fistula? Almost all fistulas occur due to obstructions. In remote regions of Africa where there are few hospitals, midwives and obstetric care are rare, complications can extend delivery for several days.
How to strengthen your pelvic floor muscles
For the development of the pelvic floor muscles and the ability to control them, use Kegel exercises, gymnastics for intimate muscles, wumbilding / imbilding and similar techniques.
To develop a skill management intra-abdominal pressure use pneumatic vaginal simulators.
Similar content
Without access to emergency cesareans, these complications can be fatal. However, if the woman is going through labor, normal birth canal injuries are common. During childbirth, the birth of a baby may be interrupted due to the size of the baby's head, which is too large for the mother's pelvis, or even the size of the pelvis, which can be very small. Birth may also be terminated if the uterus is not working properly.
When the baby's head presses against part of the birth canal, the tissue that covers it eventually dies and creates a hole, a fistula, an abnormal connection between the vagina and bladder, vagina and rectal canal, or both. This tear will never heal naturally, and usually the baby is stillborn, which further suffers from the mother.
Kegel exercises for women - Help with uterine prolapse, urinary incontinence
Kegel gymnastics for the pelvic floor muscles - A set of exercises according to the Kegel method
Although cases are rare, our surgeons have also treated a small number of cases of obstetric fistula caused by extreme sexual abuse. Fistula Symptoms Due to the abnormal opening that has been created to the bladder or rectum, a woman with a fistula will suffer from persistent urinary and fecal incontinence through her vagina. Liquids cause bad smell and can cause ulceration or burns on a woman's legs.
Typically, women drastically reduce their fluid intake in an attempt to reduce the flow of urine, which can lead to kidney disease or kidney stones. In most cases, women with obstetric fistulas develop psychological symptoms. Because of physical symptoms they are constantly excluded by the community and leave their husbands who will be looking for a "healthy" wife.
Step-by-step instructions for performing exercises with the KEGEL BALLS simulator - A technique for independent development. Alternatively, the Jade Egg trainer can be used. Attention! Perform only after preliminary strengthening of the pelvic muscles with the help of exercise without equipment.
Complications during childbirth can sometimes cause nerve damage, leading to paralysis of one or both of a woman's legs or difficulty bending her legs, a condition known as "dropped leg". These issues can further isolate women, which in turn can lead to malnutrition and exclusion from society.
Fistula treatment. Thanks to quality obstetric care, fistulas are preventable - the condition has disappeared in developed countries. In some cases, simple repairs can take as little as 45 minutes, but many are more complex and require multiple procedures performed by highly trained surgeons. Only a few institutions in Africa teach these specialized techniques.
|
After the operation, the patient will have to keep the catheter attached to the bladder for several weeks and learn how to do it. pelvic exercises to strengthen your muscles. Fortunately, women who have had a repaired obstetric fistula can have healthy babies in the future if they receive adequate prenatal care.
Training local midwives to help the mother deliver safely has importance. They can assess whether the mother is having problems with childbirth and getting help before it is too late. However complete treatment goes beyond the surgical aspect.
Topographic anatomy of the small pelvis.
Taz,pelvis.
Borders. The pelvis is the part of the body located between the abdomen and lower limbs and limited from the outside by the pelvic bones, the sacrum, the coccyx, and from below by the perineum.
External landmarks:
Iliac crest, crista iliaca; - superior anterior iliac spine, spina iliaca anterior superior; - pubic tubercle, tuberculum pubicum; - pubic symphysis, symphysis pubica; - dorsal surface of the sacrum, facies dorsalis os sacrum; - coccyx, os coccyges; - ischial tubercle, tuber ischiadicum; - greater skewer femur, trochanter major ossis femoralis; - subpubic angle, angulus subpubicus
Individual, sex and age differences:
1. Individual features of the pelvis. It consists in different ratios of the longitudinal and transverse diameters of the pelvic ring. With one extreme type of variability, the longitudinal diameter is larger than the transverse one, while the pelvis is “squeezed” from the sides, the axis pelvic organs more often inclined towards the sacrum. With another type of variability, the longitudinal diameter is less than the transverse one, the pelvis is “compressed” in the anteroposterior direction, and the axes of the pelvic organs are inclined towards the pubic symphysis.
2. Sex differences in the pelvic skeleton: - wings ilium in women, they are located more horizontally, so in women the pelvis is wider and lower than in men; - the lower branches of the pubic bones in women are located at an obtuse angle and form a pubic arch, arcus pubis; in men, they are located at an acute angle and form a subpubic angle, angulus subpubicus;
The pelvic cavity in women has the shape of a curved cylinder, in men - a curved cone;
Pelvic tilt, inclination pelvis - the angle between the horizontal plane and the plane of the upper pelvic aperture - in women 55-60, in men 50-55.
3. Age differences. By the time of birth, the pelvis consists of 3 parts, each of which has ossification nuclei. All 3 parts - iliac, ischial and pubic - are connected by layers of cartilage in the acetabulum. The iliac fossa is almost absent. By 7 years old pelvic bone doubles, then up to 12 years, growth slows down. By the age of 13-18, parts of the pelvic bone grow together, their ossification ends. The final synostosis of all elements of the pelvic bone is completed by the age of 25.
The walls of the pelvis. Limit the pubic, iliac, ischial bones, sacrum and coccyx.
pelvic floor form the pelvic diaphragm, diaphragma pelvis, and partly the urogenital diaphragm, diaphragma urogenitale.
urinary diaphragm,diaphragma urogenitale. It is formed by 2 muscles: the deep transverse muscle of the perineum and the external sphincter of the urethra.
D pelvic diaphragm. Formed by 2 muscles: the muscle that raises the anus, m. levator ani, and the coccygeal muscle, m. coccygeus.
Floors of the pelvic cavity. The pelvic cavity is divided into three floors: upper - peritoneal, cavum pelvis peritoneale, middle - subperitoneal, cavum pelvis subperitoneale, lower - subcutaneous, or perineal, cavum pelvis subcutaneum s. Perineale.
The course of the peritoneum in the male pelvis. Here, the peritoneum from the anterior wall of the abdomen passes to the bladder, covering the upper wall, partially - the side and back. On the sides of the bladder, the peritoneum forms fossae paravesicales. At the level of the symphysis, the peritoneum forms the plica vesicalis transversa. Descending along the posterior wall of the bladder, the peritoneum covers the medial edges of the ampullae of the vas deferens, the tops of the seminal glands, and passes to the rectum, forming a rectovesical depression, excavatio rectovesicalis. Moreover, the supraampullary part of the rectum is covered with peritoneum on all sides, the ampulla is covered on 3 sides for a large extent, and Bottom part the rectum is not covered by the peritoneum at all.
The course of the peritoneum in the female pelvis. Here the peritoneum also passes from the anterior wall of the abdomen to the bladder, forming a transverse fold, then covers its upper and posterior walls. After that, it passes to the anterior surface of the uterus at the level of its isthmus, forming a shallow vesicouterine cavity, excavatio vesicouterina. On the anterior surface of the uterus, the peritoneum covers only the body of the uterus. On the posterior surface of the uterus, the peritoneum covers the body, supravaginal part of the cervix and posterior fornix vagina and passes to the rectum, forming a deep recto-uterine cavity, excavatio rectouterina (Douglas space). It is limited by the folds of the peritoneum - plicae rectouterinae, which continue to the anterior surface of the sacrum.
Fascia and cellular spaces, their connections with cellular spaces of neighboring areas.
Parietal pelvic fascia, fascia pelvis parietalis, covers the back of the anterior surface of the sacrum and is called pre-sacral, fascia presacralis, on the sides - parietal muscles: m. piriformis, m. obturatorius internus, having the corresponding names (fascia obturatoria, fascia m. piriformis), in front - the posterior surface of the symphysis and the upper branches of the pubic bones, from below - the upper surface of m. levator ani.
Visceral pelvic fascia, fascia pelvis visceralis, lines the extraperitoneal parts of the pelvic organs in men and forms two sagittal spurs stretching from the pubic bones to the sacrum. Part of the visceral fascia, stretching from the pubic bone to the prostate gland in men or to the bladder in women, is called the pubic-prostatic, lig. Puboprostaticum, or pubic-cystic, lig. Pubovesicale, ligament. These ligaments accompany bundles of smooth muscle fibers m. Puboprostaticus and m.Pubovesicalis. The sagittal spurs of the visceral fascia, located behind the bladder, also contain bundles of smooth muscle fibers that form several muscles: rectococcygeal, m. sacrococcygeus; rectovesical, m. Rectovesicalis in men and recto-uterine in women. Lining the pelvic organs, the visceral fascia of the pelvis forms a capsule of the rectum (Amyusse capsule) and a capsule prostate(Pirogov-Reitzia capsule).
Cellular spaces. The main cellular spaces of the small pelvis are located within the subperitoneal floor of the pelvis.
Visceralcellular spaces are gaps between the wall of the organ and the visceral fascia. There are: paravesical, paraprostatic, paravaginal, paracervical and pararectal visceral cellular spaces.
Parietal cellular spaces in the subperitoneal floor of the small pelvis of a woman there are four: retropubic (pre-vesical). two lateral and presacral (posterior rectal). In men, one more, fifth , retrovesical cellular space.
Children's features.
The fasciae of the pelvis are very thin and loose. The parietal fascia is closely adjacent to the fascial sheaths of the parietal vessels. The parietal and near-organ cellular spaces contain a small amount of adipose tissue, which makes the anterior and
posterior Douglas space.
Internal iliac vessels.
The main arterial trunk that supplies blood to the pelvic organs is internaliliac artery, A. iliaca interna.
Branches of the internal iliac artery:
- parietal: A. ileolumbalis.,A. sacralis lateralis., A. obturatorius., A. glutea superior., A. glutea inferior.
- visceral :, A. umbilicalis (a. vasicalis superior)., A. vesicalis inferior., A. rectalis media., A. pudenda interna. A. uterina (a. ductus deferentis).
At the level of the upper edge of the greater sciatic foramen a. iliaca interna is divided into anterior and posterior trunks.
From the front trunk originate predominantly visceral arteries: aa. uterina, vesicalis inferior, rectalis media; two parietal arteries, aa. umbilicalis et obturatoria, are directed anteriorly. The umbilical artery has two parts: an open part, pars patens, from which the superior vesical artery and the artery of the vas deferens depart, and a closed part, pars occlusa. This obliterated part of the artery reaches the visceral fascia of the bladder and then, together with it, goes to the navel.
The end part of the anterior trunk at the piriform opening is divided into the internal genital, a. pudenda interna, and lower gluteal, a. glutea inferior, arteries.
Posterior trunk of the internal iliac artery gives off parietal arteries: aa sacrales laterales, iliolumbalis et glutea superior. A. iliolumbalis anastomoses with its lumbar and iliac branches with the lumbar and intercostal arteries and with a circumflexa ilium profunda and gluteal arteries. Due to this, collateral blood flow occurs when the common iliac artery is occluded.
Venous drainage from the pelvic organs carried out first in the venous plexus, which have the same names: pl. venosus rectalis, pl. venosus vesicalis, pl. venosus prostaticus, pl. venosus uterinus, pl. venosus vaginalis. Then the blood from these plexuses flows into internal iliac vein, which is located deeper than the artery and medial from it. The parietal veins accompany the arteries in the form of paired vessels.
Children's features.
The arteries of the small pelvis of a newborn have their own characteristics, due to the peculiarities of the blood supply to the fetus: the common iliac, internal iliac (its anterior trunk) and umbilical arteries are represented by a single main vessel the same diameter throughout.
The sacral plexus.
It is formed by the anterior branches of the IV and V lumbar and the anterior branches of the I, II, III, IV sacral spinal nerves exiting through the anterior sacral foramen. It lies on the anterior surface of the piriformis muscle.
From the sacral plexus depart short and long branches. short branches n. obturatorius is directed along the side wall of the pelvis to the obturator foramen. N. gluteus superior goes into the epipiriform opening with the same artery and vein. N. gluteus inferior and n. pudendus exit the pelvic cavity through the piriform opening. In addition, n. pudendus, internal arteries and the veins enter the ischiorectal fossa through the lesser sciatic foramen.
Together with them, they go into the gluteal region longbranches of the sacral plexus - n. ischiadicus and n.cutaneus femoris posterior and are sent to the piriform opening with the lower gluteal vessels.
Inferior hypogastric plexus, plexus hypogastricus inferior, - a vegetative plexus, including post-nodal sympathetic branches, parasympathetic nodes and sensory fibers for innervation of the pelvic organs. It descends in the form of a plate from the sacrum to the bladder.
Lymphatic vessels and regional lymph nodes.
Groups of lymph nodes: along the external and common iliac arteries (from the free lower limb; along the internal iliac artery (from the pelvic organs).; behind the rectal (from the sacrum, coccyx).
lymph outflow in the pelvis is carried out through three groups of nodes. The first is located along the internal iliac vessels: nodi iliaci interni. It collects lymph from the pelvic organs. The second group - nodi iliaci externi et communes, is located along the outer and common iliac arteries. They receive lymph from the lower limb, the lower parts of the abdominal wall, the superficial layers of the perineum, from the external genitalia. The third group - sacral nodes, nodi sacrales, collects lymph from the back wall of the pelvis and from the rectum. The nodes lying in the bifurcation of the common iliac arteries are called interiliac, nodi interiliaci. They receive lymph from both the pelvic organs and the lower limb.
Male pelvic organs.
Topography of the bladder.
The bladder is located in anterior section small pelvis, behind the pubic bones and symphysis, when filled, the bladder in an adult goes beyond the pelvic cavity, rising above the pubic bones. It distinguishes the top, body, bottom and neck. The wall of the bladder has well-defined muscular and submucosal layers. There are no folds and submucosal layer in the bottom of the bladder, the mucous membrane fuses with the muscular membrane. Here a triangular platform is formed, trigonum vesicae, or Lieta triangle. The peritoneum, passing from the anterior abdominal wall to the bladder, forms a transverse fold and covers a very small part of the anterior wall, upper and posterior walls. Passing from the back wall to the rectum, the peritoneum forms the vesico-rectal fold and the vesico-rectal recess, excavatio rectovesicale.
In the subperitoneal region, the bladder has a pronounced visceral fascia of its own. Between the wall of the bladder and the fascia in the perivesical space in a well-defined layer of loose fiber is the venous network of the bladder.
Syntopy of the bladder.
The anterior surface of the bladder, covered by the visceral fascia, is adjacent to upper branches pubic bones and pubic symphysis, separated from them by a layer of loose connective tissue of the retropubic (pre-vesical) cellular space. The ampullae of the vas deferens, the seminal glands, the terminal sections of the ureters and the fascia rectoprostatica (septum rectovesicale) are adjacent to the posterior surface of the bladder.
The vas deferens and the ureters crossing them from below and outside adjoin the lateral surfaces of the bladder for some length. From above and from the sides to the bladder, the loops of a thin, sigmoid, and sometimes transverse colon or caecum with a appendix separated from it by the peritoneum are adjacent. The bottom of the bladder is located on the prostate.
Bladder blood supply. It is carried out from the system a. iliaca interna. One or two a. vesicalis superior most often depart from the non-obliterated part of a. umbilicalis, a. vesicalis inferior - directly from the front trunk a. iliaca interna or from the obturator artery.
Bladder veins form a network in the visceral cellular space of the bladder. From there the blood is sent to venous plexus bladder and prostate, located in the retropubic space. Further, the blood flows into v. iliaca interna.
Lymph drainage from the bladder. It is carried out in nodi lymphoidei iliaci, located along the external iliac arteries and veins, and in nodi lymphoidei iliaci interni and sacrales.
Bladder innervation. The upper and lower hypogastric nerve plexuses, the pelvic splanchnic nerves and the pudendal nerve, which form on the walls of the bladder and especially at the confluence of the ureters and around them, the plexus vesicalis take part in the innervation of the bladder.
Children's features.
In newborns and young children, the topography of the pelvic organs is significantly different from that in adults. The bladder is mostly located above the symphysis, its anterior wall is not covered by the peritoneum and is adjacent to the anterior abdominal wall. The urinary duct runs from the upper wall of the bladder to the navel. The latter quickly becomes empty and obliterated, turning into a connective tissue cord. With the age of the child, an increase in the pelvic cavity occurs and the bladder, as it were, descends and, in an emptied state, is located in the cavity of the small pelvis behind the pubic joint.
Topography of the ureters.
Ureter - paired organ, has 3 narrowings along its length: at the beginning of the ureter, at the place where the abdominal part of the ureter passes into the pelvic part, and at the place where it flows into the bladder.
The pelvic section of the ureter, which is approximately half of its length, starts from the border line of the pelvis. At the level of this line, the left ureter crosses the common iliac artery, and the right ureter crosses the external iliac artery.
Further, the ureter is located on the side wall of the pelvis in the lateral cellular space medially from the nerve trunks and internal iliac vessels of the pelvis and laterally from the rectum. Then the ureter crosses the obturator neurovascular bundle and the beginning of the umbilical artery and goes medially to the bottom of the bladder.
Here the ureter passes between the posterior wall of the bladder and the anterolateral wall of the ampulla of the rectum and crosses at right angles to the ductus deferens, located outward from it and anterior to the seminal glands.
blood supply the pelvic ureters is carried out from aa. rectales mediae and aa. vesicales inferiores.
Deoxygenated blood flows into vv. testiculares and vv. iliacae internae.
Pelvic ureters innervated from the upper and lower hypogastric plexuses, and in the lower part they receive parasympathetic innervation from nn. splanchnici pelvini.
lymph outflow from the pelvic ureters occurs in the iliac lymph nodes.
Topography of the prostate.
The prostate consists of 30-50 glands, forming substantia glandularis, and a muscular substance, substantia muscularis, representing the stroma of the gland. The glands through the ductuli prostatici open into the prostatic part of the urethra. The prostate is located in the subperitoneal floor of the small pelvis. It has a cone-shaped shape and is directed downward, towards the urogenital diaphragm. The base of the prostate is located under the bottom of the bladder. The prostate has two lobes and an isthmus. The prostate has a visceral fascial capsule, capsula prostatica (Pirogov-Retzia), from which to pubic bones go mm. (ligg.) puboprostatica.
Syntopy of the prostate.
Above the prostate are the bottom of the bladder, the seminal glands and the ampullae of the vas deferens. Below is the urogenital diaphragm, in front is the posterior surface of the pubic symphysis, behind is the Denonville-Salishchev fascia rectoprostatica and the ampulla of the rectum. The prostate is easy to feel through the rectum.
Blood supply to the prostate carried out by branches from aa. vesicales inferiores and aa. rectales mediae (from a. iliaca interna). Vienna form a venous plexus, plexus prostaticus, which merges with the plexus vesicalis; further blood flows into v. iliaca interna.
innervation carry out branches of the lower hypogastric plexus.
lymph outflow from the prostate is carried out in The lymph nodes located along a. iliaca interna, a. iliaca externa and on the pelvic surface of the sacrum.
Topography of the vas deferens.
The pelvic section of the vas deferens is located in the subperitoneal floor of the small pelvis, divided into parietal, intermediate, and cystic. This part is located in the retrovesical cellular space.
Coming out of the deep inguinal ring, the vas deferens, first accompanied by the artery of the same name, and then leaving it, goes around from outside to inside and down a. epigastric inferior. Rounding a. et v. iliacae externae, the vas deferens is directed medially and backwards into the lateral space of the pelvis. Here it crosses the obturator neurovascular bundle, the umbilical artery, and the superior cystic arteries.
Located medially from these vessels, the vas deferens reaches the side wall of the bladder, then passes between the ureter and the posterior surface of the bladder, forming the ampulla of the vas deferens, ampulla ductus deferentis. On the back wall of the bladder, the ampoule is located medially from the ureter and seminal gland.
The duct of the ampoule, merging with the duct of the seminal gland, ductus excretorius, forms the ejaculatory duct, ductus ejaculatorius, which penetrates the prostate and opens to seed tubercle into the prostate urethra. The vas deferens are supplied with blood from a. ductus deferentis.
Topography of the seminal glands.
They are saccular protrusions outside of the terminal sections of the ductus deferens. They are surrounded by the visceral fascia and are located between the posterior wall of the bladder and the anterior wall of the ampulla recti.
Syntopy of the seminal glands.
In front of the glands are the posterior wall of the bladder and the final section of the ureters. Medially, they are adjacent to the vas deferens with ampullae. Lower divisions glands lie at the base of the prostate, and the superomedial sections are covered by the peritoneum, through which they come into contact with the loops of the intestine.
blood supply seminal glands is carried out by aa. vesicalis inferior et rectalis media. The veins drain into the plexus vesicalis.
Innervated inferior hypogastric plexuses.
Lymph drainage from the seminal glands goes through the lymphatic vessels of the bladder to the lymph nodes located along the iliac arteries and on the sacrum.
Children's features.
In boys, the prostate gland and seminal vesicles are also located relatively high compared to their position in adults.
Topography of the rectum.
The rectum (rectum) is a continuation of the sigmoid colon and is located within the small pelvis at the anterior surface of the sacrum.
The rectum ends at the level of the pelvic diaphragm (m. levator ani), where it passes into the canalis analis. The length of the rectum is 10-12 cm.
In the rectum, the supraampullary part and the ampulla are isolated. supraampullary part and upper half ampoules are located in the upper, peritoneal floor of the small pelvis. The lower half of the ampulla of the rectum is located in the subperitoneal floor of the pelvis and instead of the peritoneum is covered with visceral fascia (Amyusse capsule).
The pelvic part of the rectum, in accordance with the curvature of the sacrum and coccyx, forms a bend directed backward by a bulge, nexura sacralis. At the transition to canalis analis, the final section of the rectum deviates downward and backward, forming a second bend, anal-rectal, flexura anorectalis (flexura perinealis), facing forward with a bulge.
The rectum makes three bends in the frontal plane. These include the upper right lateral bend, flexura superodextra lateralis, the intermediate left lateral bend, flexura intermediosinistra lateralis, the lower right lateral bend, flexura inferodextra lateralis.
Layers of the rectum- muscular membrane (consists of the outer longitudinal, stratum longitudinale, and the inner circular, stratum circulare, layers).
At the level of the pelvic diaphragm above the fibers of the external sphincter, m. sphincter ani externus, m fibers are woven into the muscles of the rectum. levator ani, in particular m. puboanalis, etc. puborectalis.
mucous membrane upper division ampulla of the rectum forms 2-4 transverse folds that do not disappear when the rectum is filled, plicae transversae
recti, having a helical course. In the ampullar part there is one fold on the right wall, two on the left.
Syntopy of the rectum.
In the subperitoneal floor anterior to the rectum are the posterior wall of the bladder not covered by the peritoneum, the prostate, the ampullae of the vas deferens, the seminal glands (vesicles) and the terminal sections of the ureters. The rectum is separated from them by Denonville-Salishchev's fascia rectoprostatica (septum rectovesicale). On the sides of the ampulla are the branches of the internal iliac vessels and the nerves of the plexus hypogastricus inferior. Behind the rectum adjoins the sacrum. .
Blood supply: a. rectalis superior (unpaired - terminal branch of the lower mesenteric artery) and a. rectalis media (steam room, from a. iliaca interna). .
Venous return: veins form a venous plexus, plexus venosus rectalis, in the wall of the rectum, in which the submucosal and subfascial parts are isolated. From the upper sections, the blood flows through v. rectalis superior, which is the beginning of v. mesenterica inferior (portal vein system). All veins anastomose widely among themselves and with the veins of other pelvic organs. Thus, there is one of the portocaval anastomoses here.
In innervation the lower mesenteric, upper and lower hypogastric plexus and pelvic splanchnic nerves take part. As part of the sacral spinal nerves are sensory nerves that convey the feeling of filling the rectum.
lymph outflow from the nadampular part of the rectum and partly from the upper part of the ampulla through the nodi pararectales along the superior rectal artery to the nodi rectales superiores and further to the nodi mesenterici inferiores. This explains the possibility of spread of cancer metastases along the rectum. From the subperitoneal region of the rectum, lymph flows to the internal iliac and sacral lymph nodes.
Children's features.
The rectum in newborns is located high, expanded and its curves are weakly expressed. It is adjacent to the ureters, bladder and vagina (in girls), prostate and seminal vesicles (in boys). With the growth and development of the child, the topographic and anatomical relations of the rectum approach those in adults.
Organs female pelvis.
Topography of the bladder in women.
The bladder in the female pelvis lies deeper in the pelvic cavity than in men. In the peritoneal floor, behind the bladder of women, the body of the uterus and loops of the intestine, which enter the excavatio vesicouterine, are adjacent. In the subperitoneal floor, the bladder adjoins the pubic symphysis with its front surface and is fixed to it by the pubic-vesical muscles (ligaments), mm. (ligg.) pubovesicalia. Back wall bladder lies anterior to the cervix and vagina. The bubble is firmly connected with the vagina, separating from it only with an insignificant layer of fiber, with the uterus the union is more loose. The bottom of the bladder is located on the urogenital diaphragm. Laterally adjacent to it m. levator ani.
At the bottom of the bladder in women, in front of the anterior wall of the vagina, the ureters flow into it.
The lymphatic vessels of the bladder in women are connected with the lymphatic vessels of the uterus and vagina at the base of the broad ligament of the uterus.
Topography of the uterus and its appendages.
The uterus is located in the small pelvis between the bladder in front and the rectum in the back. It consists of two sections: the upper one - the body, corpus, and the bottom, fundus, and the lower one - the cervix, cervix uteri. In the neck, supravaginal and vaginal parts, portio supravaginalis and portio vaginalis are distinguished.
On portio vaginalis cervicis there is an opening of the uterus, ostium uteri, limited in front of labium anterius and behind labium posterius. This hole connects the vagina through the canalis cervicis uteri with the uterine cavity, cavum uteri. The lateral edges of the uterus are called margo uteri dexter et sinister. For the most part, the uterus is located in the upper, peritoneal, floor of the small pelvis.
Suspension apparatus uterus. Formed by round and wide ligaments of the uterus, ligg. teres uteri and ligg. lata uteri. The broad ligaments of the uterus are a duplication of the peritoneum. They depart from the uterus almost in the frontal plane and reach the peritoneum of the side walls of the pelvis. In this place, the peritoneal sheets of the broad ligament form the suspensory ligament of the ovary, lig. suspensorium ovarii, containing the vessels of the ovary (a. et v. ovarica). Down and back from the angle of the uterus in the thickness of the broad ligament departs own bundle ovary, lig. ovarii proprium. Down and anteriorly from the angle of the uterus, the round ligament of the uterus, lig. teres uteri.
The uterus has a visceral fascia. Muscular fibrous bundles of the main ligament of the uterus, lig. cardinale. Ligaments attached to the visceral fascia: cardinal ligaments, ligg. cardinalia, recto-uterine, ligg. rectouterina, pubocervical. ligg. pubocervicale
The pubic-vaginal muscle, m. Pubovaginalis; urethrovaginal sphincter, m. sphincter urethrovaginalis and perineal membrane, membrana perinei.
blood supply carried out by two uterine arteries, aa. Uterinae, ovarian arteries, aa. ovaricae (from abdominal aorta), and the arteries of the round ligament of the uterus, aa. lig. teretis uteri. A. Uterina is a branch of the internal iliac artery. Venous outflow from the uterus occurs first in the uterine venous plexus, plexus venosus uterinus. It widely anastomoses with all the veins of the pelvis, but primarily with the venous plexus of the vagina, plexus venosus vaginalis. From the plexus, blood flows through the uterine veins into the internal iliac veins.
Outflow from the bottom of the uterus, ovaries and tubes occurs in the inferior vena cava through vv. ovaricae.
Innervation of the uterus carried out by an extensive uterovaginal nerve plexus, plexus uterovaginalis - the middle section of the paired lower hypogastric plexus, plexus hypogastricus inferior.
lymph outflow from the uterus from the visceral parauterine and paravaginal nodes (nodi parauterini et paravaginales), the lymph flows into the iliac lymph nodes and further into the common iliac nodes. Along the way ligg. cardinalia from the cervix, lymphatic vessels carry lymph to the obturator lymph nodes, and then to the external and common iliac nodes. From the bottom of the uterus along the outlet lymphatic vessels the round ligament of the uterus, the lymph partially flows to the inguinal lymph nodes.
The fallopian tubes.
Fallopian tube, tuba uterina, or Fallopian tube- a paired organ that connects the uterine cavity with the peritoneal cavity. It is located along the upper edge of the broad ligament of the uterus and has a mesentery, mesosalpinx, which is part of the broad ligament just below the tube.
Diameter fallopian tube varies and ranges from 5 to 10 mm. In the tube, the uterine part, pars uterina, with the uterine opening, ostium uterinum, isthmus, isthmus, ampulla, ampulla, and funnel, infundibulum are distinguished. The funnel of the fallopian tube has fringes, fimbriae, bordering the abdominal opening of the tube, ostium abdominale tubae uterinae. One of the fimbriae, approaching the tubal end of the ovary, is called fimbria ovarica.
blood supply The fallopian tubes originate from the ovarian and uterine arteries
Ovaries. Ovary - women's steam room gonad measuring 1.5 x 1.5 x 1.0 cm. It is covered with germinal epithelium. The transition of the epithelium into the endothelium of the peritoneum is marked with a whitish line. In this place, the mesentery of the ovary ends, mesovarium, extending from the posterior leaf of the broad ligament of the uterus.
The ovary has two ends - tubal and uterine, two surfaces - medial and lateral, two edges - free and mesenteric. The ovary is attached to the posterior surface of the broad ligament of the uterus near the side wall of the pelvis. Under the peritoneal cover, a. approaches the ovary. ovarica from the retroperitoneal space. The uterine end of the ovary is connected with the body of the uterus through the connective tissue of the ovary's own ligament, lig. ovarii proprium.
blood supply ovary is carried out by a. ovarica, extending from the abdominal part of the aorta at the level of the 1st lumbar vertebra, as well as the ovarian branch of the uterine artery.
Outflow of venous blood from the ovary occurs through v. ovarica dextra directly into the inferior vena cava, through v. ovarica sinistra - first to the left renal vein and through it into the lower hollow.
In innervation ovary involved branches of the lower hypogastric plexus.
Lymph drainage from the ovary is carried out along the efferent lymphatic vessels accompanying the ovarian artery, to the lymph nodes located around the aorta, and to the iliac lymph nodes.
Children's features.
In newborn girls, the uterus is located above the plane of entry into the small pelvis. She has not finished her development and her body is 1/3, and the cervix is 2/3 of the entire length.
The ovaries are located near the boundary line of the pelvis. With age, the uterus and ovaries descend, and by the age of 12-14 they occupy a position corresponding to their position in women. By this age, the size of the uterus increases and the length of its body and cervix becomes the same.
Topography of the rectum in women.
The structure, division into sections, blood supply and innervation of the rectum in women do not differ from those in men. Only the syntopy and lymph drainage of the rectum in women differ.
In the peritoneal floor anterior to the rectum in women, the body, cervix and posterior fornix of the vagina are located. Between the rectum and the posterior wall of the body of the uterus there are loops descending from the lower floor of the abdominal cavity small intestine. They enter the recto-uterine cavity, excavatio rectouterina. In the subperitoneal floor, the rectum in women is adjacent to the vagina in front. However, they are separated by the fascia rectovaginalis. This fascia is rather thin and loose, it is penetrated by lymphatic vessels, so that it does not become an obstacle either to the spread of metastases in tumors of both organs, or to the development of rectovaginal fistulas.
Malformations genitourinary system in children.
Cysts of the urinary duct (urachus). They are formed with incomplete obliteration and sometimes have a fistulous tract that opens in the navel area - vesico-umbilical fistulas. Also to congenital fistulas includes vesico-intestinal fistulas, which are extremely rare. They usually occur between the rectum and the area of the bladder triangle, sometimes combined with atresia. anus.
In addition, in girls, ectopic laying of endometrial elements can occur in the urinary duct. In these cases, during puberty during the menstrual period, cysts filled with blood can form in the cord left from the urinary duct. In the presence of a fistulous tract, blood may be released from the navel.
Bladder exstrophy. This malformation is characterized by the absence of the anterior wall of the bladder and part of the anterior abdominal wall. The bladder is open anteriorly, the mucosa, according to the defect of the bladder wall, is fused with the edges of the skin defect. The pinholes of the ureters are clearly visible on the posterior wall of the bladder mucosa. Urine continuously flows out of them.
Hypospadias is a malformation characterized by the absence of part of the lower wall of the urethra.
Epispadias - underdevelopment of the upper wall of the urethra.
Malformations of the rectum.
Atresia of the anus, atresia ani. With this defect, there is no anus and the rectum ends blindly close to the skin of the perineum. The bowel is usually distended with accumulated meconium.
With atresia of the rectum, atresia recti, the anus is represented by a pronounced depression, but the rectum is short and blindly ends above the bottom of the small pelvis. In this case, the blind end of the rectum is separated from the perineum by a significant layer of tissue.
With atresia of the anus and rectum, atresia ani et recti, which occurs more often than other malformations, the anus remains closed, and the rectum ends blindly at different distances from the pelvic floor.
Topography of the perineum.
Borders, areas.
Perineum (region perinealis), forming the lower wall of the pelvic cavity, has the shape of a rhombus and is limited in front by the pubic symphysis, in front and laterally by the lower branch of the pubis and the branch of the ischium, laterally by the ischial tuberosities, laterally and posteriorly by the sacrotuberous ligaments, and posteriorly by the coccyx. A line connecting the ischial tuberosities (linea biischiadica) . the perineum is divided into the urogenital and anal regions. The tendon center of the perineum is usually projected into the middle of the line connecting the ischial tubercles.
Layers of regions and their characteristics.
The layered structure of the anal area in men and women is almost the same. In the center of the anal region is the anal opening of the direct kateshka, anus.
1 .Leather(derma) at the anus it is pigmented, thinner than along the periphery of the region, and fused with the subcutaneous part of the external sphincter of the anus, as a result of which it forms folds, and then passes into the mucous membrane of the rectum. In men, between the root of the scrotum and the anus is the perineal suture, raphe perinei.
2. Subcutaneous adipose tissue And superficialfascia of the anal area (panniculusadiposusfascia perinei superficialis) better expressed than the genitourinary. In the fiber are the skin branches of the lower gluteal and lower rectal arteries and the subcutaneous venous network, which is especially thickened near the anus. Innervate the skin of the branch nn. rectales inferiores from n. pudendus in the medial parts of the region and rr. perineales from n. cutaneus femoris posterior in the lateral sections.

