Topographic anatomy of the perineum. Medical Encyclopedia - Perineum
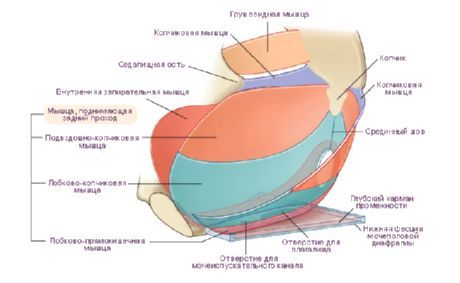
perineum, perineum, is called the area bounded in front by the pubic symphysis; behind - the tip of the coccyx; on the sides - ischial tubercles and sacro-hump ligaments. With the legs abducted and bent, it resembles the shape of a rhombus, the sides of which are formed in front by the branches of the pubic and, and behind - by the sacrospinous ligaments, which are covered by the lower edges of the large sciatic muscles. In the middle of the perineum in the sagittal direction, there is a tendon suture, raphe perinealis, which in men passes into a suture.
The perineum is the lower wall of the body, it closes the small pelvis from below, the urethra passes through it, and in women. It prevents prolapse of the pelvic organs, promotes the retention of urine, feces, controls urination and defecation. Knowledge of the topographic and anatomical features of the structure of the female perineum must be taken into account during surgical intervention for perineal ruptures during childbirth.
The segment of the perineum, located between the posterior commissure of the labia majora and the otkhodnikov hole, is called the perineum in the narrow sense of the word, or the obstetric perineum.
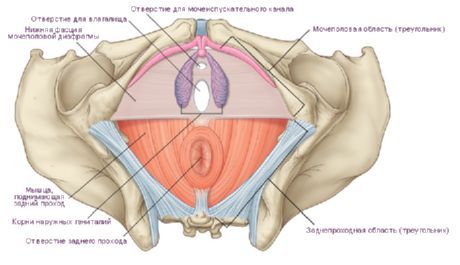
The perineum is divided by a horizontal line into two sections, or two triangles: anterior and posterior. front triangle, or urinary-genital area, regio urogenital, filled with urinary-genital diaphragm, diaphragma urogenital, which is located frontally. It is represented by a dense muscular-fascial plate, which consists of a deep transverse muscle of the perineum and two fascial sheets that cover the muscles from above and below. ahead urethra the diaphragm does not reach the pubic fusion, but forms a dense transverse ligament of the perineum, lig. transversum perinei. The space between the transverse ligament and the arcuate ligament of the pubic fusion is the site of passage of the artery (clitoris) and v. dorsalis penis et v. clitoridis.
The posterior triangle, or anal region, regio analis, is filled with the pelvic diaphragm, diaphragma pelvicum, which is located horizontally. It is formed by the right and left muscles that lift the anus, and located behind them by the right and left coccygeal muscles and fasciae. The rectum passes through the pelvic diaphragm and opens with the anus. In men, the urethra passes through the urinary-genital diaphragm, and there is also the scrotum and the root of the penis, and in women, the vagina and external genitalia.
Perineal muscles
The urinary-genital and pelvic diaphragm is represented by muscles that form two layers: superficial and deep.Muscles of the urinary-genital diaphragm: Superficial muscles:
- Bulbous spongy muscle, m. bulbospongiosus;
- Ischiocavernosus muscle, m. ischocavernosus;
- Superficial transverse muscle, m. transversus perinei superficialis.
Deep muscles:
- Deep transverse muscle of the perineum, m. transversus perinei profundus-,
- Muscle-closure of the urethra, m. sphincter urethrae.
bulbospongiosus muscle, m. bulbospongiosus, - steam room, covers the lower lateral surface, bulbis penis, and the spongy body and fuses with the same muscle of the opposite side, forming a longitudinal seam, raphe. Bulbous
spongy muscle compresses the urethra and promotes the excretion of urine and sperm. In the female m. bulbospongiosus is divided into two adjacent halves, it limits and narrows the opening of the vagina.
Ischiocavernosus muscle, m. ischiocavemosus, - originates from the ischial tuberosity of the right and left sides and is attached to the cavernous body. The ischiocavernosus muscle compresses the venous vessels of the penis or clitoris and promotes erection.
Superficial transverse muscle, m. transversus perinei superficial, - a small steam room, located on the border between both diaphragms, originates from the ischial tuberosity on the right and left sides and is directed to the tendon center, which strengthens it.
Deep transverse perineal muscle, m. transversus perinei profundus. - It is a flat muscle covering the membranous part of the urethra. It originates from the ischial tubercles and proximal parts of the ischial bones, goes to the midline, where it forms a tendon suture. The deep transverse perineal muscle strengthens the urogenital diaphragm. The urethra and vagina pass through it. In the area where the urethra passes through the muscle, part of the fibers of the deep perineal muscle forms around it the urethra closing muscle, m. sphincter mduae, which is an arbitrary sphincter.
deep muscles- levator muscle anus, m. levator ani]
- Coccygeal muscle, m. coccygeus.
Muscle that lifts the anus, m. levator ani, - flat, triangular in shape, goes back to the descending part of the pubic bone, the fascia of the obturator internus muscle and the pelvic surface of the ischial spine. One part of the muscle fibers goes back, limits the rectum and fuses with the bundles of the opposite side. The second part of the muscle fibers runs from the side and, and in women, the vagina. Muscle fibers are intertwined with muscles Bladder and vagina, are sent back, where they attach to the coccyx and anal-coccygeal ligament.
coccyx muscle, m. coccygeus, - located in the posterior region pelvic diaphragm. It originates from the ischial spine and sacrospinous ligaments and is attached to the lateral edge of the sacrum and coccyx.
Muscles of the pelvic diaphragm: Superficial muscles
- Muscle-closure of the anus external, m. sphincter ane externus.
Muscle-posterior posterior external, m. sphincter ane externus, - refers to the superficial muscles of the pelvic diaphragm. It is located around the anal above m. levator ane. The muscle is an external arbitrary contactor of the anal, closes it. Muscle bundles, m. sphincter ane extemus, form a semi-oval. The superficial bundles end in the subcutaneous tissue, the bundles of which originate from the coccyx and end in the tendon center, and the deepest ones surround the anal and adjacent to m. levator ane.
Fascia of the pelvis and perineum
The walls of the pelvic cavity, cavitas pelvis, and the pelvic organs are covered with fascia. There are the following fascias:- Pelvic fascia, fascia pelvis-,
- Parietal fascia of the pelvis, fascia pelvis parietalis;
- Visceral fascia of the pelvis, fascia pelvis visceralis-,
- Peritoneal-perineal fascia, peritoneo-perinealis-,
- Upper fascia of the pelvic diaphragm, fascia diaphragmatis pelvis superior,
- Lower fascia of the pelvic diaphragm, fascia diaphragmatis pelvis inferior,
- Superior fascia of the urogenital diaphragm, fascia diaphragmatis urogenital is superior,
- Lower fascia of the urogenital diaphragm, fascia diaphragmatis urogenitalis inferior;
- Superficial fascia of the perineum, fascia perinei superficialis.
pelvic fascia, fascia pelvis, - is a continuation of fascia iliaca, and is divided into two sheets: the parietal fascia of the pelvis, fascia pelvis parietalis, and the visceral fascia of the pelvis, fascia pelvis visceralis. The parietal sheet lines the walls and bottom of the pelvic cavity, and the visceral sheet lines the internal organs of the pelvis. The parietal fascia of the pelvis, fascia pelvis parietalis, passes to upper surface pelvic diaphragm and covers the posterior lift muscle from above. This part of the parietal fascia is called the upper fascia of the pelvic diaphragm, fascia diaphragmatis pelvis superior, it passes to the organs of the small pelvis and is called the visceral fascia of the small pelvis, fascia pelvis visceralis. Passing to the organs of the small pelvis, the pelvic fascia gives two spurs, which are located in the sagittal plane between the pubic bones and the sacrum. Thus, the pelvic organs are located in a space that is limited: in front - by the pubic bones; behind - the sacrum and coccyx, from the sides - the plates of the pelvic fascia. This space is divided by a partition located in the frontal plane into two sections: anterior and posterior. The septum is formed by the peritoneal-perineal fascia, fascia peritoneo-perinealis, or aponeurosis (Denovillier), it separates the rectum from the bladder and prostate.
Thus, in anterior section spaces in men are: bladder, prostate, seminal vesicles, vas deferens; and in women - the bladder and vagina, in the posterior section is the rectum. The pelvic organs occupy a central place and are separated from them, which is located in the spaces: spatium retropubicum and spatium retrorectale.
The lower surface of the pelvic diaphragm is covered by the lower fascia of the pelvic diaphragm, fascia diaphragmatis pelvis inferior. Thus, the muscles of the pelvic floor are limited to the superior and inferior fasciae of the pelvic diaphragm.
Superior and inferior fasciae of the urogenital diaphragm, fascia diaphragmatis urogenitalis superior et inferior, cover the front and back of the transverse deep muscle of the perineum, m. transversus perinei profundus et m. sphincter urethrae, and together form the urogenital diaphragm, diaphragma urogenital. In front, between the deep transverse perineal muscle and the fascia symphysis, they form the fibrous part of the urogenital diaphragm, which is called lig. transversum perinei. Anterior to this ligament is a. dorsalis penis v. dorsalis penis (clitoridis).
The superficial fascia of the perineum, fascia perinei superficial, covers the superficial muscles of the urogenital diaphragm: m. transversus perinei superficial, m. bulbospongiosus, m. ischiocavemosus, and together with the lower fascia of the urogenital diaphragm forms a vagina for the spongy bodies of the penis.
Ischioanal fossa, fossa ischioanalis, located laterally in the perineal region of the rectum. The fossa is filled with loose connective and adipose tissues, or a fatty body, corpus adiposum.
Ischioanal fossa, fossa ischioanalis, limited by such walls:
lateral - by the obturator internus muscle and its fascia; medial - by the muscle-elevator of the anal and its fascia; in front - the transverse superficial muscle of the perineum; behind - the lower edge of the large sciatic muscle and the external muscle-posterior anal. On the lateral wall of the ischio-anal fossa in the splitting of the fascia there is a genital canal, canalis pudendalis (Alcock canal), in which the neurovascular bundle formed by the genital artery, vein and nerve passes, this must be taken into account in surgical practice.
blood supply perineum is carried out by the internal pudendal artery, a. pudenda interna, which penetrates the ischio-anal fossa and gives branches to the skin and muscles of the anal. At the lower layer of the urogenital diaphragm, the internal pudendal artery branches into terminal branches that supply the penis with blood. Venous outflow from the perineum is carried out into the internal iliac vein.
Lymph flows from the perineum into the inguinal The lymph nodes, nodi lymphatici inguinales, inguinal lymph nodes, nodi lymphatici paravaginales, rectal lymph nodes, nodi lymphatici pararectales, lower gluteal, nodi lymphatici glutiales inferior, and sacral, nodi lymphatici sacrales.
innervation perineum is carried out by the pudendal nerve, n. pudendus, its branches: nn. restales inferiores, n. perinei, nn. scrotales (n. labiales), and coccygeal plexus, pl. coccygeus.
The perineum (perineum) is a complex of soft tissues (skin, muscles, fascia) that close the exit from the pelvic cavity.
The perineum occupies an area bounded in front by the lower edge of the pubic symphysis, behind by the tip of the coccyx, and on the sides by the lower branches of the pubic and ischial bones and ischial tubercles. If we take the ischial tubercles as the extreme lateral points of the perineum, in front - the lower point of the pubic symphysis, behind - the top of the coccyx, then the outlines of the perineum can be compared with a rhombus.
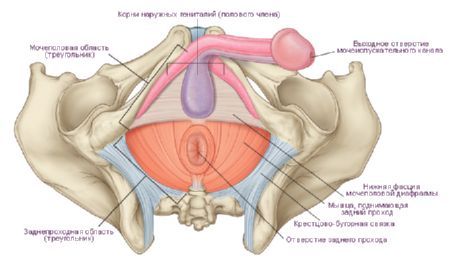
The transverse line connecting the ischial tuberosities divides this area into two parts, having the shape of triangles. anterior top part received the name of the urogenital region (regio urogenitalis), and the lower back - the anal region (regio analis). Within the urogenital region is the urogenital diaphragm, and in the anal region is the pelvic diaphragm. Both diaphragms are adjacent to each other with their bases, and the tops are directed, respectively, to the pubic symphysis and coccyx.
In a narrow sense, the perineum is understood as the area located between the external genital organs in front and anus behind. This area corresponds to the tendinous center of the perineum (centrum tendineum perinei). In women, this area extends from the posterior edge of the genital fissure to the anterior edge of the anus, and in men, from the posterior edge of the scrotum to the anterior edge of the anus. In the anteroposterior direction, a dark strip passes on the skin of the perineum - the median suture of the perineum (raphe perineum), which in men in front continues into the suture of the scrotum.
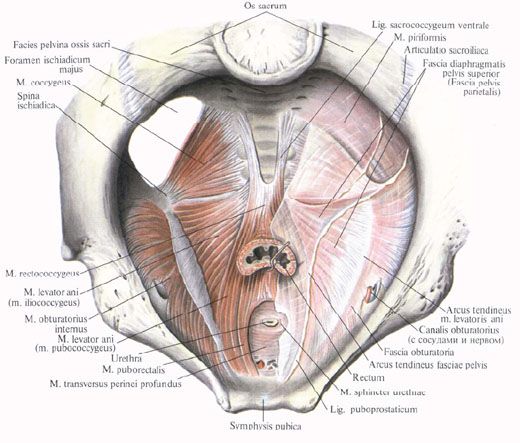
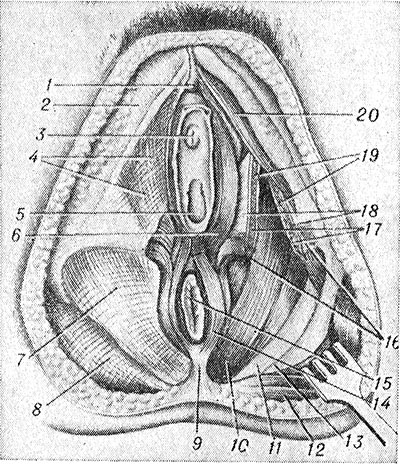
The urogenital diaphragm (genitourinary region) and the pelvic diaphragm (anal region) are muscular-fascial plates formed by two layers of muscles (superficial and deep) and fascia. In the anal area, the muscles of the pelvic diaphragm lie between its upper and lower fascia. The muscles of the urogenital diaphragm are located in such a way that the deep layer is enclosed between the upper and lower fascia of the urogenital diaphragm. All this muscular-fascial plate from the side of the pelvic cavity is covered with pelvic fascia, outside (from below) - with superficial fascia.
The urogenital diaphragm occupies the anterior part of the perineum and has the shape of a triangle, the apex of which faces the pubic symphysis. The sides are limited by the lower branches of the pubic and ischial bones, the base corresponds to the line connecting the ischial tuberosities. The urethra passes through the urogenital diaphragm in men, and the urethra and vagina in women.
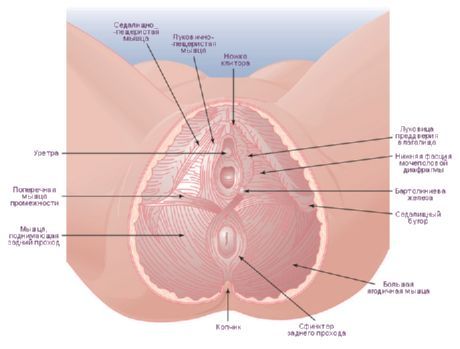
The muscles of the urogenital diaphragm are divided into superficial and deep. Superficial muscles include 3 muscles: superficial transverse perineal, ischiocavernosus, and bulbospongiosus
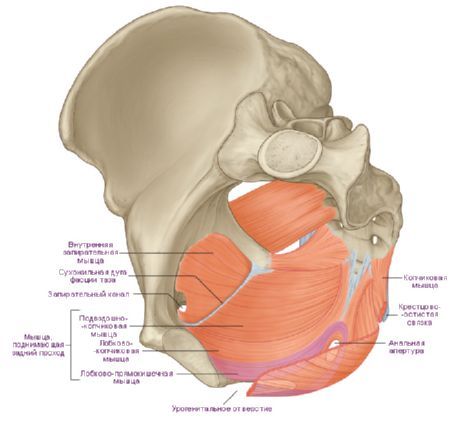
The superficial transverse muscle of the perineum (m. transversus perinei superficialis) is steam room, lies in the deep layer of subcutaneous fatty tissue. Starts on the lower branch ischium near the ischial tuberosity, goes transversely towards the same muscle of the other side and ends in the tendon center of the perineum, formed by thin flat tendons of these muscles. Part of the fibers of this muscle is woven into external sphincter anus and into the bulbous-spongy muscle of the opposite side. Superficial transverse muscles are involved in strengthening the tendon center of the perineum.
The sciatic-cavernous muscle (m.ischiocavernosus) is also paired, begins on the lower branch of the ischium. Adjacent with its medial side to the stalk of the penis (in men) or the clitoris (in women). The muscle is attached to the cavernous body, part of this muscle continues with a tendon ending to the back of the penis, where it connects to the fibers of the same muscle of the opposite side. In women, this muscle is smaller than in men. The sciatic-cavernous muscles during contraction contribute to the erection of the penis or clitoris, squeezing the venous vessels.
The bulbous-spongy muscle (m.bulbospongiosus) in men originates at the seam and the lower surface of the bulb of the penis. The fibers go forward, laterally and upward, cover the bulb and spongy body of the penis on the right and left and attach to its albuginea and superficial fascia on the back of the penis. When the muscle contracts, it compresses the bulb, the cavernous bodies and the dorsal vein of the penis, as well as the bulbourethral glands, participates in erection, and also contributes to the ejection of sperm and urine from the urethra. In women, the bulbous spongy muscle is steam room, covers the vagina in the area of \u200b\u200bits opening (m.sphincter urethrovaginalis). The muscle begins at the tendinous center of the perineum and the external sphincter of the anus, attaches to the dorsal surface of the clitoris, weaving into its albuginea. On its way, the muscle is attached from below to the glands of the vestibule. When contracting, it narrows the entrance to the vagina, compresses the large gland of the vestibule, the bulb of the vestibule and the veins emerging from it.
The deep muscles of the urogenital diaphragm include the transverse muscle of the perineum and the muscle - the sphincter of the urethra.
The deep transverse muscle of the perineum (m.transversus perinei profundus) is steam room, looks like a thin plate, begins on the branches of the ischium and pubic bones. Along the midline of the perineum, with its flat tendon, it connects with the tendon of the same muscle of the other side and participates in the formation of the tendon center of the perineum. Both muscles strengthen the urogenital diaphragm.
Muscle - the sphincter of the urethra (m. sphincter urethrae) begins partially on the lower branches pubic bones. The muscle bundles have a predominantly circular direction, covering the membranous part of the urethra in men, and the urethra in women. In men, the fiber bundles of this muscle are attached to the prostate gland, and in women, they are woven into the wall of the vagina. The muscle is an arbitrary constrictor of the urethra. In women, the muscle also compresses the vagina.
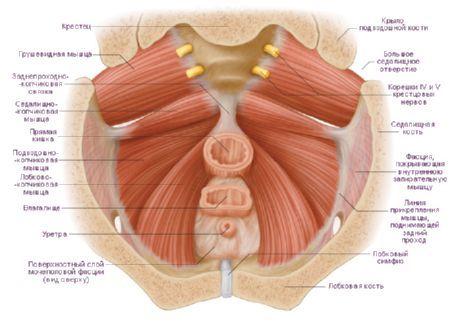
The pelvic diaphragm (diaphragma pelvis) back perineum and has the form of a triangle, the top of which is facing the coccyx, and the corners are directed to the buttocks. The final section of the rectum passes through the pelvic diaphragm in both men and women.
The surface layer of the muscles of the pelvic diaphragm is represented by an unpaired muscle - the external sphincter of the anus (m. sphincter ani externus). This muscle lies under the skin surrounding the terminal rectum. Consists of several bundles, the most superficial of which end in subcutaneous tissue. The bundles, starting at the top of the coccyx, cover the anus and end in the tendon center of the perineum. The deepest bundles, surrounding lower section rectum, adjacent to the muscle that raises the anus. All bundles of the external sphincter of the anus during their contraction compress (close) the opening of the anus.
The deep muscles of the pelvic diaphragm are two muscles that form back department bottom of the pelvic cavity. The muscle that raises the anus (m.levator ani) is steam room, has the shape of a thin triangular plate, forms a funnel with a similar muscle of the other side, the wide part facing upwards. The lower parts of both muscles, narrowing, cover the rectum in the form of a loop. The muscle originates on the side wall of the small pelvis in several bundles. The anterior bundles start at inner surface lower branch of the pubic bone, lateral - on the tendon arc of the muscle that lifts the anus (arcus tendineum musculi levatoris ani). The tendon arch is an arcuate thickening of the pelvic fascia where it forms the obturator fascia. The bundles of the right and left muscles that lift the anus go down and backwards, connect with each other, cover the rectum. Some of the fibers of these muscles are woven into the prostate gland (in men), the wall of the vagina (in women), as well as into the wall of the bladder and rectum; the muscles themselves end at the top of the coccyx in the form of an anal-coccygeal ligament (lig. anococcygeum). When the muscle that lifts the anus contracts, it strengthens and rises pelvic floor, the lower (final) section of the rectum is pulled forward and upward, which is compressed at the same time. This muscle in women also compresses the entrance to the vagina and brings back wall vagina to the anterior.
The coccygeal muscle (m.coccygeus) is paired, starts on the ischial spine and sacrospinous ligament, goes medially and posteriorly; attached to the lateral edge of the coccyx and the top of the sacrum. The bundles of this muscle are adjacent on the medial side to the sacrospinous ligament, partly woven into it, strengthening the back of the pelvic diaphragm.
The bottom of the pelvic cavity is closed by the pelvic diaphragm (diaphragma pelvis), which is complemented in front by the urogenital diaphragm (diaphragma urogenitale).
The composition of the pelvic diaphragm includes both muscles that raise the anus (m. levator ani), the coccygeal muscle and the external sphincter of the rectum (m. sphincter ani externum).
The muscle that raises the anus, steam room, has a triangular shape and consists of the pubic-coccygeal (m. pubo-coccygeus), iliococcygeal and ischiococcygeal (m. ileo-coccygeus). The entire muscle mass of the pelvic diaphragm has the shape of an inverted bowl or dome, with a concave surface facing upwards, and a convex surface downwards. In the middle of this dome there is a genital gap through which the urethra, vagina and rectum come out.
The urogenital diaphragm has a triangular shape. In its anterior section is the urogenital sphincter (sphincter uro-genitale), in the posterior - the transverse deep muscle of the perineum (m. transversus perinei profundus), associated with the muscles of the surface layer and levators.
The outer layer of the pelvic floor muscles includes the external and internal sphincters anus(m. sphincter ani externus, internus), bulbous-cavernous muscle (m. bulbo-cavernosus), superficial transverse perineal muscle (m. transversus perinei superficialis) and ischiocavernosus muscle (m. ischiocavernosus). The outer layer of the pelvic floor muscles merges with its tendons into a strong fibrous formation - the tendinous center of the perineum (centrum tendineum perinei).
The blood supply to the bottom of the pelvic cavity is carried out mainly by the branches of the internal genital vessels (a. pudenda interna). Blood supply to the perineum - external and internal genital vessels (a. pudenda externa et interna).
The innervation of the pelvic floor muscles occurs due to the branches of the sacral plexus (pli. sacralis), the external pudendal nerve (p. pudendus), and the lumbar plexus (pl. lumbalis).
The muscles of the pelvic floor are essential in maintaining intra-abdominal pressure, fixation organs abdominal cavity and pelvis.
Vessels and nerves of the perineum
The blood supply to the perineum is carried out by the branches of the internal (deep) pudendal artery, which leaves the pelvic cavity through the large sciatic foramen, goes around the ischial spine, and then enters the ischiorectal fossa through the small sciatic foramen. Here the artery gives several large branches: inferior rectal artery, perineal artery, and dorsal artery of the penis or clitoris. Deoxygenated blood flows through the veins of the same name into the internal iliac vein. Lymphatic vessels flow into the superficial inguinal lymph nodes.
The innervation of the perineum is carried out along the branches of the pudendal nerve: nerve fibers lower rectal nerves, perineal nerves, as well as anal-coccygeal nerves - branches of the coccygeal nerve.
Perineum Development
In the embryo, in the process of development, the cavity of the cloaca is divided into the ventral section - the urogenital sinus and the dorsal section - the rectum due to the frontally growing into it of the urinary rectal septum. The urinary-intestinal septum grows in the caudal direction, reaches the cloacal plate, which is then subdivided into the anterior part - the urogenital plate and the back part - the anal plate. Each plate independently breaks through, resulting in the formation of holes in the anus and the urogenital opening. Muscle fibers are formed around these openings from the mesoderm that has grown into the thickness of the anal and urogenital plates. First, sphincters are formed from these fibers, and then the muscle that lifts the anus (in the region of the anal plate), the perineum, and the rest of the muscles that make up the basis of the urogenital diaphragm.
CROTCH [perineum(PNA, JNA, BNA)] - the area between the pubic symphysis in front, the tip of the coccyx in the back, ischial tubercles and sacrotuberous ligaments from the sides. It is the lower wall of the trunk, closing the small pelvis from below, through which the urethra, rectum, and also the vagina (in women) pass. P. prevents prolapse of the pelvic organs, creates the possibility of retaining their contents (feces, urine) and controlling urination and defecation.
Embryology
Rice. 1. Schematic representation of the initial (a), middle (b) and final (c) stages of the separation of the cloaca and the formation of the perineum in embryonic period: 1- urine rectal septum; 2 - cloaca; 3 - cloacal membrane; 4 - urogenital sinus; 5 - allantois; 6 - mesonephric duct; 7 - rectum; 8 - remains of the cloacal membrane; 9 - primitive perineum. (Arrows indicate the direction of growth of the urinary-rectal septum. In Fig. b, the place of formation of the cloacal membrane is marked with a rectangle, in Fig. c, the same place is given in an enlarged form at the final stage of development of the perineum).
Separation of the intraembryonic primary intestine, the formation of a cloaca occur on the 3rd-4th week. embryonic development(Fig. 1). At the anterior and posterior ends of the primary gut, blind pockets lined with endoderm form. The posterior pocket at this stage of development expands, connects with the ducts of the allantois and the middle kidney (mesonephric duct) and turns into a cloaca (cloaca). On the outer surface of the body, according to the location of the cloaca, a recess is formed - the outer cloacal fossa (fovea externa cloacalis), edges during the 4th week. gradually deepens towards the cloaca. The bottom of the specified anal recess (proctodaeum) is separated from the cloaca by a cloacal membrane (membrana cloacalis). At the same time, from the side of the back of the coelom, paired epithelial folds containing mesenchyme and forming the urogenital septum grow into the cloaca, growing towards the proctodeum and dividing the cloaca into two sections - the anal canal (canalis analis) and the urogenital sinus (sinus urogenitalis). At the end of the separation of the cloaca by the 6-7th week. development, the cloacal membrane ruptures, forming two openings: anal (anus) and urogenital (ostium urogenitale). The lower part of the urinary rectal septum, containing the mesenchyme, subsequently forms the perineal body (corpus perineale), the upper part undergoes reduction, remaining in adults in the form of the peritoneal perineal fascia (fascia peritoneoperinealis). The degree of development of the urinary rectal septum determines the external shape of the P.: with its significant development, the P. is convex, with a weak development, it is concave. P.'s deformations meet at a concave form more often.
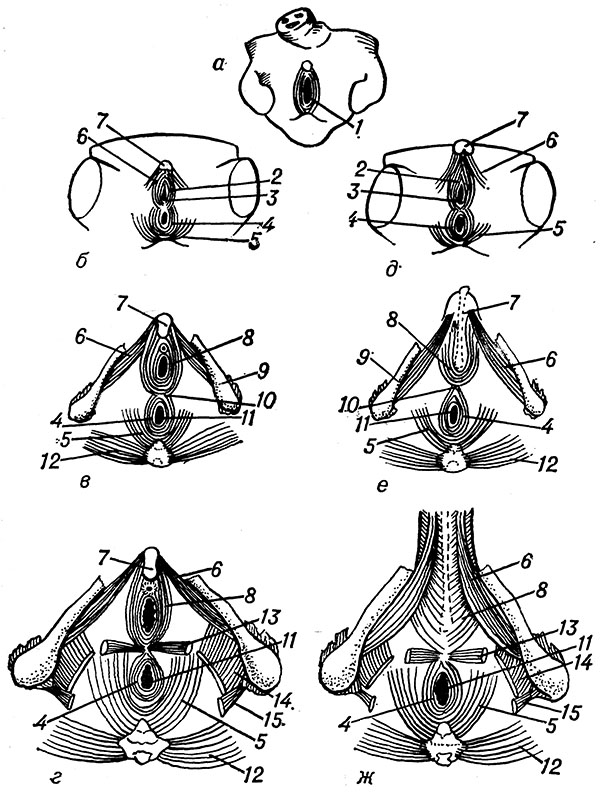
Rice. 2. Schematic representation of the stages of development of the muscles of the perineum: a - indifferent stage; b, c, d - subsequent stages of development of the muscles of the perineum of a woman; e, f, g - man's perineum; 1 - cloaca; 2 - sphincter urogenital sinus; 3 - opening of the urogenital sinus; 4-external anal sphincter; 5- muscle that raises the anus; 6 - sciatic-cavernous muscle; 7 - head of the clitoris (penis); 8 - bulbous-spongy muscle, 9 - ischium; 10 - crotch seam; 11 - anus; 12 - gluteus maximus; 13 - superficial transverse muscle of the perineum; 14 - iliac-coccygeal muscle; 15- sciatic-coccygeal muscle.
Perineal muscles that develop later than muscles abdominal wall, differentiate from various sources(Fig. 2): from the dorsal mesoderm on the 4th week. a cloacal sphincter (sphincter cloacalis) is formed, which later divides (according to the division of the cloaca) into the anlage of the sphincters of the rectum and urinary organs; the muscles of the bladder and urethra differentiate from the ventral mesoderm; from the sacral myotomes, the pelvic diaphragmatic plate (lamina diaphragmatica pelvica) is formed, giving rise to the levator ani muscle and the coccygeal muscle.
Anatomy
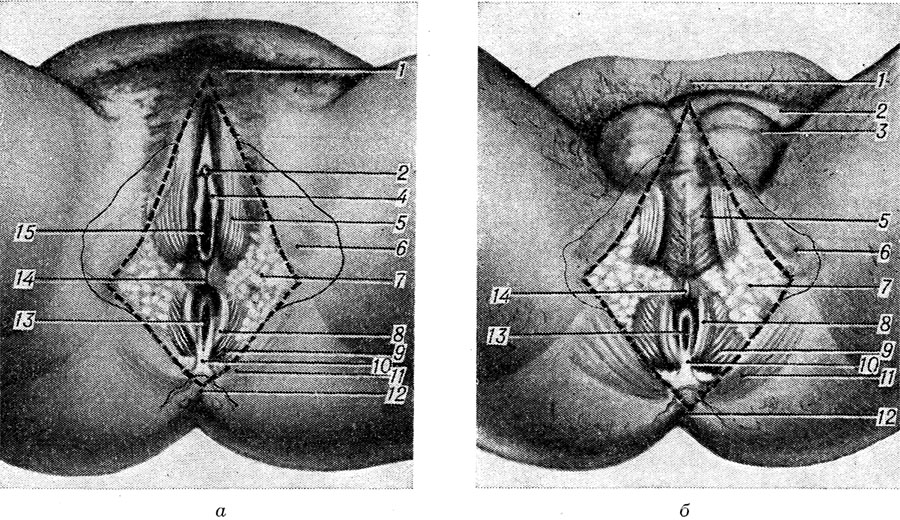
Rice. Fig. 3. Schematic representation of the female (a) and male (b) perineum (the boundaries of the perineum are indicated by a dotted line, the skin in the perineal area is separated): 1 - pubis; 2 - clitoris (Fig., a) and penis (Fig., b); 3 - scrotum; 4 - small labia; 5 - bulbous-spongy muscle; 6 - projection of the ischial tuberosity; 7- adipose tissue ischiorectal fossa; 8 - external anal sphincter; 9 - muscle that lifts the anus; 10 - anal-coccygeal ligament; 11 - gluteus maximus; 12 - projection of the coccyx; 13 - anus; 14 - crotch seam; 15 - opening of the vagina.
P. with abducted and bent legs is similar in shape to a rhombus (Fig. 3). The apexes of the corners of the rhombus are the pubic symphysis in front, the tip of the coccyx behind, and the ischial tuberosities from the sides. The sides of the rhombus form the branches of the pubic and ischial bones in front, and the sacrospinous ligaments in the back, which are covered by the lower edges of the gluteus maximus muscles. In the middle of P. in the sagittal direction there is a median tendon suture (raphe), passing in men in front into the scrotal suture.
Part P., located between the posterior commissure of the labia majora and the anus, is called the obstetric perineum, since it matters in obstetric practice. It corresponds to the tendon center P. - the place of fixation of most of the muscles of this area.
The horizontal line drawn through both ischial tubercles (linia biiachiadica), P. is divided into two areas: anal (regio analis) and genitourinary (regio urogenitalis).
Anal area
Anal area makes back department P. through which there passes a rectum (see). The skin of this department of P. is thick, grows together with the mucous membrane of the anus (see) and the muscle bundles of the external sphincter of the anus, forming radiant folds here; contains many sebaceous and sweat glands. Subcutaneous tissue and superficial fascia are well defined. In this layer skin branches of an internal genital (pubescent) artery, hypodermic limf are located. vessels, perineal nerves (branches of the pudendal nerve), perineal branches of the posterior cutaneous nerve of the thigh.
(in the figure, the skin and subcutaneous tissue are removed on the left, the fascia are removed on the right): 1 - head of the clitoris; 2 - wide fascia; 3 - external opening of the urethra; 4 - superficial fascia of the perineum; 5 - opening of the vagina; 6 - bulbous-spongy muscle; 7 - lower fascia of the pelvic diaphragm; 8 - gluteal fascia; 9 - anal-coccygeal ligament: 10 - muscle that lifts the anus; 11 - sacrospinous ligament; 12 - gluteus maximus; 13 - sacrotuberous ligament; 14 - external anal sphincter; 15 - anus; 16 - superficial transverse muscle of the perineum (crossed); 17 - deep transverse muscle of the perineum (crossed); 18 - lower fascia of the urogenital diaphragm; 19 - upper fascia of the urogenital diaphragm; 20 - ischiocavernosus muscle.
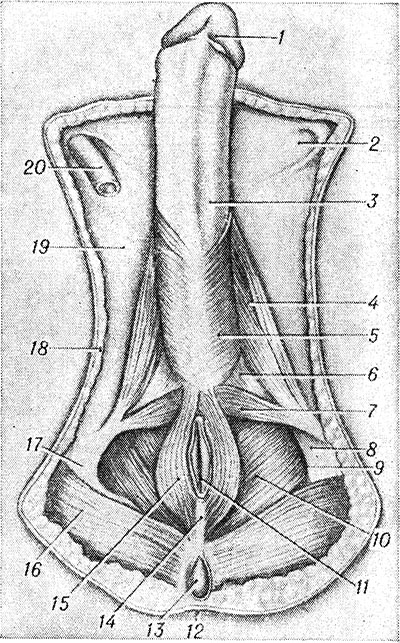
(removed the skin, subcutaneous tissue, fascia of the muscles of the perineum, testicles and scrotum): 1 - glans penis: 2 - superficial inguinal ring; 3 - fascia of the penis; 4 - ischiocavernosus muscle; 5 - bulbous-spongy muscle; 6 - deep transverse muscle of the perineum; 7 - superficial transverse muscle of the perineum; 8 - obturator fascia; 9 - rectal-sciatic fossa; 10 - muscle that lifts the anus; 11 - anus; 12 - skin; 13 - coccyx; 14 - anal-coccygeal ligament; 15 - external anal sphincter; 16 - gluteus maximus; 17 - ischial tubercle; 18 - subcutaneous tissue; 19 - wide fascia; 20 - vas deferens.
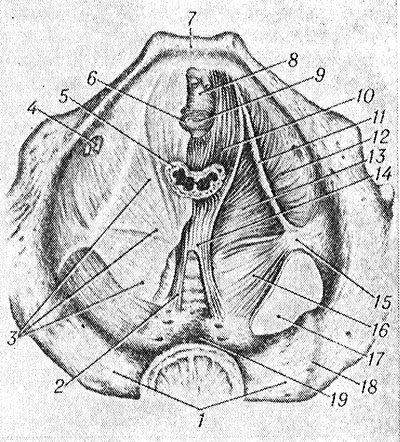
(top view; muscle fascia removed on the right): 1 - sacrum; 2 - ventral sacrococcygeal ligament; 3 - upper fascia of the pelvic diaphragm; 4 - obturator canal (with neurovascular bundle); 5 - rectum; 6 - sphincter of the urethra; 7 - pubic symphysis; 8 - deep transverse muscle of the perineum; 9 - urethra; 10 - pubic-coccygeal muscle; 11 - tendinous arch of the muscle that raises the anus; 12 - internal obturator muscle; 13 - iliac-coccygeal muscle; 14 - rectococcygeal muscle; 15 - ischial spine; 16 - coccygeal muscle; 17 - large sciatic foramen; 18 - sacroiliac joint; 19 - pelvic surface of the sacrum.
![]()
Color illustrations.: Rice. one. Muscles, arteries and nerves of the male perineum(skin, subcutaneous tissue and fascia removed): 1-meaty shell of the scrotum; 2 - posterior scrotal nerves; 3 - bulbous-spongy muscle; 4 - artery of the bulb of the penis; 5- perineal artery; 6 - dorsal artery of the penis; 7 - dorsal nerve of the penis; 8 - branches of the lower rectal artery; 9 - ischiorectal fossa; 10 - gluteus maximus muscle (cut off on the left); 11 - lower gluteal nerves; 12-external anal sphincter; 13 - anal-coccygeal nerves; 14 - coccyx; 15 - lower rectal nerves; 16 - sacrotuberous ligament (crossed); 17-genital nerve; 18 - sacrospinous ligament; 19 - internal genital artery; 20 - perineal nerve; 21 - ischial tubercle; 22 - superficial transverse muscle of the perineum; 23 - perineal branches of the posterior cutaneous nerve of the thigh; 24 - ischiocavernosus muscle; 25 - posterior scrotal arteries. Rice. 2. Muscles, arteries and nerves of the female perineum(skin, subcutaneous tissue and fascia removed): 1 - head of the clitoris; 2 - opening of the vagina; 3 - posterior labial nerves (large labia); 4 and 22 - bulbous-spongy muscle; 5 - dorsal nerve of the clitoris; 6 - dorsal artery of the clitoris; 7-perineal nerve; 8 - internal genital artery; 9 - ischiorectal fossa; 10 - gluteus maximus; 11 - lower rectal nerves; 12 - anal - coccygeal nerves; 13 - coccyx; 14 - lower gluteal nerve; 15 - anus; 16 - external anal sphincter; 17 - muscle that lifts the anus; 18 - perineal branches of the posterior cutaneous nerve of the thigh; 19 - superficial transverse muscle of the perineum; 20 - posterior labial arteries (large labia); 21 - sciatic-cavernous muscle; 23 - external opening of the urethra.
Deeper lies P.'s own fascia (fascia perinei propria), upon dissection, the sciatic-rectal fossa (fossa ischiorectalis) opens, filled with loose connective and adipose tissue - the fatty body (corpus adiposum). The outer wall of the fossa is the internal obturator muscle and its fascia, the inner wall is the lower surface of the muscle that lifts the anus, the lower fascia of the pelvic diaphragm and the external sphincter of the anus covering it (Fig. 4, 5, 6). The superficial transverse muscle of P. is considered the anterior border of the fossa, although the fossa protrudes in the form of a narrow pocket into the genitourinary region. In the fiber of the fossa are the lower rectal vessels and nerves of the same name; on the lateral wall in the splitting of the fascia (pudendal canal, sapa-lis pudendalis, Alcock's canal) pass the internal genital vessels and the genital nerve (tsvetn. Fig. 1, 2).
The following muscles are located in the anal region of P.. The external sphincter of the anus (m. sphincter ani ext.) starts from the top and lateral sections of the coccyx, anal-coccygeal ligament (lig. anococcygeum) and adjacent skin areas. The sphincter bundles bypass the anus on the right and left and join in front of it; they are supported by muscle bundles of the longitudinal layer of the rectum, bundles of the muscle that lifts the anus, and the anal-coccygeal muscle (m. anococcygeus). The depth of coverage of the anal canal by the sphincter is 3-5 cm, the thickness of the sphincter is up to 8 mm. The sphincter is divided into three parts: subcutaneous (pars subcutanea), superficial (pars superficialis) and deep (pars profunda). The muscle that lifts the anus (m. Levator ani), steam room, together with the coccygeal muscle makes up the pelvic diaphragm (diaphragma pelvis). Depending on the place of the beginning of its individual portions, it is divided into two muscles: pubic-coccygeal (m. pubococcygeus) and iliococcygeal (m. iliococcygeus). The pubococcygeal muscle starts from the posterior surface of the pubic bones and from the anterior part of the tendinous arch of the muscle that lifts the anus (arcus tendineus m. Levatoris ani), formed by the obturator fascia. The muscle bundles spread backwards, cover the rectum, and they are intertwined with the bundles of the same muscle of the other side and with the longitudinal muscle bundles of the intestine and are attached to the anal-coccygeal ligament, coccyx and ventral sacrococcygeal ligament. In men, the anterior edges of the pubococcygeal muscle are closely fused with the prostate capsule; this part of the muscle bundles stands out as a muscle that lifts the prostate gland (m. levator prostatae). In women, such bundles adjoin the wall of the vagina and are designated as the pubic-vaginal muscle (m. pubovaginalis). The iliococcygeal muscle originates from the tendinous arch of the levator ani muscle and the ischial spine. The muscle bundles run downward, posteriorly and medially and are attached to the coccyx and ventral sacrococcygeal ligament. The bundles of this muscle are intertwined at the rectum with the bundles of the pubococcygeus muscle and form a loop-like coverage around the intestine. The coccygeal muscle (m. coccygeus) originates from the ischial spine and is attached to the lateral surface of the lower sacral vertebrae and coccyx. The pubic-rectal muscle (m. puborectalis) is also distinguished, which starts from the pubic bones, goes to the rectum, lying more superficially than the pubococcygeal muscle, and connects to the external sphincter of the anus. These muscles are covered by the inferior fascia of the pelvic diaphragm.
blood supply the anal region is carried out through the internal genital artery (a. pudenda int.) and the arteries that are its branches: the lower rectal (a. rectalis inf.), going to the anal canal and anus, and the perineal (a. perinealis) - to the muscles of P. ; venous outflow occurs through the veins of the same name.
Innervated the anal region with the pudendal nerve (n. pudendus) and its branches: the lower rectal nerves (nn. rectales inferiores), innervating the external sphincter of the anus, the perineal nerve (n. perinealis), giving muscle branches, and the anal-coccygeal nerves (nn. anococcygei), which are branches of the coccygeal nerve.
lymph drainage passes through the paravaginal (nodi lymphatici paravaginales), pararectal (nodi lymphatici pararectales), lower gluteal (nodi lymphatici gluteales inf.), sacral (nodi lymphatici sacrales) and inguinal (nodi lymphatici inguinales) limf. nodes.
Genitourinary area
In the urogenital region in men is the scrotum (see) and the root of the penis (see), in women - the external genitalia (see Vulva). The skin is hairy and richly supplied with sebaceous and sweat glands. Subcutaneous tissue and superficial fascia are expressed. Own fascia is part of P.'s own fascia.
Deep-lying formations form two spaces of the genitourinary region: superficial and deep. In the surface space (spatium perinei superficiale) there are 3 muscles: the superficial transverse muscle of the P., ischiocavernosus, and bulbous-spongy. The superficial transverse muscle P. (m. transversus perinei superficialis) is steam room, narrow, goes from the ischial tubercle to the tendon center P. The sciatic-cavernous muscle (t. ischiocavernosus) is steam room, originates from the ischial tuber and is attached to the albuginea of the cavernous body; under the muscles lie the legs of the root of the penis in men and the legs of the clitoris in women. The bulbous-spongy muscle (m. bulbospongiosus) steam room, starts from the tendon center P., in men it covers the inferolateral surface of the bulb of the penis and fuses in the middle with the same muscle of the other side; in women, it surrounds the opening of the vagina.
AT deep space(spatium perinei profundum) the urogenital diaphragm (diaphragma urogenitale), otherwise called the urogenital triangle (trigonum urogenitale), is located, formed by the deep transverse muscle of P. and the fascia covering it from above and below - the upper and lower fascia of the urogenital diaphragm (fasciae diaphragmatis urogenitalis sup. et inf .). The deep transverse muscle of P. (t. transversus perinei profundus) starts from the ischial tubercles and branches of the ischial and pubic bones. Its bundles go transversely in the medial direction to the midline, where they form a tendon median suture P with the muscle of the opposite side. The urethra passes through the muscle in men (see), in women - the urethra and vagina (see). The part of the muscle surrounding the urethra is called the sphincter of the urethra (m. sphincter urethrae). The front edge of the deep transverse muscle does not reach the symphysis, and this gap is filled with fused upper and lower fascia of the urogenital diaphragm, which form here the transverse ligament P. - lig. transversum perinei (old name: transverse pubic ligament - lig. transversum pubis). The part of this fusion adjacent to the symphysis is called the arcuate pubic ligament (lig. arcuatum pubis). In men, between the urethra and the anal part of the rectum, below the rectovesical septum, the perineal body (corpus perineale) is located under the skin. In women, this body is located between the anterior wall of the anus and the posterior wall of the vagina below the rectovaginal septum. The perineal body is tightly attached behind to the front of the external sphincter of the anus, and in front - to the prostate gland and the membranous part of the urethra (in men) and to the vagina (in women). The perineal body is a fibromuscular mass 1.5-2 cm wide (its dimensions are 1-1.5 cm in the anteroposterior and 2-2.5 cm in the vertical directions).
blood supply formations of the genitourinary region carry out branches of the internal pudendal artery: in men - scrotal arteries (rr. scrotales posteriores), urethral artery (a. urethralis), artery of the bulb of the penis (a. bulbi penis), arteries of the penis (aa. profunda et dorsalis penis ); in women, the posterior labial arteries (rr. labiales posteriores), the urethral artery (a. urethralis), the vestibule artery (a. vestibuli vaginae), the clitoral artery (aa. profunda et dorsalis clitoridis). Venous outflow blood is coming through the veins of the same name, carrying blood into the internal iliac vein (v. iliaca int.).
Innervate this area of the branch of the perineal nerves: posterior scrotal (labial) - nn. scrotales (labiales) posteriores, dorsal nerve of the penis (clitoris) - n. dorsalis penis (clitoridis).
lymph drainage passes through the same limf, nodes, as from the anal region of P.
Pathology
Developmental defects. congenital clefts Items arise in late stages development of the embryo as a result of nonunion of the genital folds. In boys, the cleft is located along the median suture of P. and is a narrow rectilinear tissue defect, the walls of which are covered with a mucous membrane that produces mucus. In girls, the cleft merges with the genital cleft and is covered with a mucous membrane coming from the vestibule of the vagina; the posterior commissure of the labia is absent.
Wedge. manifestations of P.'s cleft in boys are irritation of the skin of the perineum and the presence of itching. The girls have no complaints.
In boys, the cleft does not heal on its own, therefore it is shown surgical treatment, a cut consists in excision of the mucous membrane covering the cleft, together with the skin edges and suturing the wound tightly. In girls, clefts usually heal on their own.
P.'s teratoid educations are a consequence of disturbance of embryonic development. They occur both in children (more often in girls) and in adults (more often in men). In children, teratoid formations are characterized by rapid growth and a significant risk of malignancy, which, according to various sources, is observed in 10-25% of patients and is associated with low differentiation of formation cells. Teratomas are more common (see), much less often - dermoid cysts (see Dermoid) and epidermoid cysts (see). In adults, epidermoid and dermoid cysts predominate, teratomas are rare. Malignancy is observed in approximately 2% of patients.
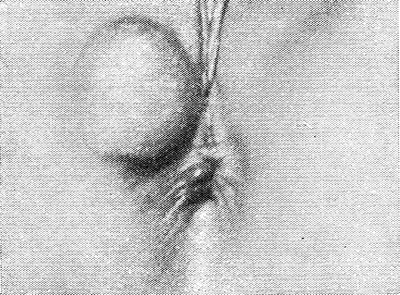
Rice. 7. View of the perineum with a dermoid cyst in a woman.
Teratoma is usually located under the skin of the perineum between the tip of the coccyx and the anus, often hanging between the legs of the child. because of rapid growth it can shift the anus anteriorly or to the side. In this case, the rectum and urethra are often compressed, which leads to a delay in stool and urination. Dermoid and epidermoid cysts look like tumor-like formations located in the subcutaneous tissue of the perineum (Fig. 7). Cysts have a tight elastic consistency, sometimes fluctuation can be felt. Quite often, teratoid formations suppurate and spontaneously open, followed by the formation of long-term non-healing single or multiple fistulas.
Epidermoid and dermoid cysts are diagnosed on a wedge. signs. One of characteristic features teratoma is the alternation in it of dense areas of tissue with cystic formations. Plain radiography reveals bone structures and calcified inclusions. In some cases, teratoid formations differentiate with spinal hernia(see Spina bifida), and in the presence of fistulas - with fistulas of the rectum (see). In these cases, the most effective fistulography (see) and puncture cystography (see): in the presence of teratoid formations on radiographs are determined cystic formations round shape with smooth clear inner contours. In doubtful cases the biopsy is necessary (see).
Treatment of teratoid formations is operative. In children, due to the frequent malignancy of teratomas, the operation is carried out without delay. A transverse arcuate skin incision is made on the perineum, the ends of which reach the ischial tubercles, and the middle is 5 cm posterior to anus. The tumor-like formation in front is separated from the wall of the rectum. To remove part of it, located in the pelvis, the coccyx is sometimes resected. The teratoma is removed as a single block without opening the cystic cavities. After excision of the resulting excess skin, the wound is sutured tightly, leaving rubber drains.
Dermoid and epidermoid cysts in adults are removed as a single block, using a fringing skin incision and avoiding opening the lumen of the cyst. In the presence of draining fistulas, the latter are excised within healthy tissues. The wound is sutured leaving rubber drains. In the presence of purulent fistulas, the wound is not sutured tightly, but only narrowed with sutures.
Forecast at prompt removal benign teratoid formations favorable. With malignant and primary malignant tumors, the prognosis is unfavorable.
Damage perineum can be closed (bruises, subcutaneous ruptures, hematomas, etc.) and open (cut and stab wounds, gunshot wounds and etc.). In those and other cases, P.'s damage can be combined with damage to the extraperitoneal rectum, bladder, urethra, and pelvic bones, which determines the wedge. picture. Damage to P. in women associated with childbirth has a certain specificity (see below).
All P.'s injuries are characterized by sharp pains, sometimes accompanied fainting, increased body temperature. In connection with the hemorrhage (see) or the formation of a hematoma (see), there is a feeling of fullness in P., the edge swells, its skin acquires a cyanotic color. Closed injuries Items with damage to the rectum, bladder, or urethra are usually observed in the presence of fractures of the pelvic bones. In these cases, urine and feces can enter the surrounding tissues. With combined wounds of P. and the rectum, urgent (sometimes false) urges to defecate appear immediately after the injury. Feces and gases are released from the wound openings on P., an admixture of blood is found in the feces; the function of the external sphincter of the anus is often disturbed. The combined wounds of P. and the bladder or urethra are accompanied by the release of urine from P.'s wound, urinary infiltration of P.'s fiber with the formation of urinary streaks (see Urinary stagnation).
Soft tissue wounds near the anus are exposed to contamination during defecation and become infected. And if superficial wounds often heal without significant complications, then with deep and extensive wounds often develop phlegmon, spreading to the pelvic tissue. At the same time accession of an anaerobic infection is possible (see).
Diagnosis of P.'s damages is based on characteristic a wedge. symptoms and wound probing data, finger research rectum, anoscopy, rectoscopy and rentgenol. research.
Treatment of P.'s damages depends on their character. With P.'s bruises without damage to the rectum or bladder (urethra), apply conservative treatment- rest, in the first days cold on P., then thermal procedures (see Bruising). Hematomas that do not tend to increase are also treated conservatively; at distribution of a hematoma make operation for the purpose of a hemostasis (see. Hematoma ). Superficial wounds Items, given their increased infectivity, are widely dissected, excised non-viable tissues and well drained (see Drainage).
When P. is injured with damage to the rectum, the wound is cut into P., necrotic and fecal-contaminated tissues are excised, the wound is treated with antiseptics and antibiotics, and it is drained with swabs with ointment. A wound in the intestinal wall, depending on the size of the defect and the duration of the injury, is sutured or drained after a colostomy is applied (see Colostomy). Damaged fibers of the external anal sphincter are sutured.
When P.'s injury is combined with an injury to the bladder (urethra), a high suprapubic fistula is applied (see Cystotomy), urinary streaks are drained (see Bladder).
With combined wounds of the perineum, rectum and bladder (urethra), complicated by pelvic phlegmon, P.'s wound is widely dissected and drained, purulent streaks are opened, an unnatural anus (see Anus praeternaturalis) and a high fistula of the bladder are applied.
Diseases. Purulent processes in P. may occur with microtraumas and wounds of P., damage and inflammatory processes in the rectum, injury to the urethra, purulent inflammation prostate and seminal vesicles, osteomyelitis of the sacrum and coccyx, suppuration of teratoid formations; also transfer of an infection from the remote centers on limf is possible. and venous routes.
Furuncles, hypodermic abscesses and phlegmons of P. Klin are more often observed. the picture of P.'s furuncle differs little from furuncles of other localizations (see Furuncle ).
Syphilis P. manifests itself in the form of primary syphilomas the size of lentils, which have the correct shape, dense texture, reddish color. Then there is erosion or an ulcer. Secondary syphilis in the form of papular syphilis is often localized on the perineum. Sometimes papules increase in size, their base is covered with growths, expands (wide condylomas). Syphilitic gummas (tertiary syphilis) of the perineum are from 1 to 3 cm in diameter, located in the subcutaneous tissue. They spontaneously open and form ulcers with undermined edges and scanty discharge. Specific treatment - see Syphilis].
Perineal hernias are rare. Seen in people who engage in heavy physical labor, especially those with a weak pelvic diaphragm or traumatized P. There are anterior and posterior perineal hernias (see). Clinically, they manifest as a tumor-like formation that occurs when physical activity, walking, coughing. Easily adjusted. On palpation, a defect in the P. muscles is detected. Treatment is surgical closure of the hernial orifice in the pelvic diaphragm, for which perineal access is often used.
P.'s mesenchymoma (Fig. 8) is less common than lipoma; is a tumor of a complex structure from mesenchymal derivatives. The tumor is of soft consistency, moderately mobile and slightly painful, covered with a capsule; on the cut, its fabric is distinguished by great variegation.
Along with knotty-stranded tissue, there may be cystic cavities with a diameter of 5-20 cm, filled with viscous or liquid contents. Microscopically, the tumor is a multicomponent formation consisting of fatty, vascular and fibrous tissue in various combinations.
Often perineal mesenchymoma is associated with the wall of the rectum. Tumors built from mature components of the mesenchyme proceed benignly.
For diagnosis use a puncture biopsy and rentgenol. research methods (survey radiography, proctography, parietography). In some cases, it becomes necessary to differentiate mesenchymoma from perineal hernia and teratoid formations.
Treatment is operative. Operational access - perineal. The postoperative wound is sutured leaving rubber drains.
Injuries to the perineum in women associated with childbirth have a certain specificity. Most often breaks and hematomas of P meet.
Perineal lacerations are more common with pathological childbirth(extension inserts, breech presentation) and during operative delivery (forceps, extraction of the fetus by the pelvic end, vacuum extraction).
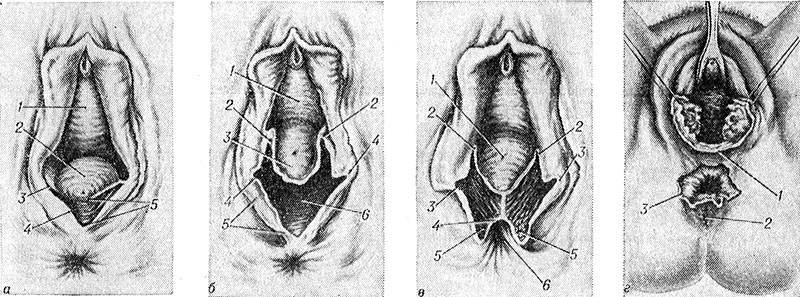
A - rupture of the 1st degree (1 - anterior wall of the vagina, 2 - posterior wall of the vagina, 3 - posterior commissure of the labia majora, 4 - skin of the perineum, 5 - rupture of the perineum; b - rupture of the II degree (1 - anterior wall of the vagina, 2 - the upper edge of the gap, 3 - the posterior wall of the vagina, 4 - the posterior commissure of the labia majora, 5 - the skin of the perineum, 6 - the gap of the perineum); III degree(1 - the posterior wall of the vagina, 2 - the upper edge of the gap, 3 - the posterior commissure of the labia majora, 4 - the mucous membrane of the rectum, 5 - the external sphincter of the anus, 6 - the anus); d - central gap (1 - posterior commissure of the labia majora, 2 - anus, 3 - central gap of the perineum).
There are three degrees of P.'s ruptures: at a rupture of the I degree, the posterior commissure of the labia majora and P.'s skin are damaged without muscle damage (Fig. 9, a); with a rupture of the II degree, in addition to the posterior commissure and the skin of the perineum, the tendon center of the P. and the bulbous-cavernous muscle going to it, the superficial transverse muscle of the P., and the muscle that lifts the anus are torn (Fig. 9, b); with a rupture of the III degree, a violation of the integrity of the external sphincter of the anus is added (Fig. 9, c) with damage ( complete break III degree) or without damage (incomplete rupture III degree) of the rectal wall. Extremely rare so-called. the central gap of P., at Krom the back commissure of large labia and the upper part of P. remain intact, the gap occurs in the area of the tendon center of P. (Fig. 9, d); the fetus in this case can be born through the hole between the posterior commissure of the labia majora and the external sphincter of the rectum, bypassing the opening of the vagina.
Diagnosis of ruptures and the degree of P.'s damage is performed when examining the vulva after the completion of the afterbirth period (see).
Treatment of ruptures is operative. P.'s rupture of any degree must be sutured, which protects the puerperal from penetrating the infection into the wound and prevents the future development of pelvic floor muscle insufficiency with the prolapse of the walls of the vagina and uterus and relaxation of the vagina; unsutured rupture III degree, accompanied by non-retention of gases and stool leading to disability. To eliminate these phenomena, they subsequently resort to different options perineoplasty in order to restore the muscular-fascial structure of the P. and the pelvic floor (see Prolapse of the uterus, vagina; Colpoperineoplasty).
Sewing up of the first degree tear can be performed under local infiltration anesthesia with 0.25% solution of novocaine. Rupture II degree is recommended to be sutured under conduction anesthesia(see Local anesthesia), for which purpose 50-80 ml of 0.25% solution of novocaine is injected into each ischiorectal fossa; infiltration anesthesia with II degree rupture can make it difficult to orientate in tissues and compare them with each other. Rupture III degree is sutured under anesthesia (see). At puerperas with toxicosis of pregnancy in order to avoid provocation of an attack of an eclampsia (see) it is recommended to take in all P.'s ruptures under anesthesia.
With a rupture of the perineum of the 1st degree, 2-3 silk sutures are applied to the edges of the wound, which are carried out under the bottom of the wound. At a rupture of the II degree, catgut sutures are first applied to the torn muscle that lifts the anus, the fascia and the superficial transverse muscle of the P., and only after that silk sutures are applied to the skin and posterior commissure large labia. In case of a rupture of the perineum of the III degree, the rupture of the rectum is first sutured, sutures (catgut or thin lavsan) are carried out through the muscles of the intestine without piercing the mucous membrane, the external sphincter of the anus is sutured with two catgut sutures, and then they act as with a rupture P. II degree. With central tears, the preserved posterior commissure of the labia majora is dissected, and then the gap is sutured in the same way as a grade II tear.
After stitching the gaps I and II degree on the 4th day, a laxative is given, on the 5th day the sutures are removed. With a rupture of the III degree, a laxative is prescribed on the 5th day, the sutures are removed on the 6th day.
Postoperative complications - suppuration, divergence of sutures - are rare, in the vast majority of puerperas the wounds heal primary tension. In case of divergence of the seams with ruptures of I and II degrees, within 2-3 days, agents are used that cleanse the wound from necrotic and purulent raids, and then secondary (silk) sutures are applied through all layers of the wound, which are removed on the 7-8th day. With a grade III rupture, re-intervention is possible after 3-4 months. after childbirth, when they disappear inflammatory phenomena in the area of damage.
P.'s prevention of ruptures consists in proper management childbirth (see), careful operational delivery and also timely dissection of P. at the threat of its rupture. The latter occurs when P. is overstretched, which is characterized first by cyanosis of the skin (difficulty venous outflow), then its blanching (decrease in arterial inflow), and finally, the appearance of small cracks in the epidermis on the glossy surface of the skin. At this point, at high II. it is recommended to produce a median perineotomy, with a low one - a lateral perineotomy or episiotomy (see Perineotomy).
P.'s hematomas are formed at outwardly intact P., meet seldom, are more often combined with hematomas of a vagina and a vulva. At the same time, after some time after childbirth, the puerperal complains of a feeling of fullness in the perineum and pressure on the rectum. On examination, P.'s bulging, blueing of the skin are found. The boundaries of the hematoma are established using mirrors, as well as with vaginal and rectal examination. If the hematoma does not increase, then they are limited to conservative treatment; in the first days - cold on the perineum, in the subsequent - heat, ultrasound, etc. Antibiotics are used to prevent infection for 5-7 days. With the growth of a hematoma, it is necessary to open it and bandage the bleeding vessel; in case of impossibility to detect a vessel in tissues imbibed with blood, they are stitched with thin catgut and the wound is plugged. An infected hematoma is opened, plugged and treated according to the rules of purulent surgery.
See also Childbirth, birth trauma.
Bibliography
Almazov I. V. and Sutul ov JI. S. Atlas on histology and embryology, M., 1978; Aminev A. M. Guide to proctology, t. 3, p. 441, Kuibyshev, 1973; Human Anatomy, ed. S. S. Mikhailova, p. 341, M., 1973; Kirpatovsky I. D. and Bocharov V. Ya. Relief human anatomy, p. 73, M., 1974; Lenyushkin A. I. Proctology childhood, With. 254, M., 1976; Malinovsky M. S. Operative obstetrics, M., 1974; Multi-volume guide to obstetrics and gynecology, ed. J.I. S. Persianinova, vol. 3, book. 2, p. 164, Moscow, 1964; Practical obstetrics, ed. Ya. P. Solsky, p. 451, Kyiv, 1977; R ud and A. S.'s N and M and rosh N and - to about in V. M. Embryogenesis of muscles of a crotch of the person, Arkh. anat., gistol, and embryol., t. 65, c. 8, p. 82, 1973; At g-l about in F. G. and M ur with and l about in and R. A. Teratoma ( mixed tumors) presacral region, JI., 1959, bibliogr.; Falin JI. I. Human embryology, Atlas, M., 1976; Kamina P., Tour-ris H. e. Rideau Y. Anatomie fonctionnelle du périnée obstétrical, le bassin mou, Rev. franc. Gynec., t. 67, p. 17, 1972; About h C. a. K a r k A. E. Anatomy of the perineal body, Dis. Colon Rect., v. 16, p. 444, 1973; Pennington T. R. A treatise on the diseases and injuries of the rectum, anus and pelviccolon, Philadelphia, 1923; W i s o n P. M, Understanding the pelvic floor, S. Afr. med. J., v. 47, p. 1150, 1973.
V. D. Fedorov; S. H. Davydov (gin.), S. S. Mikhailov (an.).
The perineum is the diamond-shaped area between the thighs and buttocks where the urethra, vagina, and anus are located. In front, the perineum is limited by the pubic symphysis, behind - by the end of the coccyx, laterally ischial tubercles. The skin limits the perineum from the outside and below, and the pelvic diaphragm (pelvic fascia), formed by the lower and upper fascia, limits the perineum from deep above.
The pelvic floor, using an imaginary line connecting the two ischial tuberosities, is divided anatomically into two triangular regions: in front - the genitourinary region, behind - the anal region. In the center of the perineum between the anus and the entrance to the vagina there is a fibromuscular formation called the tendon center of the perineum. This tendon center is the site of attachment of several muscle groups and fascial layers.
In the genitourinary region, between the lower branches of the ischial and pubic bones, there is a muscular-fascial formation called the "urogenital diaphragm" (diaphragma urogenitale). The vagina and urethra pass through this diaphragm. The diaphragm serves as the basis for fixing the external genital organs. From below, the urogenital diaphragm is limited by the surface of whitish collagen fibers that form the lower fascia of the urogenital diaphragm, which divides the urogenital region into two dense anatomical layers, which have an important clinical significance, - superficial and deep sections, or pockets of the perineum.
Superficial perineum
The superficial section of the perineum is located above the lower fascia of the urogenital diaphragm and contains on each side a large gland of the vestibule of the vagina, a clitoris leg with the ischiocavernosus muscle lying on top, a bulb of the vestibule with the onion-spongy (bulb-cavernous) muscle lying on top and a small superficial transverse muscle of the perineum.
The ischiocavernosus muscle covers the stalk of the clitoris and plays a significant role in maintaining its erection, as it presses the stalk against the ischio-pubic branch, delaying the outflow of blood from the erectile tissue. The bulbospongiosus muscle originates from the tendinous center of the perineum and the external sphincter of the anus, then passes behind around the lower part of the vagina, covering the bulb of the vestibule, and enters the perineal body. The muscle can act as a sphincter to compress the lower part of the vagina. The weakly developed superficial transverse muscle of the perineum, which looks like a thin plate, starts from the inner surface of the ischium near the ischial tuberosity and goes transversely, entering the perineal body. All muscles superficial department covered with deep perineal fascia.
Deep perineum
The deep section of the perineum is located between the lower fascia of the urogenital diaphragm and the indistinct upper fascia of the urogenital diaphragm. The urogenital diaphragm consists of two layers of muscles. The muscle fibers in the urogenital diaphragm are mostly transverse, arising from the ischio-pubic branches of each side and joining in the midline. This part of the urogenital diaphragm is called the deep transverse perineal muscle (m. transversus perinei profundus). Part of the fibers of the sphincter of the urethra rises in an arc above the urethra, while the other part is located around it circularly, forming the external sphincter of the urethra. The muscle fibers of the urethral sphincter also pass around the vagina, concentrating where the external opening of the urethra is located. The muscle plays an important role in restraining the process of urination when the bladder is full and is an arbitrary constrictor of the urethra.
The deep transverse perineal muscle enters the perineal body behind the vagina. When contracted bilaterally, this muscle thus supports the perineum and the visceral structures passing through it.
Along the anterior edge of the urogenital diaphragm, its two fasciae merge to form the transverse ligament of the perineum. In front of this fascial thickening is the arcuate pubic ligament, which runs along the lower edge of the pubic symphysis.
Anal area
The anal (anal) region includes the anus, the external anal sphincter, and the ischiorectal fossa. The anus is located on the surface of the perineum. The skin of the anus is pigmented and contains sebaceous and sweat glands. The sphincter of the anus consists of superficial and deep parts of striated muscle fibers. The subcutaneous part is the most superficial and surrounds the lower wall of the rectum, the deep part consists of circular fibers that merge with the muscle that lifts the anus (m.levator ani). The superficial part of the sphincter consists of muscle fibers that run mainly along the anal canal and intersect at right angles in front of and behind the anus, which then fall in front of the perineum, and behind - in a mild fibrous mass called the anal-coccygeal body, or anal-coccygeal. coccygeal ligament. The anus externally is a longitudinal slit-like opening, which is probably due to the anteroposterior direction of many muscle fibers of the external sphincter of the anus.
The ischiorectal fossa is a wedge-shaped space filled with fat, which is externally bounded by the skin. The skin forms the base of the wedge. The vertical side wall of the fossa is formed by the obturator internus muscle. The inclined supramedial wall contains the levator ani muscle. Ischiorectal adipose tissue allows the rectum and anal canal expand during bowel movements. The fossa and the fatty tissue contained in it are located anteriorly and deeply upward to the urogenital diaphragm, but below the levator ani muscle. This area is called the front pocket. Behind the fatty tissue in the fossa runs deep to the gluteus maximus muscle in the area of the sacrotuberous ligament. Laterally, the fossa is bounded by the ischium and the obturator fascia, which covers lower part obturator internus muscle.
Ed. G. Savelyeva
"What is and how is the perineum arranged" - an article from the section
Crotch(perineum) - the area between the pubic symphysis in front, the tip of the coccyx behind, ischial tubercles and sacrotuberous ligaments from the sides. It is the lower wall of the body, closing the small pelvis from below, through which the urethra, rectum, and also the vagina (in women) pass.
The perineum has the shape of a rhombus and is divided by a conditional line connecting the ischial tubercles into two unequal triangular regions: the anterior - the urogenital region, where the urogenital diaphragm is located, and the posterior - the anal region formed by the pelvic diaphragm.
The muscles of the urogenital diaphragm are divided into superficial and deep. Superficial muscles include the superficial transverse perineal muscle, ischiocavernosus muscle, bulbospongiosus muscle ( rice. one ). The superficial transverse perineal muscle strengthens the tendinous center of the perineum. The sciatica-cavernous muscle in men surrounds the peduncle of the penis, part of the fibers goes to the rear of the penis and passes into the albuginea by tendon stretching. In women, this muscle is poorly developed, goes to the clitoris, participates in its erection. The bulbospongiosus muscle in men begins on the lateral surface cavernous bodies and, meeting with the muscle of the same name of the opposite side, along the midline spongy body forms a seam. The muscle contributes to the eruption of sperm and urination. In women, the muscle covers the opening of the vagina ( rice. 2 ) and with its contraction narrows it. The deep muscles of the urogenital diaphragm include the deep transverse perineal muscle and the external urethral sphincter. The deep transverse perineal muscle strengthens the urogenital diaphragm. In its thickness, in men, the bulbourethral glands lie, in women - large glands of the vestibule. The external urethral sphincter surrounds the urethra; in women, this muscle also covers the vagina.
The pelvic diaphragm is formed by the levator ani muscle, the coccygeal muscle, and the external anal sphincter. The levator ani muscle covers the rectum on both sides; in women, part of the fibers is woven into the wall of the vagina, in men - into the prostate gland. The muscle strengthens and elevates the pelvic floor, elevates the final section of the rectum, in women it narrows the entrance to the vagina. The coccygeal muscle complements and strengthens the muscular arch of the pelvic diaphragm from behind. The external anal sphincter surrounds the anus, closing it when contracted.
The fascia covering the muscles of the urogenital diaphragm, at the posterior edge of the superficial transverse muscle of the perineum, is divided into three ( rice. 3 ): upper, covering the inner (upper) surface of the muscles of the genital diaphragm; lower, passing between the deep and superficial muscles of the perineum; superficial, covering the bottom of the superficial muscles P. and in men passing into the fascia of the penis. The lower and upper fasciae at the anterior edge of the transverse smooth muscle of the perineum form the transverse ligament of the perineum.
In the area of the perineum on both sides of the anus there is a paired depression - the ischiorectal fossa. It has a prismatic shape and is filled with adipose tissue, contains internal genital vessels and the pudendal nerve. Its apex corresponds to the lower edge of the tendinous arch of the pelvic fascia. The lateral wall is formed by the lower 2/3, obturator internus muscle and the inner surface of the ischial tuberosity. The medial wall is formed by the lower surface of the levator ani muscle and the external sphincter of the anus; the back wall - the rear bundles of the muscle that lifts the anus, and the coccygeal muscle; anterior - transverse muscles of the perineum. The fiber that fills the ischiorectal fossa continues into the adrectal tissue.
The blood supply to the perineum is carried out by branches of the internal pudendal artery, which branches off from the internal iliac artery. Venous blood flows through the veins of the same name into the internal system. iliac vein. Lymphatic vessels deliver lymph to the superficial inguinal lymph nodes. The innervation of the perineum is provided by the branches of the pudendal nerve (from the sacral plexus).
With deep and extensive wounds often develops phlegmon extending to the pelvic tissue. It is possible to join anaerobic infection.
Diagnosis of perineal injuries is based on characteristic clinical symptoms and data from wound probing, digital examination of the rectum, anoscopy, rectoscopy and x-ray examination.
Treatment of perineal injuries depends on their nature. In case of bruises of the perineum without damage to the rectum or bladder (urethra), conservative treatment is used - rest, cold perineum in the first days, then thermal procedures (see. bruises). Hematomas that do not tend to increase are also treated conservatively; with a growing hematoma, an operation is performed to evacuate it and hemostasis (see. Hematoma). Superficial wounds of the perineum, given their increased infectivity, are widely dissected, excised non-viable tissues and drain well (see. Drainage).
When wounding the perineum with extensive damage rectum a colostomy is applied, and the perineal wound is treated with antiseptics and drained. When a perineal injury is combined with an injury to the bladder (urethra), a high suprapubic fistula is formed, urinary streaks are drained (see Fig. Bladder). With combined wounds of the perineum, rectum and bladder (urethra), complicated by pelvic phlegmon, the perineal wound is widely dissected and drained, a colostomy and a high fistula of the bladder are applied.
Genital warts of the perineum - benign viral defeat skin. They appear in the form of tiny pink papules, which then grow and, after merging, resemble cauliflower. The formation has a soft texture and a narrow base in the form of a leg. Treatment - lubrication 20% alcohol solution podophyllin or surgical removal within healthy tissues.
Tuberculosis of the skin of the perineum is observed in patients with severe forms of tuberculosis of the internal organs. Small yellowish-red nodules appear in the crotch, turning into sores, which, merging, form large, sharply painful ulcers with a bottom covered with grayish pus. Treatment should be directed primarily to the elimination of the main focus of tuberculosis (see. Tuberculosis extrapulmonary).
Syphilis of the perineum manifests itself in the form of primary syphilomas correct form dense texture, reddish color. Then there is erosion or an ulcer. Secondary syphilis in the form of papular syphilis is often localized on the perineum. Syphilitic gummas (tertiary syphilis) of the perineum are located in the subcutaneous tissue, open spontaneously and form ulcers with undermined edges and scanty discharge. specific treatment (see Syphilis).
Perineal hernias are rare. They are observed in persons engaged in heavy physical labor, especially those with a weak pelvic diaphragm or who have suffered a perineal injury. There are anterior and posterior perineal hernias. They have the appearance of a tumor-like formation that occurs in the perineum during physical exertion, walking, coughing and is easily reduced. On palpation, a defect in the muscles of the perineum is detected. Treatment is surgical, closing the hernial orifice in the pelvic diaphragm.
Tumors. In the area of the perineum, various tumors can occur (neurogenic, vascular, connective tissue); more common lipoma. The tumor has a rounded, sometimes flattened shape, located under the skin of the perineum. On palpation, it is soft, mobile, painless. Grows slowly. Treatment is operative.
The mesenchymoma of the perineum is less commonly observed - a tumor of a complex structure from mesenchymal derivatives. It has a soft texture, moderately mobile and slightly painful, covered with a capsule.
In the diagnosis, puncture biopsy and X-ray methods of investigation (survey radiography, proctography, parietography). In some cases, it becomes necessary to differentiate mesenchymoma with perineal hernia and teratoid formations. Treatment is operative.
Bibliographer.: Aminev A.M. Guide to proctology, v. 3, p. 441, Kuibyshev, 1973; Human Anatomy, ed. M.R. Sapina, vol. 2, p. 131, M., 1986; Lenyushkin A.I. Proctology of childhood, p. 254, M., 1976.

