How to improve placental blood circulation during pregnancy. Types of uteroplacental blood flow disorders, what they are, what to do
During pregnancy female body begins to rebuild. Therefore, during this period it is so important to keep the condition of both the woman and the fetus under control. According to medical statistics, a fairly large number of pregnant women experience impaired blood flow. Additional ones that arise in the body require constant monitoring by specialists. Its violation can lead to the death of the fetus, and this can happen at any stage of pregnancy. Let's try to figure out why blood flow is disrupted during pregnancy.
A little theory
Everyone knows that the placenta acts as a link between the woman’s body and the fetus. In this complex system, there are two types of blood circulation - placental and fetal. Any violation of one of them can lead to quite sad consequences, including the development of various diseases. Only a doctor can assess the severity of the problem.
In this case, a woman who is in the 30th week of pregnancy must undergo a special ultrasound diagnostics, in which the vessels of the placenta are clearly visible in a three-dimensional image. If there is any violation, the doctor will definitely see it, since there is a change in the spatial relationship of the uterine and fetal-placental circulation. This is very dangerous condition body, as oppression occurs respiratory function, and fetal development is suspended.
Degrees of impairment
Medicine distinguishes three degrees of severity of this pathology. The easiest is considered to be the first degree, when insufficient blood circulation has not yet reached its critical values. In this case, the fetal hemodynamics are in satisfactory condition. There is a violation of uteroplacental blood flow of 1 A degree and insufficient fetal-placental blood circulation of 1 B degree.
The second degree is characterized by a deterioration in the blood supply to the fetus. In 50% of cases, there is a decrease in the maximum speed of blood movement through all heart valves, and such a violation is observed both in the fetus and in the uterine arteries.
Quite often for short period time the second degree passes into the third. In this case, blood flow practically stops flowing to the fetus, which can cause hypoxia. There is a high probability of a decrease in diastolic blood flow in the aorta, and in some cases it may disappear completely.
Causes
If there is a 1st degree blood flow disorder during pregnancy, the reasons leading to this may be different. Numerous unfavorable factors are able to influence the placenta not only during its formation, but also at a later date. Medical practice distinguishes primary and secondary due to which the functioning of the placenta, which acts as a transport, protective, immune, metabolic and endocrine organ, is disrupted.
Thus, grade 1 A blood flow impairment during pregnancy can occur for the following reasons:
- uterine tumor;
- genetic defects;
- consequences of abortion;
- infectious diseases;
- hypertonic disease;
- diseases of the adrenal glands and thyroid gland;
- structural anomalies;
- hormonal dysfunctions;
- thrombosis, atherosclerosis;
- diabetes.

If this pathology is not eliminated in a timely manner, then after 6 weeks a slight disturbance in blood flow can progress to the third stage. If a problem is detected at 30 weeks, the doctor still has enough time to take appropriate measures to restore normal blood circulation.
Symptoms
Any pathology is characterized by its clinical picture, thanks to which the doctor can make an appropriate conclusion. Lack of hemodynamics leads to changes in the functioning of the placenta, which is why the fetus begins to suffer. The necessary supplies begin to arrive to him in limited quantities. nutrients and oxygen, and the excretion of metabolic products slows down. Signs begin to appear as a result of which intrauterine development is suspended.
Thus, if a blood flow disorder occurs during pregnancy, the symptoms of this condition manifest themselves as follows:
- cardiopalmus;
- decrease or increase in fetal motor activity;
- discrepancy between the volume of the abdomen and the specific stage of pregnancy.

Such signs usually occur in cases of decompensation. If the disorder uterine blood flow during pregnancy of 1 A or 1 B degree, these symptoms do not yet appear, since hemodynamics are compensated. It is usually detected during diagnostic studies.
Diagnostics
To identify a blood flow disorder of 1 A degree during pregnancy, it is necessary to undergo a series of examinations, with the help of which the type and degree of changes that have occurred are determined, and the condition of the fetus is determined. In this case, the doctor prescribes the following procedures:
- blood test for hormones such as estrogens, human chorionic gonadotropin, progesterone;
- cardiotocography;
- ultrasonography;
- Doppler.

In some cases, the doctor is already able to determine the disorder that has arisen during the examination, focusing on the child’s heart rate, which is calculated during auscultation. But the most reliable results usually obtained after laboratory and instrumental examination.
Treatment
Disrupted uteroplacental blood flow of any degree must be treated. Mostly therapeutic measures are aimed at preventing the pathology from further progressing. Hemodynamics are normalized only if a blood flow disorder of 1 B degree is detected.
During pregnancy with abnormalities, they are used various means, improving the condition of the fetus. Mainly used conservative methods treatment. Surgical intervention possible only in case of complications and life-threatening important indications. When normalizing blood flow disorders, a set of measures is used - pathogenetic, etiotropic and symptomatic treatment.
Drug treatment
Most often, grade 1 A blood flow disturbances during pregnancy are corrected with the help of medications. When identifying initial signs disorders are treated on an outpatient basis. More severe circulatory failure requires hospitalization in a hospital.

The following drugs are used for treatment:
- antispasmodics - “Eufillin”, “No-shpa”;
- vascular - "Actovegin";
- antiplatelet agents - "Curantil";
- vitamins and microelements - “Ascorbic acid”, “Magne B6”;
- hepatoprotectors - “Hofitol”, “Essentiale”;
- tocolytics - “Partusisten”, “Ginipral”;
- improving blood microcirculation - “Trental”;
- antihypoxants - “Instenon”;
- metabolic - "ATP".
Usually, to improve the condition, two courses of therapy are carried out - immediately after the diagnosis was made and at 32-34 weeks. After this, the doctor decides on the method of delivery. This is especially important if the circulatory disorder is severe. If blood flow is impaired to the 1st degree, childbirth is carried out naturally.
Surgery

If the blood flow disturbance is pronounced, emergency delivery is performed. In case of failure conservative treatment, even in case of lung violations, a decision is made within two days. Usually carried out C-section. If it is planned at a gestational age of less than 32 weeks, then the condition of the fetus and its viability are assessed.
Preventive measures
To avoid this pathological condition, as a blood flow disorder of 1 A degree during pregnancy, preventive measures should be taken. A woman who is expecting a baby should consume products containing essential vitamins, micro- and macroelements, fats, carbohydrates and proteins. Every day you should drink at least 1.5 liters of liquid, but only if swelling does not bother you.

It is also important to keep your weight under control. During pregnancy, the recommended weight gain should not exceed 10 kg. Women at risk are given prophylaxis with drugs to interact between the maternal and fetal body systems and prevent extreme dangerous dysfunction uteroplacental circulation. A timely adjusted method of labor management also plays an important role. But it should be remembered that even compliance with these measures does not exclude the occurrence of severe neurological complications.
Conclusion
Thus, it is important to control blood flow during pregnancy. The reasons may vary. The main thing is to look after your health, and timely detection pathology will help prevent severe consequences for the unborn child.
In this article we will talk about such an issue that worries many pregnant girls as a violation of the uteroplacental blood flow. Causes of circulatory disorders in the mother-fetus system, their symptoms, dangers similar violations and treatment options.
Disturbances of the uteroplacental blood flow are much more correctly called the term “disturbances of the utero-fetal blood flow”, since conditionally the blood circulation in the mother-fetus system can be divided into two components:
- Uteroplacental blood flow.
- Feto-placental blood flow.
Disturbances of blood flow in any of these systems or in both are immediately called in obstetrics disturbances of utero-fetal blood flow.
The conventional boundary between these two systems can be called the placenta - a temporary organ of pregnancy, formed by the ingrowth of chorionic villi of the embryo into the mucous membrane of the uterine wall. The placenta is a filter consisting of numerous interlacings of multi-level vessels in which maternal blood, without mixing with fetal blood, releases oxygen and nutrients into the fetal bloodstream, and takes back harmful substances and metabolic products.
The placenta is the most important organ for the fetus, which ensures its normal functioning
Let's try to understand this complex system of blood flow:
- From the side of the uterus, the placenta is fed by the maternal arteries - uterine arteries and spiral arteries. They are the constituent components of the first level of blood supply to the pregnant uterus and fetus.
- Spiral arteries feed the placenta, directly forming placental blood flow.
- The placenta forms the umbilical cord or umbilical cord - a complex of three vessels - two arteries and one vein, surrounded by a special jelly-like substance. By umbilical vein blood rich in oxygen and nutrients moves to umbilical ring the fetus, further supplying blood to the liver and other vital organs of the fetus. Blood flows in the umbilical vessels form the second component of blood circulation in the mother-fetus system.
- Large arteries of the fetus in the vital important organs– the aorta and cerebral artery form the third component of the blood circulation.
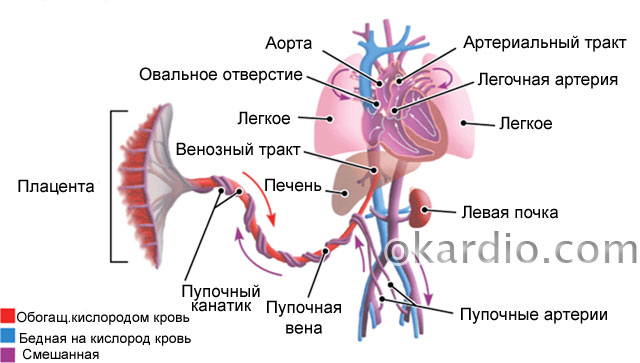 Fetal circulation. Click on photo to enlarge
Fetal circulation. Click on photo to enlarge If blood flow is disrupted at any level, the fetus does not receive enough nutrients and oxygen - intrauterine hypoxia of the fetus or its oxygen starvation. Intrauterine hypoxia can be either acute and quickly leading to fetal death, or chronic - long-term and sluggish, the main symptom of which is fetal growth retardation (abbreviated as FGR).
Depending on the severity and extent of blood flow disorders, the condition can be observed and treated conservatively (when it is not very dangerous) or the woman can be urgently delivered at any stage of pregnancy to save the life of the child.
The problem of blood flow disorders in the “mother-fetus” system is dealt with by obstetrician-gynecologists in close contact with perinatal ultrasound doctors, since the main function of determining immediate disorders and their degrees belongs to ultrasound doctors.
Causes of circulatory disorders in the mother-fetus system
- Disorders of placentation - the formation and functioning of the placenta. Such disorders can be primary - at the stage of pregnancy - placental abruption, lack of progesterone, defective uterine mucosa. The already formed placenta may also suffer. This is caused by disturbances in the coagulation system, infections, and trauma to the placenta.
- Coagulation system disorders - spontaneous and induced thrombosis. Blood clots block large and small branches of the vessels of the uterus and placenta.
- Intrauterine infections damage the placenta and trigger the formation of blood clots.
- Complications of pregnancy - Rh conflict, gestosis, twin steal syndrome, placental abruption, premature birth.
- Lack of nutrients and vitamins - in particular, iron deficiency - anemia.
- Maternal diseases - diabetes mellitus, hypertension, thrombophilia, vascular defects and vascular wall, heart and lung diseases.
- Impact harmful factors external environment – harmful conditions at work, the effect of drugs, smoking, alcoholism, drug addiction.
- Stress and nervous tension.
 Glucometer for measuring blood sugar levels. The presence of diabetes mellitus in the mother can lead to circulatory problems in the mother-fetus system
Glucometer for measuring blood sugar levels. The presence of diabetes mellitus in the mother can lead to circulatory problems in the mother-fetus system Main symptoms of the disease
These symptoms are called external because the main method for diagnosing disorders of placental and fetal blood flow is the ultrasound method with Doppler, which will be discussed below in a separate section.
How can one suspect fetal suffering before an ultrasound examination?
- Insufficient growth or complete absence increase in the main indicators of measurements of the pregnant woman’s abdomen at the next appointment - the height of the uterine fundus and abdominal circumference. It is these two sizes that the doctor measures with a centimeter tape every visit to the pregnant woman.
- Unsatisfactory results of listening to the fetal heart by a doctor during examination. Each examination of the expectant mother is accompanied by listening to the fetal heart sounds using a special tube - an obstetric stethoscope. If the doctor notes a change in the fetal heart rate, muffled tones, or lack of response of heart contractions to movements, then this should alert the doctor.
- Unfavorable fetal movement profile. This symptom is clearly noted by the woman herself. A pregnant woman may complain of weakening movements, long periods of “silence” of the fetus, or excessively violent movements. The simplest test for motor activity The fetus will have a “Count to Ten” test. In this case, a pregnant woman must count at least 10 separate fetal movements within 12 hours.
- Unfavorable or alarming types of CTG - cardiotocography. This procedure for recording the electrical activity of the fetal heart is carried out every appointment. antenatal clinic, starting from 28–30 weeks. CTG is a very sensitive method for assessing the condition of the fetus, therefore, in case of cardiotocogram abnormalities, a mandatory ultrasound examination of the fetus and its blood flow is necessary.
These are four main points at which there are objective reasons to suspect one or another violation of the blood supply to the uterus and fetus. There are also relative readings to conduct additional diagnostic measures regarding utero-fetal blood flow:
- Multiple pregnancy, especially in the presence of monochorionic twins. Such twins share one placenta, so the latter often cannot cope with such a load, especially in late pregnancy.
- Anomalies in the structure of the placenta - placental hypoplasia, roll-shaped placenta, as well as its premature aging.
- Abnormalities in the structure of the umbilical cord or its presence true nodes– such nodes are formed when the fetus actively moves.
- The presence of intrauterine infection - viral, bacterial or others.
- Rh conflict between mother and fetus based on Rh factor or blood group. Such a conflict is primarily diagnosed by the presence of antibodies in the mother’s blood.
- Maternal gestational diabetes mellitus that developed during an existing pregnancy, or pre-existing diabetes mellitus.
- Preeclampsia is a complication of late pregnancy, characterized by increased blood pressure, swelling and the appearance of protein in the urine.
- Maternal hypertension.
- Any cardiac or vascular pathologies mother.
- Blood clotting disorders - especially a tendency to thrombosis. Such disorders include hereditary thrombophilias and antiphospholipid syndrome.
All these factors significantly increase the risk of developing blood flow disorders in the mother-fetus system, and therefore are subject to close monitoring.
 Cardiotocography can be used to evaluate the fetal heartbeat at rest, during movement, and during uterine contractions.
Cardiotocography can be used to evaluate the fetal heartbeat at rest, during movement, and during uterine contractions. Diagnosis of blood flow disorders
The gold standard for diagnosing perinatal blood flow disorders is ultrasound examination of the fetus with mandatory Doppler measurements. The Doppler method is based on measuring velocities, resistance indices and other indicators of blood flow in vessels. The global medical community has developed great amount tables and diagrams of Doppler measurements of each vessel.
In obstetrics, fetal circulation is assessed using the following vessels:
- Uterine arteries – assessment of the first link of the “mother-fetus” system. Close attention to the indicators of the uterine arteries is paid to pregnant women with heart and vascular diseases, anemia, arterial hypertension, gestosis and gestational diabetes mellitus.
- Umbilical cord vessels - assessment of the mother-fetus system - indicators of blood flow coming from the placenta to the child. The most commonly assessed blood flow indicators are the umbilical artery.
- The middle or median cerebral artery is a powerful vessel in the fetal brain. Indicators of blood flow in this vessel are extremely important and significant in the presence of a conflict in the Rh system or blood groups, fetal anemia, as well as in cases of suspected fetal malformations.
The doctor measures blood flow indicators several times and correlates the obtained values with tables. These are extremely variable indicators; they can fluctuate significantly depending on external and internal factors:
- Gestation period is up to one week.
- The number of fetuses and placentas – twins and triplets have their own Doppler measurements.
- Mother's blood pressure - the ultrasound doctor is always interested in the pregnant woman's blood pressure numbers.
- Maternal hemoglobin level - with anemia, blood flow indicators can change significantly.
- Smoking and other bad habits of the mother.
- Medicines.
- Uterine tone - both normal hypertonicity and regular contractions, for example, during childbirth.
 Uterine tone (hypertonicity) – contraction of the muscular layer of the uterus
Uterine tone (hypertonicity) – contraction of the muscular layer of the uterus In addition to Doppler measurements, the doctor performs so-called fetometry - measuring the size of the fetus and calculating its estimated weight. If the fetus is significantly delayed in development from the average, the doctor has the right to make a diagnosis of “fetal growth restriction,” or FGR. A similar delay in fetal growth is observed with chronic hypoxia - that is, the fetus does not receive enough oxygen and nutrients for a long time– several weeks and even months.
Based on the obtained indicators, the ultrasound diagnostic doctor forms a diagnosis: “Impaired utero-fetal blood flow” and indicates the degree. In the presence of fetal growth restriction, the diagnosis is supplemented by the formulation “FGR”.
Now we will talk in detail about the classification of the degrees of blood flow disorders.
Three degrees of pathology
There are three main degrees of disturbances of utero-fetal blood flow:
- I degree – minor disturbances in one of the conditional circulatory systems. The first degree has two subdegrees:
- I A - disturbances of uteroplacental blood flow with preserved fetoplacental blood flow. This means a violation of blood circulation in the uterine artery system.
- I B - violation of feto-placental blood flow with preserved uteroplacental blood flow. In this case, the uterine arteries fully perform their function, but there are disturbances at the post-placental level.
Treatment of fetal-uterine blood flow disorders
Almost all degrees of blood flow disorders require mandatory treatment. The question is what degree of blood flow disturbances is detected, and whether it is accompanied by fetal growth retardation.
The most “harmless” are disturbances of uteroplacental blood flow at grade 1a. It is important to understand that this type of disorder is sometimes an accidental finding during the next ultrasound. This condition can occur against the background of increased blood pressure in the mother, her anxiety, fatigue, or decreased hemoglobin levels. This degree does not always indicate fetal suffering and often goes away on its own within a few hours after resting or going for a walk. fresh air. However, this does not mean that you need to “give up” on the diagnosis. A pregnant woman should definitely undergo a control ultrasound after 5–7 days, and record CTG several times during the week.
Basic methods of treating fetal blood flow disorders:
- Normalization of the lifestyle and nutrition of a pregnant woman. It is important to walk a lot in the fresh air, sleep at least 8 hours at night and try to rest for at least an hour during the day, avoid sitting for a long time V uncomfortable position, move a lot, eat normally and nutritiously.
- Blood pressure control is one of the most important parameters determining uterine blood flow. In the presence of arterial hypertension You need to constantly take medications prescribed by your doctor and monitor your blood pressure readings yourself.
- Treatment of intrauterine infection antiviral drugs and antibiotics.
- Treatment of extragenital pathology - normalization of sugar levels, normalization of hemoglobin levels, body weight control, correction of the blood coagulation system. The latter includes taking medications low molecular weight heparins– Fragmina, Fraxiparina and others.
- The use of antispasmodics - No-shpy, Drotaverine, Papaverine. These drugs relax the wall of the uterus and spiral arteries, increasing blood flow.
- Taking magnesium supplements - magnesium has a relaxing effect on the uterine wall and a powerful protective effect on the central nervous system fetus The last factor is important in the development of hypoxia.
- The use of “vascular” drugs – large group disaggregants, angioprotectors and drugs that improve microcirculation and tissue trophism. The most common drugs in obstetrics are Pentoxifylline, Dipyridamole, Actovegin and their derivatives.
- In case of Rh conflict, plasmapheresis is prescribed - purification of the mother's blood using a special device to reduce the amount of antibodies damaging the fetal red blood cells.
- In case of acute fetal hypoxia against the background of blood flow disorders II and III degree, inefficiency conservative therapy, as well as severe fetal growth retardation, early delivery is advisable, regardless of the gestational age. Most often, they resort to a cesarean section, since induction of labor is an additional burden on the already suffering fetus. The principle “outside is better than inside” is perfect for these situations.
The placenta is formed in the uterus after pregnancy. It is necessary to connect the body of mother and child with one blood circulation. With the help of the placenta, oxygen and nutrients necessary for the development and formation of organs are delivered to the fetus. IN reverse side unnecessary substances formed as a result of biochemical processes are eliminated.
Impaired uteroplacental blood flow causes a condition called placental insufficiency. This leads to fetal death and miscarriage.
For 36 weeks, three mandatory ultrasound examinations are performed. It allows you to promptly identify the disorder, develop a plan for managing pregnancy and childbirth, prescribe treatment, and prevent the death and abnormal development of the child.
Modern requirements of obstetricians and gynecologists are aimed at examining pregnant women using safe methods to assess uteroplacental blood flow by volume.
How does blood circulation function between mother and fetus?
The mother-fetus circulatory system is based on such anatomical formations, like the placenta, umbilical arteries, veins.
Blood enters the placenta through the uterine arteries. The structure of their walls is distinguished by the presence of a muscle layer that can contract and block the lumen. Before pregnancy occurs, this mechanism helps reduce blood loss during menstruation.
At 4–5 weeks of consolidation of the fertilized egg (gestation process), the muscle layer disappears. Blood flow to the placenta no longer depends on vascular contraction. And by the sixteenth week, the arteries are transformed for constant blood supply. This turns out to be dangerous when bleeding occurs, since it is impossible to stop it by reducing the lumen of the vessels.
IN normal conditions the placenta is attached to inner surface uterus with the help of villi, penetrating deep into the thickness of the mucosa. They grow into the walls of blood vessels and come into direct contact with maternal blood.
What happens here at the cellular level:
- exchange between the maternal body and the fetal bloodstream;
- two differently directed flows meet;
- transition is taking place necessary substances(diffusion).
The other part general circulation provide the vessels of the umbilical cord (normally there are 2 arteries and a vein). The main volume of blood flows to the fetus through the arteries, and flows through the veins towards the placenta.

As the uterus grows, the arteries expand and form anastomoses.
Violation of fetal-placental blood flow is most difficult to tolerate developing child. Creates conditions for unsatisfactory construction forecast internal organs and systems, birth healthy baby.
What reasons can break the blood flow between the mother, placenta and fetus?
The causes of disruption of the circulatory system between the maternal body and the fetus (fetoplacental insufficiency) have been well studied. Some factors are formed only during pregnancy. The other one depends on general health women.
Pregnancy pathologies include:
- Low attachment of the placenta (obstetricians say previa, “placentation”) - lower sections uteruses are thinner muscle layer. Through it, not enough blood flows to the fetus. A similar situation develops in the case of presentation in the area postoperative scar(for example, from a caesarean section).
- Late toxicosis - accompanied by damage small vessels uterus, the complication is the most frequent violation blood flow
- Anemia - low level hemoglobin causes a compensatory acceleration of the heartbeat, and blood flow through the uterine arteries increases to compensate for the lack of oxygen. Circulation also changes in the uteroplacental circle.
- Incompatibility between the blood of mother and fetus according to Rh - an immune conflict arises with the development hemolytic disease child, anemia. The same situation is possible when transfusion of different blood types from a donor.
- The load on the kidneys due to toxicosis can cause an increase in blood pressure. This helps change blood flow.
- Pathology of the umbilical cord arteries is rarely detected. If there is only one umbilical artery, then there is insufficient blood flow to the fetus.
- Multiple pregnancy - the placenta is increased in size and requires increased nutrition. Sometimes blood flow changes from one fetus to another.

It turns out that the first child is a constant donor for the twin, develops worse, because he transfers blood to his brother, and he himself is “malnourished”
Such changes are called fetotransfusion syndrome. The donor has a lower body weight. And the recipient develops increased load on the developing heart. Both kids have problems.
The most dangerous diseases for women are:
- Acute infections during pregnancy - pathogens can penetrate the placental barrier and destroy the vascular network.
- Malformations of the uterus - the most significant is the “bicornuate” uterus. Inside the cavity there is a partition dividing it into 2 parts. Pregnancy is possible only in one of them. The main violation is not the compression factor (the cavity has the ability to stretch sufficiently), but the lack of communication between the uterine arteries, insufficient development of the vascular network, and placental hypoxia.
- Endometriosis - changes in the inner lining of the uterus that occur after inflammatory diseases(including sexually transmitted infections), frequent abortions, diagnostic curettage. One of the reasons is smoking and alcohol.
- Tumor of the uterus - if a woman has even a small fibroid ( benign tumor), then pregnancy stimulates the growth of nodes. They take over part of the blood supply, and the fetal blood flow is “robbed.” Failure directly depends on the size of the tumor.
- Diabetes mellitus - affects the walls of blood vessels, often occurs in women with risk factors during pregnancy.
How does insufficient placental blood supply threaten the fetus?
All disorders of both uteroplacental and fetal placental nature lead to oxygen deficiency fetus (hypoxia). Complications are caused precisely by this mechanism:
- the formation of the internal organs of the fetus is disrupted, there is a lack of mass, this is called “delay intrauterine development»;
- the heart reacts with rapid contractions (tachycardia) or arrhythmias, bradycardia;
- the composition of electrolytes and acid-base balance are disrupted;
- functioning is disrupted endocrine system, the fetus experiences a hormonal imbalance;
- fat depots are not formed.
The most severe complications- fetal death, threat of termination of pregnancy.

Myomatous nodes take away part of the vascular network from the fetus for its growth
Types of blood flow disorders in the placenta
There are fetoplacental (between the fetus and placenta) insufficiency and uteroplacental insufficiency.
Fetoplacental hypoxia can occur as:
- Acute failure- Occurs during any period of pregnancy and during labor. Calls premature detachment placenta, vascular thrombosis, infarction in the placenta area, hemorrhage. Capable of causing the death of a child.
- Chronic - occurs more often, develops from the second trimester, but manifests itself only in the third. Changes in the placenta are premature aging, fibrin is deposited on the surface of the villi. Permeability is sharply reduced, which provokes fetal hypoxia.
Against the background of the development of chronic placental insufficiency, the following stages can be distinguished:
- compensation - the course is favorable, because they work defense mechanisms the mother's body and compensate the baby for missing nutrition, the treatment is effective, the child is born on time, healthy;
- subcompensation - the maternal body is not able to fully compensate for the “unprofitable” blood supply to the fetus, it is necessary full treatment, the child may be born with complications, developmentally delayed;
- decompensation - pathology develops rapidly, compensatory mechanisms are insufficient, the fetus’s heart activity is disrupted, intrauterine death is possible;
- critical stage- characterized by pronounced structural changes in the placenta, which disrupts its functions, therapy cannot change the condition of the fetus, death is inevitable.
Degrees of impaired blood flow
In the joint violation of fetoplacental and uteroplacental blood flow, 3 degrees are distinguished.
I - changes are compensated, do not threaten the fetus, affect only the uteroplacental blood flow, the child develops normally. Depending on the level of changes, there are:
- degree Ia - disturbance of uteroplacental blood flow is limited to one of the uterine arteries, all hemodynamic parameters are stable, within normal limits;
- degree Ib - blood flow is disrupted at the level of communication between the fetus and the placenta due to the vessels of the umbilical cord; enough blood flows through the uterine arteries.
If minor changes in the first stage were not detected and the woman did not receive treatment, then after 3-4 weeks, second-degree disorders occur.
II - blood flow in the uterine and umbilical arteries changes.
III - indicators are critical, reverse blood flow in the arteries is possible.
How is diagnosis carried out?
Most accurately helps to place correct diagnosis and identify the level of impaired blood flow using Doppler ultrasound. The method is highly sensitive and very informative. Shows even small changes in the first stage to clinical manifestations. An important advantage is safety for the fetus and the expectant mother.
Using Dopplerography, it is possible to examine blood flow through arteries and veins, obtain a color graphic image, and measure fetal hemodynamics.
This plays a significant role in predicting the course of pregnancy and creates conditions for making decisions on treatment measures.
TO indirect methods diagnostics include:
- computed tomography,
The methods allow us to identify lack of fetal weight and placental dysfunction. These signs may be evidence of the development of hypoxia.
What does the mother feel and what does the doctor determine during the examination?
Hypoxia stimulates fetal motor activity.
At an appointment with an obstetrician-gynecologist, the doctor listens to the fetal heartbeat and pays attention to high frequency, arrhythmia or bradycardia. This necessitates referral for Doppler examination.

A pregnant woman pays attention to increased movements, tremors
Treatment of disorders
Establishing the degree of impaired uteroplacental blood flow is necessary for choosing pregnancy management tactics.
- It is believed that it is possible to maintain a pregnancy in the first degree (a and b); treatment will also help.
- The second degree is considered borderline, requiring constant monitoring; the effectiveness of treatment is unlikely.
- In the third degree, urgent delivery using surgical methods is required.
Treatment options are aimed at all parts of the pathology:
- to improve microcirculation, use Pentoxifylline, Actovegin;
- to support low blood flow speed and pressure in the vessels, Stabizol, Venofundin, Infucol are used (synthesized on the basis of a starch solution, capable of retaining fluid in the vessels);
- vasodilators medicines such as Eufillin, No-shpa eliminate spasm of medium and small arteries;
- by reducing the tone of the uterus, it is possible to influence vasospasm, reduce the degree of hypoxia, use magnesium sulfate, Magne B6, Ginipral;
- antioxidants eliminate the effects of hypoxia, destroy breakdown products, prescribe Tocopherol, combinations of vitamin E and ascorbic acid, Hofitol;
- Essentiale provides protective effect by increasing the level of beneficial phospholipids in the blood, improving liver function;
- Curantil is prescribed during pregnancy against the background of uterine fibroids, it has been established positive action on microcirculation and prevention of thrombosis.
Obstetricians continue to use Cocarboxylase in practice, which cardiologists have abandoned. But gynecologists consider the drug effective for restoring tissue respiration.

Incubators are used for the treatment and care of newborns as indicated.
Forecast and consequences
For statistical research An indicator such as “perinatal mortality” is used. It includes all deaths occurring in a fetus from the 22nd week of pregnancy and among newborns in the first week of life. It is believed that it fully reflects the influence of the factor of pregnancy and childbirth. The calculation is per 1000 children born.
Currently, 13.3% of children die from the second degree of disturbance of the uteroplacental circulation, and up to 47% in the third degree. Timely caesarean section reduces mortality.
IN intensive care need:
- 35.5% of newborns with the first degree;
- 45.5% – from the second;
- 88.2% - from the third.
The consequences of preserving and treating children born in conditions of pathological hypoxia. Pediatricians and psychiatrists point to its unconditional influence on physical and mental development.
Diagnosis and treatment of conditions associated with disruption of the uteroplacental barrier can only be carried out by experienced specialists. Cannot be taken on your own medications or use advice from poorly educated people. The situation can become critical not only for the fetus, but also for the woman.
A clearly functioning “mother-placenta-baby” system is the key to the health of a woman expecting a new addition to the family and her baby. A failure in this system, resulting in impaired blood flow, can lead to negative consequences for a child, the reversibility of which is often simply impossible. Violation is fraught with delayed development of the fetus in the womb. The consequences of impaired blood flow during pregnancy also include hypoxia, malformations and even embryonic death.
An additional circle of blood circulation in a pregnant woman requires additional examination by a specialist. This examination is called Doppler ultrasound. Doppler is an ultrasound diagnosis of the intensity of blood flow in different vessels. Diagnosis is carried out in the third trimester of pregnancy. It is at this time that Doppler shows almost 100% reliable results. In some cases, Doppler measurements are performed at twenty weeks.
By comparing the information received on the device and guided by blood flow standards, the diagnostician determines whether the child is experiencing oxygen starvation or not.
Doppler testing has its own approved standards, which include: index of vascular resistance of the uterus, umbilical cord, aorta and cerebral artery fetus Self-decoding and comparing the data obtained after diagnosis and Doppler measurements is a thankless task. Only a doctor can calculate the vascular resistance index using the appropriate formula.

What should you do if the doctor, having deciphered the Doppler data and compared it with the norms, notes a violation of the blood flow of the pregnant woman? Well, definitely don’t panic and don’t get nervous. It won't be good for the child either. Timely treatment is quite effective in combating blood flow diseases.
Blood circulation disorders blood vessels during pregnancy vary in severity.
In the first degree, blood flow disturbance does not reach critical values. The fetal hemodynamics are positive.
The hemodynamics of the fetus in the second degree of the disease is impaired. Half the time maximum speed blood movement through all heart valves is reduced. In this case, blood flow is disrupted both in the child and in the arteries of the uterus of the expectant mother. In a very short period, the second degree can develop into the third.
The third degree is destructive for the child. Her diagnosis states critical condition blood supply to the fetus. Intracardiac hemodynamics at this stage there are profound changes. Fetal hypoxia is most likely in this case.

Can a pregnant woman experience blood flow problems? There are certain symptoms. But, for example, in the first stage, placental insufficiency does not manifest itself in any way. It can only be diagnosed by ultrasound. A second degree symptom is a change in the baby’s behavior. He is either too active or, conversely, inactive. Secondary signs of blood flow disease may include protein excretion in the urine, insufficient or excessive amounts of amniotic fluid, swelling, gestosis (late toxicosis), pressure surges, sudden weight gain.
Bloody discharge from birth canal- most danger sign disorders associated with placental abruption. In this situation, only ambulance specialists.

The consequences of impaired blood flow are very sad if treatment is not prescribed in time. This is at least spicy or chronic hypoxia, as well as intrauterine growth retardation. More severe complications: premature birth; pregnancy fading; miscarriage; development congenital pathologies, including those incompatible with life; intrauterine fetal death.
To prevent the disastrous consequences of impaired blood flow, we need, first of all, thorough prevention.
In order for the baby to be fully nourished, a woman must consume a balanced diet during pregnancy. These are products with maximum possible number vitamins and microelements. High-quality proteins, carbohydrates and fats. Frequent consumption of water (more than one liter) is also required. Except in cases where the expectant mother is prone to swelling.

Prevention of blood flow disorders involves monitoring weight changes during pregnancy. An increase of more than 10 kg by the end of pregnancy is considered excessive.
If a pregnant woman is at risk (under 17 years of age or over 36 years of age; with bad habits; having chronic diseases etc.), then prevention should include taking medications, preventing blood flow diseases.
A woman who dreams of becoming the mother of a healthy baby in the future should, already during pregnancy planning, analyze her lifestyle and, if possible, eliminate potential risks.
Video on the topic of the article

