Ischemic heart disease: types and clinical picture. Classification, manifestations, outcomes of ischemia
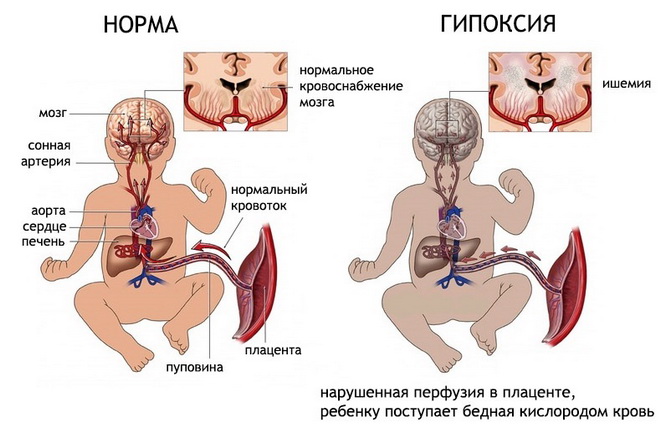
Ischemia- violation peripheral circulation, which is based on the restriction or complete cessation of the inflow arterial blood.
Clinic: blanching of the organ area, decrease in temperature, impaired sensitivity in the form of paresthesia, pain syndrome, decrease in blood flow velocity, decrease in organ volume, decrease blood pressure in the area of the artery located below the obstacle, a decrease in tissue turgor, dysfunction of an organ or tissue, dystrophic changes.
Classification of ischemia by etiology:
A) compression ischemia occurs when the afferent artery is compressed by a scar, tumor, etc.;
B) obstructive ischemia occurs when the lumen of the artery is partially or completely closed by a thrombus or embolus. Inflammatory and productive-infiltrative changes in the artery wall in atherosclerosis, obliterating endarteritis, periarteritis nodosum also leads to local blood flow restriction by the type of obstructive ischemia;
C) angiospastic ischemia occurs due to irritation of the vasoconstrictor apparatus of the vessels and their reflex spasm.
Causes of ischemia
Reasons: emotions (fear, pain, anger), physical factors(cold, injury), chemical agents, biological irritants (toxins), etc.
Angiospasm leads to a slowdown in blood flow up to its complete stop.
Develops most often by type of vascular unconditioned reflexes from the corresponding interoreceptors. It may also have a conditioned reflex character.
Irritation of the vasomotor center with toxins, mechanical irritation of subcortical structures that regulate vascular tone, the presence of pathological process in area diencephalon also often lead to pronounced angiospastic phenomena.
In the development of angiospastic ischemia, not only irritation various departments reflex arc, but also the functional state of the muscle fibers of the vascular wall, electrolyte and other types of metabolism in it.
For example, sodium ions, accumulating in the muscle fibers of the vessel, increase its sensitivity to pressor substances - catecholamines, vasopressin and angiotensin.
The nature of all types of changes in the ischemic tissue or organ is determined by the degree oxygen starvation, the severity of which depends on the rate of development and type of ischemia, its duration, localization, nature collateral circulation, functional state organ or tissue.
Ischemia is vital important organs has more severe consequences. Brain, heart are characterized high level energy metabolism, but, despite this, their collateral vessels are functionally absolutely or relatively incapable of compensating for circulatory disorders. Skeletal muscles and especially connective tissue, thanks to low level energy metabolism in them, are more stable in conditions of ischemia.
Ischemia in conditions of increased functional activity organ or tissue is more dangerous than at rest.
Changes in tissues during ischemia:
The first structural changes occur in mitochondria. Their swelling, the disappearance of cysts, the disintegration of mitochondria and the endoplasmic reticulum and cell nuclei can result in the formation of a focus of necrosis - a heart attack. It occurs in organs hypersensitivity to oxygen starvation and insufficient network of collaterals.
In the ischemic area, there is an enhanced biosynthesis of connective tissue components.
Stasis is the slowing down and stopping of blood flow.
Types of stasis:
A) true (occurs due to pathological changes in capillaries or disorders rheological properties blood);
B) ischemic (occurs due to the complete cessation of blood flow from the arteries);
B) venous.
Venous and ischemic stasis is the result of a simple slowing and stopping of blood flow.
Elimination of the cause of stasis leads to the restoration of normal blood flow. progression of ischemic and venous stasis contributes to the development of truth.
Causes of true stasis: physical (cold, heat), chemical, biological (bacterial toxins).
Mechanisms for the development of stasis: intracapillary aggregation of erythrocytes and, as a result, an increase in peripheral resistance. Importance in the pathogenesis of true stasis, it is attached to a slowdown in blood flow in the capillary vessels due to thickening of the blood. The leading role is played by the increased permeability of the capillary wall under the influence of biologically active substances to shift the reaction of the medium to the acid side.
Increased permeability vascular wall and vasodilation leads to thickening of the blood, slowing of blood flow, aggregation of red blood cells and stasis.
Thrombosis is a lifelong learning process inner surface walls of vessels of blood clots, consisting of its elements. Thrombi can be parietal and obstructive.
Depending on which components predominate in the structure of a thrombus, there are:
A) red (erythrocytes predominate);
B) white (a thrombus is formed by platelets, leukocytes, plasma proteins);
C) mixed thrombi.
The most common cause of thrombosis are diseases in which the vascular wall is affected:
Diseases of an inflammatory nature (rheumatism, syphilis, typhus);
Atherosclerosis;
Cardiac ischemia;
allergic processes.
inadequate supply of oxygen to the heart muscle coronary atherosclerosis, can lead to a violation of the mechanical, biochemical and electrical functions of the myocardium. sudden development ischemia usually affects the function of the myocardium of the left ventricle, which leads to disruption of the processes of relaxation and contraction. Due to the fact that the subendocardial sections of the myocardium are less well supplied with blood, ischemia of these areas develops in the first place. Ischemia involving large segments of the left ventricle leads to the development of transient insufficiency of the latter. If ischemia also captures the region of the papillary muscles, then it can be complicated by insufficiency of the left atrioventricular valve. If ischemia is transient, it is manifested by the occurrence of an angina attack. With prolonged ischemia, myocardial necrosis may occur, which may or may not be accompanied by a clinical picture. acute infarction myocardium. Coronary atherosclerosis is local process which can cause ischemia varying degrees. Focal left ventricular contractility disorders resulting from ischemia cause segmental bulging or dyskinesia and may to a large extent reduce the pumping function of the myocardium.
Based on the above mechanical disturbances lies wide range changes in cell metabolism, their function and structure. In the presence of oxygen, the normal myocardium metabolizes fatty acid and glucose into carbon dioxide and water. Under conditions of oxygen deficiency, fatty acids cannot be oxidized, and glucose is converted to lactate; The pH inside the cell decreases. In the myocardium, the reserves of high-energy phosphates, adenosine triphosphate (ATP) and creatine phosphate are reduced. Impaired function cell membranes leads to a lack of K ions and absorption of Na ions by myocytes. Whether these changes are reversible or whether they lead to the development of myocardial necrosis depends on the degree and duration of the imbalance between myocardial oxygen supply and demand.
With ischemia, the electrical properties of the heart are also disturbed. The most characteristic early electrocardiographic changes are repolarization disturbances, which are wave inversions. T, a later - segment offset ST(ch. 178). Transient segmental depression ST often reflects subendocardial ischemia, while transient segment elevation ST, is considered to be a consequence of more severe transmural ischemia. In addition, due to myocardial ischemia, its electrical instability occurs, which can lead to the development ventricular tachycardia or ventricular fibrillation (ch. 184).
state of microcirculation. Local manifestations and consequences.
infarction due to ischemia.
Ischemia - a decrease in blood supply to an organ or tissue as a result of difficulty in the flow of blood through the afferent vessels.
Causes of increased resistance to blood flow in the arteries - 3 (three) groups of reasons:
Compression (compression from the outside) afferent vessels (tumor, scar, ligature, foreign body). Such ischemia is called compression.
Obturation of afferent vessels - as a result of complete or partial closure from the inside of the lumen of the artery by a thrombus or embolus.
Angiospasm of the afferent arteries - as a result of vasoconstriction of vascular smooth muscles. Mechanisms of arterial spasm: a) extracellular - associated with prolonged circulation of vasoconstrictor substances in the blood. These are: catecholamines, serotonin; b) membrane - associated with a violation of the process of repolarization of membranes of smooth muscle cells; c) intracellular - intracellular transport of calcium ions is disturbed, hence the non-relaxing contraction of smooth muscle cells.
Microcirculation during ischemia.
reduced due to a decrease in hydrostatic pressure in the arterial part of the channel.
Blood flow resistance in the arterial part of the channel is increased due to the obstruction of blood flow in the leading arteries.
Volumetric blood flow velocity reduced by reducing the arteriovenous pressure difference and increasing resistance to blood flow.
Linear blood flow velocity reduced due to a decrease in arteriovenous pressure difference and increased resistance to blood flow.
reduced due to the closure of part of the functioning capillaries.
ischemia symptoms.
Reduction in diameter and quantity visible arterial vessels due to their narrowing and reduced blood supply.
Paleness of tissues or organs due to a decrease in blood supply and a decrease in the number of functioning capillaries.
Decreased arterial pulsation as a result of their filling with blood.
Lowering the temperature of the ischemic tissue or organ a consequence of a decrease in the influx of warm arterial blood, further a decrease in metabolism.
Decreased lymph formation as a result of a decrease in perfusion pressure in tissue microvessels.
Decreased volume and turgor of tissues and organs due to insufficiency of their blood and lymph filling.
consequences of ischemia. The main pathogenetic factor of ischemia is hypoxia. In the future: reduction of under-oxidized products, ions, biologically active substances. It follows from this:
Reduced specific functions.
Decreased non-specific functions and processes: local defensive reactions, lymph formation, plastic processes.
The development of dystrophic processes, tissue hypotrophy and atrophy.
Necrosis and infarction.
The significance of the level of tissue and organ functioning, shunting and collateral circulation in the outcome of ischemia. infarction due to ischemia.
The nature of the consequences of ischemia depends on:
The rate of development of ischemia. The higher it is, the more significant the degree of tissue damage.
The diameter of the damaged artery or arteriole.
"Sensitivity" of the organ to ischemia. This sensitivity is especially high in the brain, kidneys, and heart.
The values of the ischemic organ or tissue for the body.
The degree of development of collateral vessels and the rate of "turning on" or activation of collateral blood flow in a tissue or organ. Under collateral blood flow understand the circulatory system in the vessels around the ischemic tissue area and in itself. A number of factors contribute to its inclusion, namely: a) the presence of a blood pressure gradient above and below the narrowed area; b) accumulation in the ischemic zone of biologically active substances with a vasodilating effect (adenosine, Ax, prostaglandins, kinins, etc.); c) "emergency" activation of local parasympathetic influences, contributing to the expansion of collateral arterioles; d) the degree of development of the vascular network in the affected organ or tissue.
5. Venous hyperemia. Definition, causes and mechanism of development.
Changes in microcirculation and hemodynamic parameters.
Manifestations, significance in pathology and consequences.
Venous hyperemia - this is an increase in blood supply to an organ or tissue due to a mechanical obstruction to outflow venous blood from an organ or tissue. This might be consequence:
Narrowing of the lumen of the venule or vein with her: a) compressions (edematous fluid, tumor, scar, tourniquet, etc.); b) obstruction (thrombus, embolus, tumor).
heart failure, when the heart does not pump blood from a large circle to a small one and central venous pressure in large veins rises.
With pathology of venous vessels, which is accompanied by low elasticity of the venous walls. This pathology is usually accompanied by the formation of extensions (varicose veins) and narrowing.
The mechanism of development of venous hyperemia. It consists in creating a mechanical obstacle to the outflow of venous blood from tissues and a violation of the laminar properties of blood.
Microcirculation changes.
Arteriovenous pressure difference reduced ha by increasing the hydrostatic pressure in the venous part of the channel.
Blood flow resistance in the venous part of the channel is increased due to the obstruction of blood flow in the outlet vessels.
Volumetric blood flow velocity reduced due to a decrease in arterio-venous pressure difference and increased resistance to blood flow.
Linear blood flow velocity reduced by reducing the arterio-venous pressure difference and increased resistance to blood flow.
Total cross-sectional area of the capillary bed increased due to the opening of a part of previously non-functioning capillaries.
Macrosymptoms of venous hyperemia.
Increase in the number and diameter of visible venous vessels due to the increase in their lumen.
Cyanosis of organs and tissues. The cyanotic shade is associated with: a) an increase in the amount of venous blood in them; b) an increase in the content of oxygen-free forms of hemoglobin in it (the result of a pronounced transition of oxygen into the tissues due to its slow current through the capillaries).
Lowering the temperature of organs and tissues due to: a) an increase in the volume of venous blood in them (in comparison with warmer arterial blood); b) decrease in the intensity of tissue metabolism.
Swelling of tissues and organs as a result of the increase blood pressure in capillaries, postcapillaries and venules. With prolonged venous hyperemia, edema is potentiated due to the "switching on" of osmotic, oncotic and membranogenic pathogenetic factors.
Hemorrhage into tissue or bleeding (internal and external) as a result of overstretching and microrupture of the walls of venous vessels.
Microsymptoms of venous hyperemia.
Increase in the diameter of capillaries, postcapillaries and venules.
Increase in the number of functioning capillaries on initial stage VH and decrease - at later stages, when blood flow stops in them due to the formation of microthrombi and aggregates of blood cells.
Deceleration of venous blood flow up to the complete cessation of the outflow.
Significant expansion of the axial cylinder of blood cells(up to the size of the lumen of the venules) and the disappearance of the "band" of the plasma current in them.
"Jerky" and "pendulum" movement of blood in venules. Hydrostatic pressure increases in front of the obstruction in the blocked vein. If its value reaches diastolic blood pressure, then during diastole ………………………….
Consequences and significance of venous hyperemia.
VG has a damaging effect on tissues. The main pathogenetic factor is hypoxia of the corresponding tissue or organ. Venous hyperemia is accompanied by tissue edema, often - hemorrhages or bleeding. Therefore, against the background of VG:
The specific functions of an organ or tissue are reduced.
Non-specific functions and processes are suppressed.
Hypotrophy and hypoplasia develop structural elements of cells and tissues.
Necrosis of the parenchyma and proliferation of connective tissue(sclerosis, scars).
Ischemia- violation of peripheral circulation, which is based on the restriction or complete cessation of arterial blood flow.
Clinic: blanching of an organ site, decrease in temperature, impaired sensitivity in the form of paresthesia, pain syndrome, decrease in blood flow velocity, reduction of an organ in volume, decrease in blood pressure in the area of the artery located below the obstacle, decrease in tissue turgor, dysfunction of an organ or tissue, dystrophic changes.
1. compression ischemia occurs when the afferent artery is compressed by a scar, tumor, etc.;
2. obstructive ischemia occurs when the lumen of an artery is partially or completely closed by a thrombus or embolus. Inflammatory and productive-infiltrative changes in the artery wall in atherosclerosis, obliterating endarteritis, periarteritis nodosum also leads to local blood flow restriction by the type of obstructive ischemia;
3. angiospastic ischemia occurs due to irritation of the vasoconstrictor apparatus of blood vessels and their reflex spasm.
Causes: emotions (fear, pain, anger), physical factors (cold, trauma), chemical agents, biological stimuli (toxins), etc.
Angiospasm leads to a slowdown in blood flow up to its complete stop.
It develops most often according to the type of vascular unconditioned reflexes from the corresponding interoreceptors. It may also have a conditioned reflex character.
Irritation of the vasomotor center with toxins, mechanical irritation of the subcortical formations that regulate vascular tone, the presence of a pathological process in the area of the diencephalon also often lead to pronounced angiospastic phenomena.
In the development of angiospastic ischemia, not only irritation of various parts of the reflex arc is important, but also the functional state of the muscle fibers of the vascular wall, electrolyte and other types of metabolism in it.
For example, sodium ions, accumulating in the muscle fibers of the vessel, increase its sensitivity to pressor substances - catecholamines, vasopressin and angiotensin.
The nature of all types of changes in the ischemic area of the tissue or organ is determined by the degree of oxygen starvation, the severity of which depends on the rate of development and type of ischemia, its duration, localization, the nature of the collateral circulation, and the functional state of the organ or tissue.
Ischemia of vital organs has more severe consequences. The brain and heart are characterized by a high level of energy metabolism, but, despite this, their collateral vessels are functionally absolutely or relatively unable to compensate for circulatory disorders. Skeletal muscles and especially connective tissue, due to the low level of energy metabolism in them, are more stable in conditions of ischemia.
Ischemia in conditions of increased functional activity of an organ or tissue is more dangerous than at rest.
Stasis, types, etiology, pathogenesis, signs.
Stasis- this is a slowdown, up to a complete stop, of blood flow in the vessels of the microvasculature.
Blood stasis may be preceded by venous plethora (congestive stasis) or ischemia (ischemic stasis).
Blood stasis is characterized by blood stopping in capillaries and venules with the expansion of the lumen and gluing of erythrocytes into homogeneous columns - this distinguishes stasis from venous hyperemia. Hemolysis and blood clotting does not occur.
Stasis must be differentiated from the "sludge phenomenon". Sludge is a phenomenon of erythrocytes sticking together not only in capillaries, but also in vessels of various calibers, including veins and arteries.
Stasis is a reversible phenomenon. Stasis is accompanied by dystrophic changes in the organs where it is observed. Irreversible stasis leads to necrosis.
Causes of stasis
Ischemia and venous hyperemia. They lead to stasis due to a significant slowdown in blood flow (during ischemia due to a decrease in arterial blood flow, with venous hyperemia as a result of slowing or stopping its outflow) and creating conditions for the formation and / or activation of substances that cause adhesion shaped elements blood, the formation of aggregates and blood clots from them.
Proaggregants are factors that cause aggregation and agglutination of blood cells.
Stasis pathogenesis
At the final stage of stasis there is always a process of aggregation and / or agglutination of blood cells, which leads to thickening of the blood and a decrease in its fluidity. This process is activated by proaggregants, cations and high molecular weight proteins.
All types of stasis are divided into primary and secondary.
Primary (true) stasis. The formation of stasis primarily begins with the activation of blood cells and the release of a large number of proaggregants and/or procoagulants. At the next stage, formed elements aggregate, agglutinate and attach to the wall of the microvessel. This causes a slowdown or cessation of blood flow in the vessels.
Secondary stasis (ischemic and congestive).
Ischemic stasis develops as an outcome of severe ischemia due to a decrease in arterial blood flow, a slowdown in the rate of its current, and its turbulent nature. This leads to aggregation and adhesion of blood cells.
Congestive (venous-congestive) variant of stasis is the result of slowing down the outflow of venous blood, thickening it, changing physical and chemical properties, damage to blood cells (in particular, due to hypoxia). Subsequently, blood cells adhere to each other and to the wall of microvessels.
Manifestations of stasis
With stasis are happening characteristic changes in the vessels of the microcirculatory bed:
Reducing the internal diameter of microvessels in ischemic stasis,
An increase in the lumen of the vessels of the microcirculatory bed with a stagnant variant of stasis,
A large number of aggregates of blood cells in the lumen of blood vessels and on their walls,
Microhemorrhages (more often with congestive stasis).
At the same time, manifestations of ischemia or venous hyperemia may overlap manifestations of stasis.
Consequences of stasis
With the rapid elimination of the cause of stasis, blood flow in the vessels of the microvasculature is restored and no significant changes develop in the tissues.
Prolonged stasis leads to the development dystrophic changes in tissues, often - to the death of a tissue or organ site (heart attack).
Any brain damage is accompanied by life-threatening organic change in his tissues. Oxygen starvation, insufficiency of incoming nutrients, manifested nearby characteristic symptoms determine the dynamics of the functioning of the brain, and the absence of a therapeutic effect in this case can lead to an aggravation of the process and the occurrence of serious side conditions. Cerebral ischemia caused by pathology blood vessels and capillaries in the tissues of the brain, is accompanied by a constantly ongoing progression of pathological processes in the tissues of the brain, which are accompanied by a significant deterioration in its blood supply.
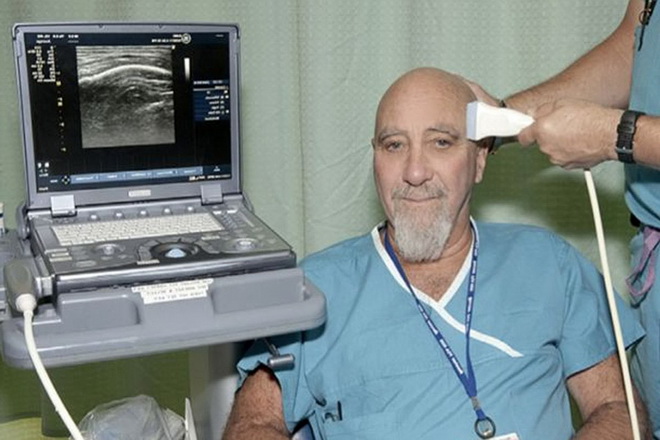
Having an idea of what cerebral ischemia is, what are its main manifestations and possible Negative consequences for health, can be diagnosed in a timely manner given state, conduct necessary treatment and keep your brain healthy. Since the main cause of this condition is organic lesion central (cerebral) vessels in the brain, it is their condition that should be considered the most indicative in the process of identifying the lesion in question. Indeed, it is precisely due to the violation of their integrity, the appearance of excessive permeability of the walls and the tendency to brittleness that increases the risk of possible side effects in the work of the brain, which are caused by manifestations of oxygen starvation and the absence required amount nutrients.
General description of the disease
A disease such as cerebrovascular ischemia has a certain classification depending on the stage of the pathological process, its prevalence and negative impact on brain tissue. Also negative impact exposed state of the nerve of the cerebellum, the anterior lobe of the brain responsible for the processes of memorization and long-term memory. All manifestations of this pathology manifest themselves in steps, the first stage is considered the most easily amenable therapeutic effect and therefore it is the first stage of the disease that must be detected as early as possible. Thanks to the presence characteristic manifestations cerebrovascular ischemia can be detected in time and treated.

Cerebrovascular ischemia in the photo
Today, according to medical statistics, cerebral ischemia occurs in more cases in the elderly (about 50-55% of all people over 65 years of age have one of the stages of this lesion) against the background of existing provoking diseases. Hypertension, gradually progressing, can gradually provoke a violation in the process of blood supply to the brain, which leads to the appearance of signs of the disease in question. It should be noted that cerebral ischemia is not amenable to complete cure, it is only possible to stop the rate of pathological processes occurring in the vessels of the brain, stabilization general condition patient and elimination of the most characteristic manifestations.
A chronic disorder in the process of blood circulation largely determines both the quality of the brain and the general condition of a person, because it is the brain that belongs to the target organs, which are primarily affected by the most severely manifested pathologies in the body. Therefore, even minor changes in the state of the brain, which have characteristic clinical manifestations(frequent headaches, abrupt shifts mood and memory difficulties) should be considered the first signs, and which must be paid close attention and begin an adequate therapeutic effect.
Development mechanism
The progression of the disease is in the following way: first, there is some deterioration in the functioning of the brain (the anterior lobe of the hypothalamus and cerebellum) due to the development of pathology of the cerebral (central) blood vessels, which are responsible for the process of supplying brain tissues with both oxygen and nutrients. In this case, there is often a lesion of the nerve connecting the brain (or parts of it) with the central nervous system, as a result of which there is a pronounced imbalance in his work. Then, as the disease progresses, an ever-increasing degenerative process in the brain is noted against the background of oxygen starvation, which leads to a gradual disruption of organic processes in its tissues.
In this case, pathological processes are first noted first transitory, and then chronic course in the brain. This condition is fraught with persistent manifestations of the current pathology. Characteristic features diseases draw attention to themselves and allow you to apply in time for an examination to a medical institution.
The main complication of this condition is high probability stroke, during the progression of the disease, the symptoms and manifestations of it negatively affect everyday life sick. Therefore, in order to prevent the occurrence serious consequences for the health and preservation of the life of the patient, it is recommended to begin treatment immediately after diagnosing this disease.
Symptoms of the disease
External manifestations are quite characteristic: frequent shifts moods, fluctuations in it - a sharp transition from positive attitude to a state of depression, fatigue, frequent depression and a decrease in the quality of the work of the intellect, as well as an increase in the degree of irritability, weakness during the day. Many patients experience a decrease in intelligence, which initial stages pathological process is imperceptible, however, as it progresses, it can seriously change a person's life - lower its quality.
In the absence of treatment, the listed manifestations are greatly aggravated: pain in the head becomes stronger, there is a deterioration in night sleep and fatigue throughout the day, short syncope and loss of performance.
Any deviations from the norm in the state of blood vessels provoke a qualitative change in the daily life of the patient, which immediately attracts attention and requires immediate attention. medical care. Home treatment of this lesion, especially in advanced stages, does not give a pronounced positive result and may be an adverse health delay in drug treatment resulting in an increased risk of negative complications.

Basic principles of disease classification
There are several various kinds classification of the disease in question. All of them are subdivided according to the degree of damage to brain tissues, the presence and number of symptoms, and the magnitude of manifestations. The most commonly used classification is according to the nature of the manifestations and the indicator of the impact on the patient's health. A classification based on the duration of the course of disorders caused by the current pathological process is also used.
The classification of the disease in accordance with the nature of the manifestations is as follows:
- transient variety - this condition is characterized by an ischemic attack or a cerebral crisis, in which there is a sharp change in the general condition with characteristic manifestations in the form of a prolonged and acute headache, decreased attention and concentration;
- acute phase of the disease, which should include hemorrhagic stroke, acute form encephalopathy and ischemic stroke and unspecified nature of occurrence;
- chronic course is characterized by manifestations of occlusion of blood vessels, cerebral thrombosis, subcortical encephalopathy. Chronic cerebral ischemia is accompanied by long-term preservation characteristic manifestations, a gradual deterioration in the general condition of the patient with an aggravation of the symptoms of the disease.
Cerebral ischemia 1 degree manifests itself at the initial stages of the pathological process. At the same time, the manifestations of the disease are not clearly expressed, the patient is characterized by sudden changes in mood, fatigue. Cerebral ischemia of the 1st degree is observed in many elderly people, its impact on everyday life is not very pronounced, which greatly hinders its timely diagnosis.
Cerebral ischemia of the 2nd degree- more advanced process clinical picture which is more pronounced. Headaches become permanent, there is a loss of concentration and the ability to concentrate. The second stage can also be characterized by a deterioration in the quality of night sleep, the appearance of unusual sensations during wakefulness: pain in the frontal lobe of the head, noise in the head for no apparent reason.
Cerebral ischemia 3 degrees has the most strong manifestation symptoms of the disease, there is a sharp decrease in the patient's performance. At the third stage of the development of the pathological process, he needs urgent hospitalization and active drug therapy.
There is also such a type of disease as ischemia spinal cord. At the same time, there is tissue damage in the adjacent area, insufficiency of blood supply to the spinal cord with a gradual deterioration in its functioning. For this disease, there is a similar classification that allows you to attribute the identified lesion to one of the classes, which allows you to quickly select the most appropriate treatment.
Causes
Causes of cerebrovascular ischemia can be different. They are mainly organic in nature, lesions of the heart and its accompanying illnesses often become a trigger for the occurrence of this pathology.
Most common causes cerebrovascular ischemia should be considered the following:
- thromboembolism of blood vessels;
- thrombosis of arteries and veins;
- heart defects, which can be both congenital and acquired;
- vasculitis;
- changes in the condition of the walls of blood vessels (their increased fragility and permeability)
- disturbances in the processes of blood clotting;
- metabolic disorders.
It is also necessary to highlight a number of risk factors that can provoke the disease.
One of the risk factors for the development of this pathology is long-term depressive states and stresses, which have an extremely negative effect on the processes of blood circulation in the brain tissues. Gout, advanced stages cervical osteochondrosis, smoking and frequent use alcoholic beverages should also be considered serious risk factors in the development of the pathology in question.
Among brain disorders it is by considering the disease that it occupies one of the first places in the number of probable side effects for health, therefore, when it is detected, a mandatory professional treatment with appropriate medicines and immediate hospitalization of the patient. Ischemic diseases also have a high degree of risk to the life of the patient: in case of untimely assistance or its insufficiency, the risk lethal outcome increases.

