Displacement and compression of the brain stem. Dislocation syndrome - brain dislocation: types, causes, diagnosis and treatment
Acute pathological processes in dislocation syndromes involve the same anatomical structures with stereotypical clinical manifestations. In other words, the clinical picture of acute dislocation syndrome does not depend on the etiology of the process. The difference is in clinical manifestation in different patients depends on the rate of its development, location and volume.
The fact is that dislocation syndromes are essentially internal hernias of the brain, that is, invagination of its parts into holes and crevices, formed by bones and dura mater. There are 3 degrees of brain dislocation: protrusion, herniation and pinching. There are lateral and axial (along the axis of the brain stem) dislocations of the brain.
Drawing a parallel with hernias, it should be remembered that sharp violation the patient’s life activity arises not from the fact of the existence of a hernia, but from its infringement. Infringement represents a protrusion, which is accompanied by cessation of blood flow due to compression of blood vessels.
Types of dislocation syndromes
In the majority medical literature 4 types of dislocation syndromes are described (1-4), which have highest value V clinical practice, as they may be accompanied by a significant deterioration in the patient’s condition. At the same time, the Great Medical Encyclopedia identifies 8 dislocation syndromes. Some sources also describe external dislocation (number 9), which is a bulging of parts of the brain through a traumatic defect of the skull.
- Displacement of the cerebral hemispheres under the falciform process
- Temporotentorial displacement
- Cerebellar-tentorial displacement
- Displacement of the cerebellar tonsils in the foramen magnum of the occipital bone
- Displacement of the cerebral pons through the foramen of the tentorium cerebellum
- Filling the middle and side tanks of the bridge
- Bias posterior section corpus callosum in the dorsal direction into the cistern of the same name
- Displacement of the gyri of the frontal lobe into the chiasm cistern
- External brain dislocation
Displacement of the cerebral hemispheres under the falciform process
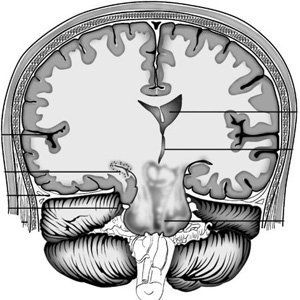
When the brain is compressed on one side by an acute volumetric process, with an increase in cerebrospinal fluid pressure in one lateral ventricle due to acute occlusive hydrocephalus, a difference in cerebrospinal fluid pressure develops between the right and left lateral ventricles. This creates conditions for the dislocation of the hemisphere big brain in the transverse direction into the gap between the falx cerebrum and the corpus callosum. The wedged area is mainly the cingulate gyrus and its adjacent areas. Thus, the cingulate gyrus fills the cistern of the corpus callosum. The cingulate gyrus, bulging in the opposite direction, displaces the anterior cerebral arteries, pressing them against the falciform process. The lateral and third ventricles are deformed. Perifocal edema can generalize due to slowing of blood circulation, as a result of compression of arteries and veins. All this leads to insufficient supply to the brain tissue nutrients and oxygen, which leads to the development of even greater edema-swelling of the brain and to even greater dislocation. These processes can lead to blockage of liquor outflow. The cerebrospinal fluid produced in the lateral ventricles, having no outflow tract, creates an area of distension in the supratentorial space with the development of temporotentorial herniation, which leads to compression of the midbrain.
Temporotentorial and cerebellartentorial herniation
These 2 dislocation syndromes can be combined due to the commonality of the affected structures and the correspondingly developing clinic. They differ in the location (sub- or supratentorial) of the area of distension. Temporotentorial herniation is a protrusion into the tentorial foramen (Bishat's fissure) of the area temporal lobe brain and primarily the medial areas of the hippocampal gyrus, partly anterior section lingual gyrus and isthmus of the vaulted gyrus. Wedged between the free edge of the cerebellar tentorium and the oral parts of the brainstem, the area of the temporal lobe can occupy different positions in relation to the trunk: anterior - when located in front of the trunk; anterolateral - when located anterior to the trunk and along its anterior quadrant, posterolateral, posterior. Herniation of brain areas into the tentorial foramen can occur not only from the side cerebral hemispheres brain, but also in the opposite direction, that is, from the back cranial fossa. In such cases, a portion of the cerebellum protrudes between the free edge of the tentorium and the quadrigeminal region. This wedging is called cerebellar-tentorial. It occurs during pathological processes in the posterior cranial fossa. The occurrence of temporo-tentorial and cerebellar-tentorial herniations is inevitably associated with a displacement of the trunk in the opposite direction, which depends on the size and characteristics of the herniation.
The ipsilateral oculomotor nerve is compressed - the pupil dilates after a short-term miosis.
Lateral displacement of the homolateral parahippocampal gyrus causes midbrain move across the midline towards the opposite edge of the tentorium. This small change in midbrain configuration can lower the patient's level of consciousness and cause targeted arousal.
Eventually, the globus pallidus, internal capsule, and thalamus opticum on the homolateral side move caudally, and the parahippocampal gyrus protrudes beyond the edge of the cerebellar tentorium into the subtentorial space. The mamillary bodies are wedged into the narrowed interpeduncular fossa. Under these conditions, the midbrain experiences intense pressure, which causes the development of coma. The midbrain may be pressed against the opposite edge of the tentorium so tightly that the descending motor fibers in the compressed cerebral peduncle are damaged. The hemiplegia caused by this type of herniation is not contralateral, but homolateral in relation to the volumetric process - Kernoghan's cerebral peduncle syndrome . Due to compression, hemorrhages occur in the inferotemporal and occipital regions of the brain, midbrain, which can often lead to irreversible consequences and death of the patient
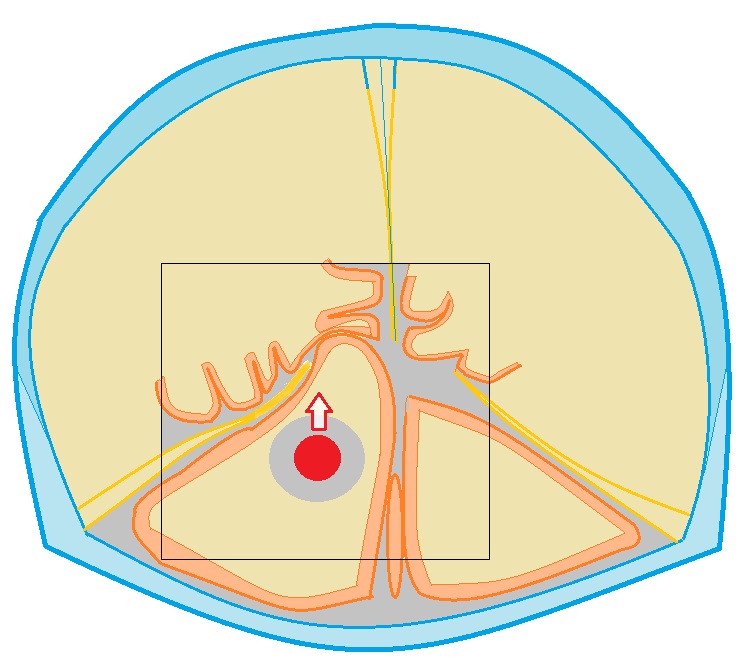
Herniation of the cerebellar tonsils into the foramen magnum
The tonsils of the cerebellum, shifting into the foramen magnum, sometimes reach the level of the second cervical vertebra. Wedged between the caudal part of the medulla oblongata, the adjacent part of the spinal cord and the occipito-cervical ring, they tightly envelop and compress this part of the trunk from the dorsal surface.
This causes disturbances cerebral circulation, inevitably leading to hypoxia and to an even greater increase in edema-swelling of the brain. Thus, a vicious circle is closed, which leads to the progression of compression of the brain stem, which leads to disruption of the function of the vital centers of blood circulation and respiration embedded in them and, as a consequence, to the death of the patient.
Displacement of the cerebral pons through the foramen of the tentorium cerebellum
The pons is displaced in the oral direction into the interpeduncular cistern.
Filling the middle and side tanks of the bridge
It occurs as a result of pressing the brain bridge against the slope of the base of the skull.
Displacement of the posterior part of the corpus callosum in the dorsal direction into the cistern of the same name
Occurs with closed hydrocephalus of the brain, which can also occur with the above dislocation syndromes. Due to high blood pressure in the ventricles, the corpus callosum is displaced into the cistern of the same name. The free edge of the falx forms a notch on the corpus callosum. Since this dislocation syndrome occurs against the background of deep disturbances in the vital functions of the body, it is rarely described in the literature devoted to this problem.
CSF circulation disorders
Brain dislocations are dangerous not only by the development of cerebrovascular accidents. There is also displacement and compression of the cerebrospinal fluid-containing spaces, both as a whole and in their individual parts, in particular the cerebral aqueduct, the fourth ventricle, etc. Compression leads to disruption of the cerebrospinal fluid circulation. The normal state of the cerebrospinal fluid pathways is disrupted due to their narrowing at the level of the tentorial foramen or foramen magnum, which leads to the development of hydrocephalus. Naturally, if the outflow of cerebrospinal fluid from the ventricles is disrupted, a pressure gradient occurs between the ventricles and the spinal sac. This pressure difference leads to even greater displacements of the brain stem in the caudal direction, to the development of new dislocation syndromes.
Clinic
At temporotentorial and cerebellartentorial herniations oculomotor disturbances appear (horizontal, rotatory, vertical nystagmus, discrepancy eyeballs, Hertwig-Magendie symptom, partial or complete paresis of upward or sideways gaze or complete immobility of the eyeballs, weakened or absent reaction of the pupils to light, etc.). Unilateral pyramidal insufficiency, which occurs during an acute space-occupying process (Kernohan's cerebral peduncle syndrome), becomes bilateral. This fact indicates the involvement of the second leg of the brain in the pathological process. The clinical picture of these types of dislocations depends on which arteries to which areas of the brain are compressed in the tentorial foramen.
Compression of vessels leading to basal ganglia extrapyramidal system, leads to dysregulation muscle tone first in the form of increased extensor tone, the appearance of cogwheel symptoms. Then hormetonia develops, muscle rigidity and as a consequence, muscle atony is evidence of disconnection of the midbrain from the overlying sections. Diencephalic disorders are detected in the form of tachycardia, which replaces bradycardia. The ECG is recorded various shapes arrhythmias, infarction-like ischemia and other disorders that are functional in nature, secondary to cerebral pathology and disappear without a trace when eliminated acute period. Tachypnea, hyperthermia also occurs, in some patients up to 39-40°C, hyperemia and greasiness skin and others. The consciousness of patients is depressed, up to coma varying degrees expressiveness.
Displacement of the tonsils of the cerebellum into the foramen magnum clinically the most severe. In this case, vital centers suffer, primarily the centers of respiration and circulation. Breathing problems occur central genesis varying degrees, which depends on the rate of development, degree and duration of herniation. These disorders are detected in tachypnea (at the beginning of the process), which then develops into deeper forms of pathology, up to Cheyne-Stokes breathing, Biota, terminal types and apnea. In parallel with the breathing disorder, the depth of the disturbance of consciousness increases, and anabolic disorders develop. Swallowing is grossly impaired, the pharyngeal reflex decreases or disappears - develops bulbar syndrome. Vascular tone decreases. Arterial hypotension develops.
Diagnostics
Diagnostic methods:
- Echoencephalography - determines the degree of displacement of the midline structures in one direction or another. It should be taken into account that according to Echo-EG data, only lateral dislocation can be assumed (displacement of the cerebral hemispheres under the falciform process), since according to its data it is impossible to diagnose axial dislocation of the brain.
- barbituric anesthesia
- moderate hypothermia
- periodic deep hyperventilation
- glucocorticoids
- Big medical encyclopedia. Main Ed. B.V. Petrovsky. Ed. 3rd. M., "Owls. Encyclopedia", 1977 p. 347-349
- Duus P. Topical diagnosis in neurology Anatomy. Physiology. Clinic - M. IPC "Vazar-Ferro", 1995 p. 173-179
- Lebedev V.V., Bykovnikov L.D., Kariev M. Emergency Diagnostics and assistance in neurosurgery - T.: Medicine 1988 p. 44-67
- Lebedev V.V., Krylov V.V. Emergency neurosurgery: A guide for doctors. - M.: Medicine, 2000 p.103-141
- Misyuk N. S., Evstigneev V. V., Rogulchenko S. M. Displacements and infringements of the brain stem. Minsk, "Belarus", 1968
- Neurotraumatology. Directory / Edited by: Academician of the Russian Academy of Medical Sciences A.N. Konovalov, Professor L.B. Likhterman, Professor A.A. Potapov. - M.: IPC “Vazar-Ferro”, 1993
- Practical neurosurgery: A guide for doctors / Ed. B.V. Gaidar. - St. Petersburg: Hippocrates, 2002
Treatment
The first and indispensable condition for treating a dislocation is to eliminate the cause that caused it.
Non-surgical measures used for dislocation syndromes include:
An operation for life-saving reasons in the development of cerebral edema and processes that lead to the dislocation of some parts of the brain in relation to others is decompressive craniotomy. To remove the pathological focus, a wide (minimum 5-6 x 6-7 cm) decompressive craniotomy is performed, which does not necessarily have to be resection, but definitely decompressive. With temporotentorial herniation, trepanation is performed in the temporoparietal region as low as possible. With bilateral symptoms, decompressive trepanation is performed on both sides. After removal of the pathological focus, the dura mater is not sutured.
Also, to reduce intracranial pressure and, accordingly, reduce the risk of developing life-threatening herniation processes, drainage of the ventricular system is performed. The anterior or posterior horn is punctured from standard points(Kochera or Dandy). The effect of puncture of the ventricles of the brain is stronger if the drainage is carried out more early stages wedging. With a lateral displacement of the ventricles, it is not easy to get into the displaced and compressed ventricle of the brain. Puncture of the hydrocephalic ventricle on the side opposite to the lesion (“healthy”) with a remaining pathological focus is fraught with an increase in dislocation and an increase in vital disturbances.
Literature
The brain, as opposed to, for example, organs abdominal cavity or chest, is located in the cranial cavity, the volume of which is static and cannot increase if necessary. The bones of the skull form a rigid “frame”, due to which, with increasing pressure inside the skull, more soft structures, located inside it, are pushed back and compressed in the holes and under the outgrowths of the hard meninges. It is necessary to distinguish between the concepts of “displacement” and “wedging”. In the first case we're talking about about the dislocation of brain structures under the influence of some volumetric process that creates excess pressure on the opposite side (without infringement), in the second - displacement of the brain into the natural openings of the skull or under the outgrowths of the membrane with possible infringement.
Reasons leading to the occurrence of dislocations of the brain
- Ischemic stroke. Dislocations at ischemic stroke from small to moderate, depending on the volume of the lesion and the severity of cytotoxic cerebral edema. However, even a small dislocation, for example, during a stroke localized in the cerebellum, can cause breathing problems and cardiac activity due to compression of the medulla oblongata.
Ischemic stroke in the right middle basin cerebral artery. CT scan of the brain. When describing it, it should be noted that the entire parietal and frontal lobe on the right is in edema, as a result of which the right lateral and 3rd ventricle are completely compressed. There is a slight dislocation of the middle structures to the left.
- Hemorrhagic stroke. Intracerebral hematomas lead to more pronounced displacements of brain structures, clearly visible on computed tomography and MRI. The degree of displacement depends on the size of the hematoma and the severity of perifocal cerebral edema. 
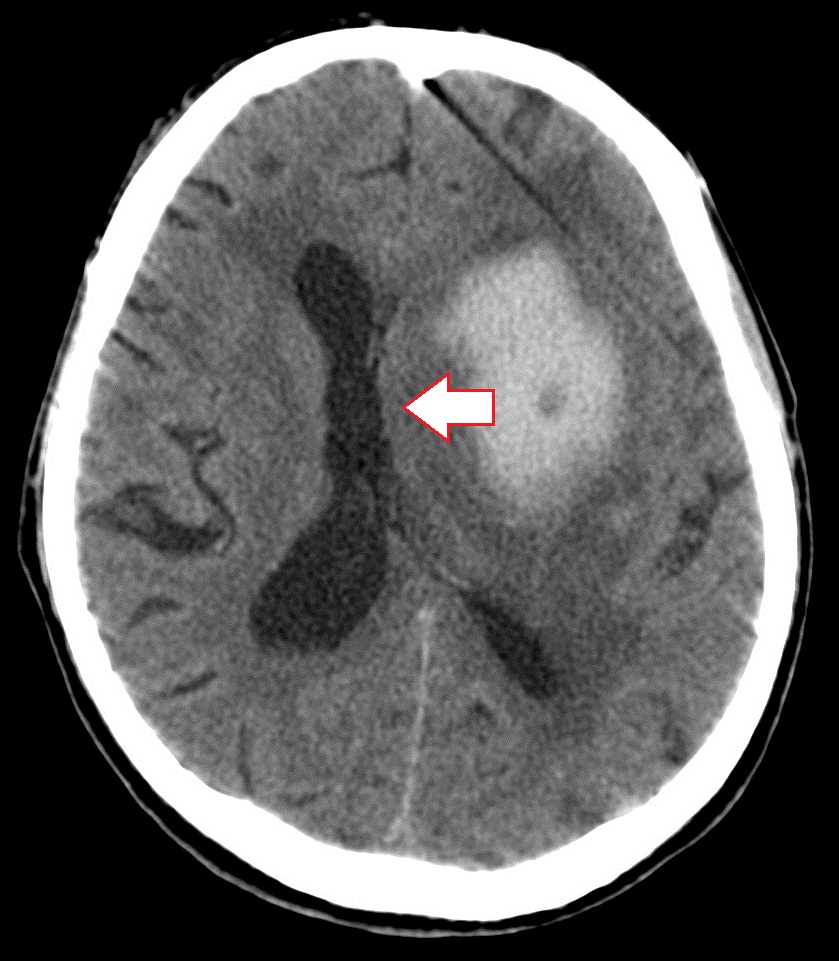
CT signs of lateral dislocation syndrome in hemorrhagic stroke(left). The left lateral ventricle and the 3rd ventricle of the brain are compressed, the right lateral ventricle in both cases appears dilated. Pronounced dislocation of the middle structures to the right side.
- Subdural hematoma. Causes significant dislocations of brain structures, since the volume of blood in subdural hematomas is large and can reach several hundred ml. Both acute and chronic subdural hematoma lead to displacement of the midline structures and other types of dislocations.

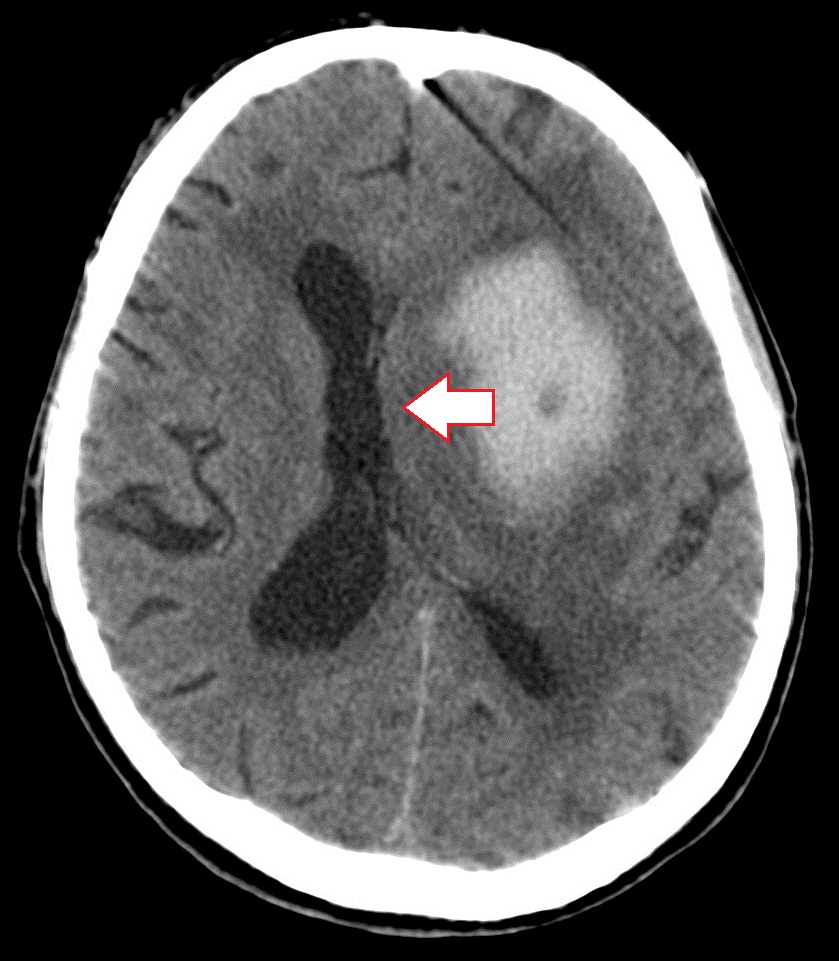
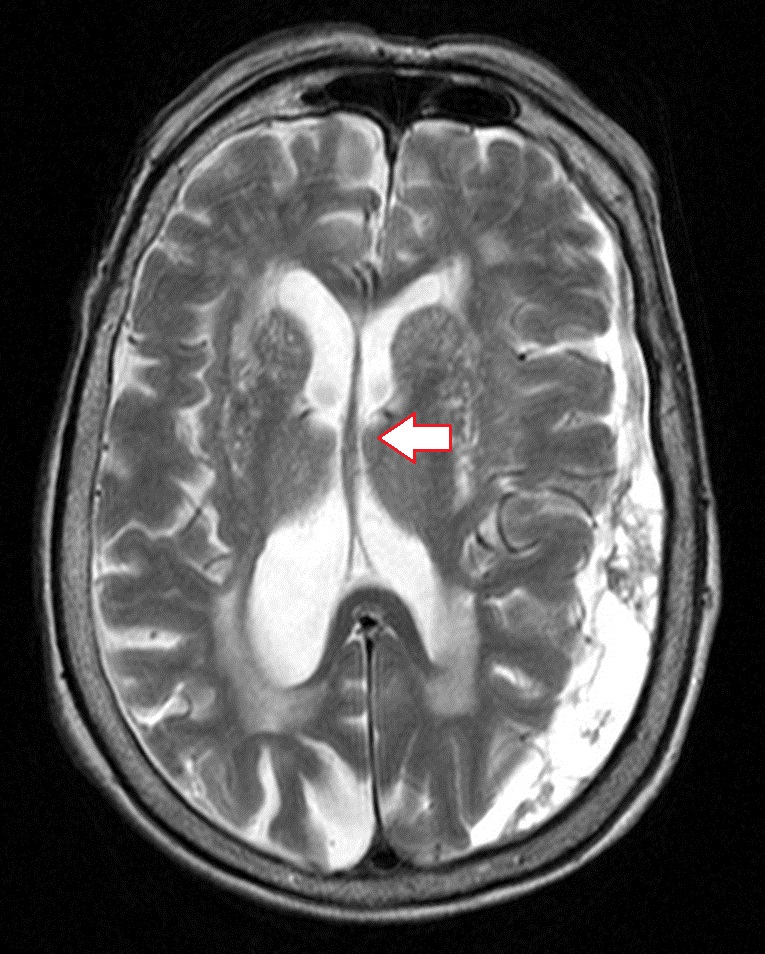
Dislocation syndrome (direction of displacement is indicated by an arrow) with a left-sided acute subdural hematoma (far left image). Marked displacement of the ventricles of the brain to the right. The image in the middle shows a dislocation of brain structures caused by a chronic subdural hematoma; the image on the far right shows an MRI of the brain; decoding revealed a slight displacement of the median structures to the right due to a chronic subdural hematoma.
- Epidural hematoma. It usually occurs with fractures of the skull bones, leads to the appearance of local displacements, and almost never causes significant dislocations, since the volume of blood flowing into the epidural space is small - rarely reaching 100 ml.
- Brain contusion. By its nature, the contusion focus is an intracerebral hematoma, in combination with areas of crushing of the brain substance, and areas of ischemia resulting from damage to the arteries. The severity of dislocations of brain structures in CT and MRI studies depends on the volume of the hematoma, as well as the size of the area of perifocal edema.

CT scan of the brain. During decoding, a tumor of the left parietal lobe, “mass effect”, displacement of the ventricles of the brain to the left
- Brain tumor. Dislocations are caused by volume pathological tissue, as well as cerebral edema. The larger the tumor and more swelling– the greater the displacement. Tumors of the meninges (meningiomas) behave similar to epidural hematomas - they cause minimal displacement of the brain in a limited area.
— Monoventricular hydrocephalus (due to occlusion of the cerebrospinal fluid ducts). Dilatation of the right or left lateral ventricle leads to displacement of the septum pellucida and other midline structures of the brain in the opposite direction.
Classification of displacements and herniations of brain structures on CT and MRI
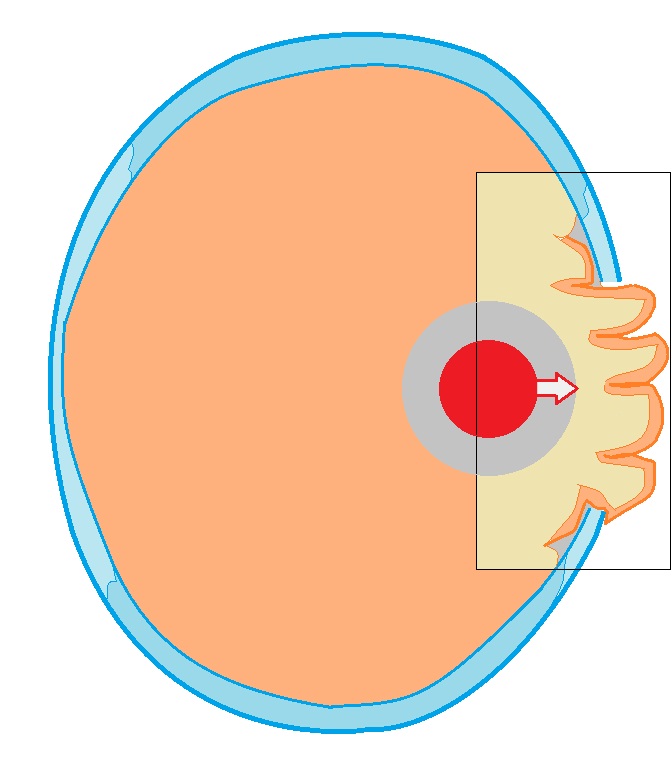
Lateral dislocation of the midline structures of the brain (lateral dislocation syndrome). The type of displacement most often detected on CT and MRI of the head. Measurements are usually made relative to the transparent septum and falxcerebri (or the conventional midline of the head). Dislocations of the midline structures are very often accompanied by compression of the lateral ventricle on one side and expansion on the other. 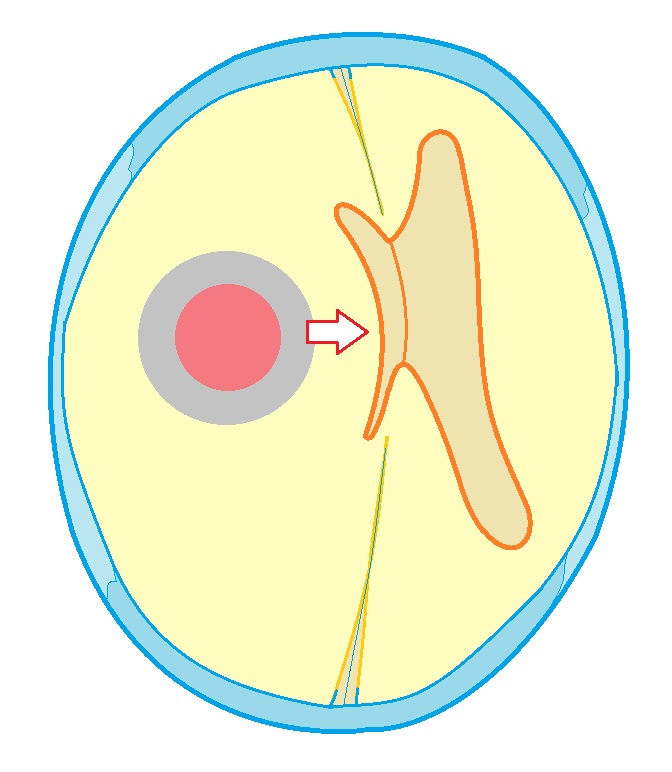 Schematic representation of changes in lateral dislocation syndrome. The pathological focus is marked in red, the direction of pressure is marked with an arrow. Falxcerebri and lateral ventricles are displaced to the side, multiventricular hydrocephalus occurs against the background of compression of the ventricle closest to the pathological process.
Schematic representation of changes in lateral dislocation syndrome. The pathological focus is marked in red, the direction of pressure is marked with an arrow. Falxcerebri and lateral ventricles are displaced to the side, multiventricular hydrocephalus occurs against the background of compression of the ventricle closest to the pathological process.
Herniation of the frontal lobe under the falx cerebri occurs due to space-occupying processes localized in the frontal lobe of the brain. As a result, one of the gyri (or several) of the frontal lobe on the medial side is wedged and pinched under the “sickle” of the brain.
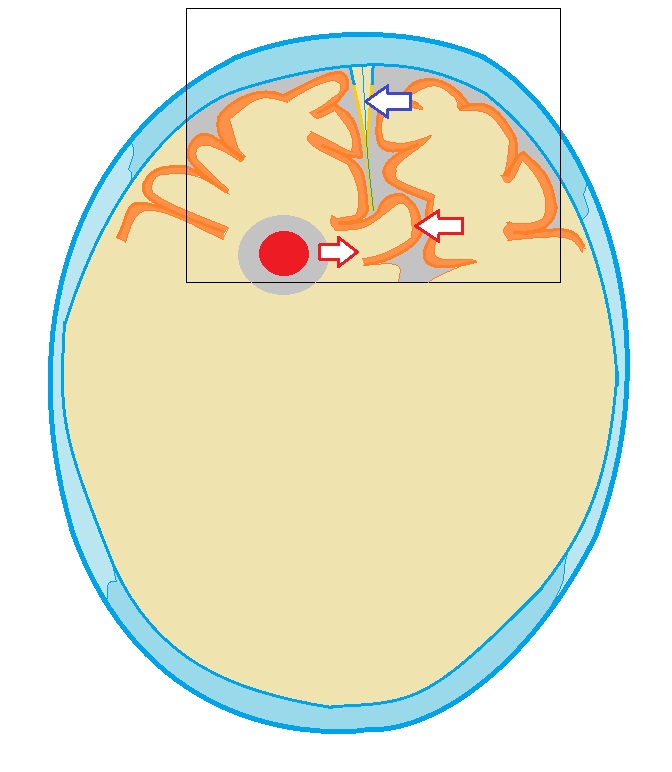 Wedging of the medial gyrus of the frontal lobe under the "sickle" of the brain. The volumetric pathological process that caused the herniation is marked in red, the arrow from it indicates the direction of displacement, and the blue arrow indicates the “sickle” of the brain.
Wedging of the medial gyrus of the frontal lobe under the "sickle" of the brain. The volumetric pathological process that caused the herniation is marked in red, the arrow from it indicates the direction of displacement, and the blue arrow indicates the “sickle” of the brain.
Temporo-tentorial herniation. With volumetric processes in the middle cranial fossa, displacement of the temporal lobe and herniation of the hippocampus under the tentorium of the cerebellum may occur.
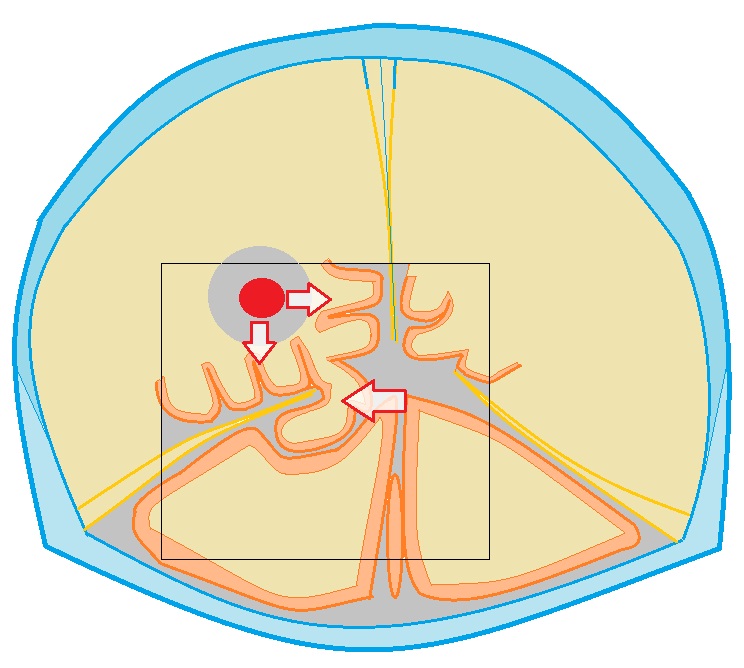
Temporo-tentorial herniation (diagram). The volumetric pathological process is marked in red, the arrows indicate the direction of displacement. The gyrus of the temporal lobe, displaced under the tentorium, was also noted.
Cerebellar-tentorial herniation: one of the cerebellar hemispheres is displaced upward and located above the tentorium, closely adjacent to temporal lobe brain
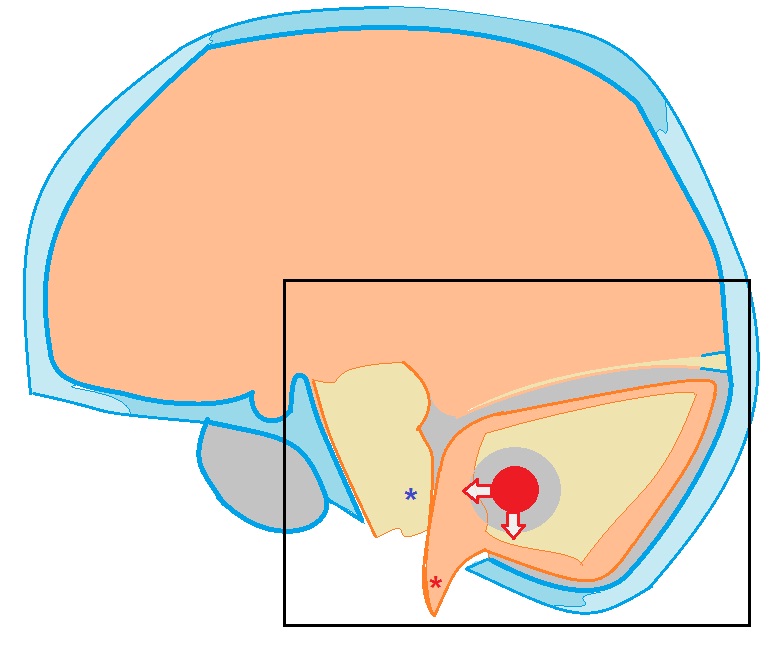
Intrusion of the tonsils of the cerebellum into the foramen magnum occipital bone can occur with space-occupying processes (tumors) of the cerebellum, with strokes localized in the cerebellum, cerebellar hematomas. The tonsils (marked with a red asterisk) protrude into the dural infundibulum and are located below the plane of the foramen magnum. The fourth ventricle is compressed and deformed. This condition is also dangerous due to the possibility of compression of the brain stem (marked with an asterisk of blue color) with the development of respiratory and cardiac disorders).
External dislocation of the brain (diagram). Occurs after resection craniotomy. An area of the brain bulges into the burr hole and can be compressed by its edges
(Late Latin dislocatio displacement, movement)
displacement of the brain due to changes in intracranial topography during various pathological processes in the central nervous system. The causes of D. g. m. are an increase in intracranial pressure, an increase in the volume of the brain, or deformation of its various parts. In case of intracranial tumor or hematoma, brain abscess, traumatic brain injury accompanied by cerebral edema, the syntopy of brain structures changes and is redistributed intracranial pressure in the spaces separated by the tentorium cerebellum and the greater falciform process of the dura mater (falx cerebri). Dislocation of the brain may be accompanied by prolapse and pinching of the cerebellar tonsils in the foramen magnum and superior part spinal canal with the development of life-threatening nuchal herniation syndrome ( rice. 1
). It is typical for tumors of the posterior cranial fossa, but can also develop with tumors located above the tentorium of the cerebellum. Clinical picture in this syndrome is caused primarily by compression of the medulla oblongata and the associated violation of vital important functions. With occipital herniation, it sharply intensifies headache, especially in the occipital region; vomiting, dizziness, which increases with changes in the position of the head and body, forced positioning of the head, which helps to reduce headaches, are noted, meningeal syndrome, choking when taking liquid food, hiccups, increased sweating, increasing disturbances in breathing rhythm (arrhythmic, intermittent, Cheyne-Stokes type) and activity of cardio-vascular system. Symptoms of intracranial hypertension are expressed (see Intracranial hypertension) -
progressive lethargy, congested discs optic nerves, diplopia, decreased corneal reflexes, sense of smell, hearing, etc. The rapid increase in herniation phenomena leads to the development of coma and respiratory arrest. With tumors of the temporal lobe of the brain, and less commonly with tumors of the frontal or occipital lobes, the brain may be pushed from front to back and medially. In this case, the medial parts of the hemispheres are wedged into the foramen of the tentorium of the cerebellum, squeezing the brain stem passing through this hole ( rice. 2
). Such tentorial herniation, depending on the degree and symmetry of compression of the brainstem, may initially clinically manifest itself as intracranial hypertension syndrome and symptoms of unilateral damage to the brainstem. However, soon the brainstem symptoms become bilateral, headache and vomiting intensify, and the disturbance of consciousness deepens. Trunk syndrome of tentorial herniation is characterized by paresis of upward gaze, absence of the pupillary light reflex, weakness of convergence, the presence of bilateral pathological pyramidal reflexes, etc. Compression at the base of the brain of the oculomotor nerve causes ptosis, strabismus, dilation of the pupil on the affected side. The progression of the phenomena of tentorial herniation leads to the development of paralysis, decerebrate rigidity (Decerebrate rigidity) ,
coma. Brain dislocation caused by swelling around the site of brain contusion, intracranial hematoma, a tumor of the parietal, frontal lobe, etc., may involve a lateral displacement of the median structures (around the third ventricle, etc.) of the brain and medial parts of the cerebral hemispheres. In this case, a herniation occurs under the large falciform process of the dura mater. Displacement of the midline structures of the brain aggravates the severity of clinical symptoms caused by the focal process and enhances vegetative-vascular, endocrine-metabolic and metabolic disorders. The development of D. g.m. should be suspected in cases of acute deterioration of the condition of patients with intracranial processes, primarily of a tumor nature, accompanied intracranial hypertension, hydrocephalus (Hydrocephalus) ,
occlusion syndrome (occlusion syndrome) .
Echoencephalography helps to clarify the diagnosis, CT scan heads, craniography. Diagnostic spinal tap contraindicated due to the possibility of increasing the dislocation of the brain. Suspicion of occipital or tentorial herniation requires immediate administration of dehydrating agents and an urgent decision on the issue of neurosurgical operation, which is the only radical therapeutic measure. Question of character surgical intervention must be addressed before vital signs develop. Lateral dislocation of the brain can sometimes be eliminated by symptomatic means (corticosteroid and dehydrating drugs), puncture of the cerebral ventricles followed by neurosurgical surgery or radiation therapy. The prognosis is always very serious, depending on the location and nature of the main process that caused the dislocation of the brain. Bibliography: Blinkov S.M. and Smirnov N.A. Displacements and deformations of the brain, L., 1967; Diseases nervous system, ed. P.V. Melnichuk, vol. 1-2, M., 1982; Multi-volume guide to surgery, ed. B V. Petronsky, vol. 3, book. 1. p. 87, M., 1968.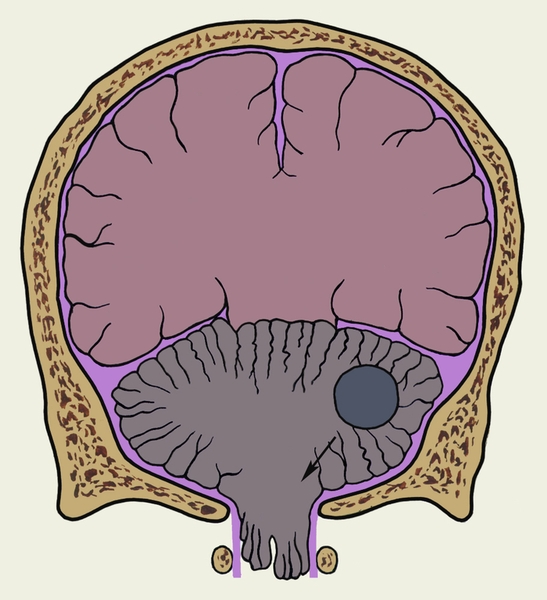
- - displacement of the brain associated with deformation and displacement medulla under the influence of increased intracranial pressure, cerebral edema, hydrocephalus, hemorrhage, tumor and...
- - An abscess that forms in the brain tissue as a result of pathogens entering them purulent infection from other foci or with traumatic brain injury...
Medical encyclopedia
- - metastatic brain abscess, in which the source of metastasis is the inflammatory endocardium; occurs in children with birth defects blue type hearts, mainly with tetralogy of Fallot...
Medical encyclopedia
- - Brain abscess that develops as a result of the spread of infectious agents from a nearby focus of purulent inflammation...
Medical encyclopedia
- - see Hydrocephalus...
Medical encyclopedia
- - common name cavities located in the brain, lined with ependyma, communicating with each other and with the subarachnoid space and containing cerebrospinal fluid...
Medical encyclopedia
- - see Compression of the brain...
Medical encyclopedia
- - closed damage brain, characterized by the appearance of a focus of destruction of its tissue and manifested by neurological and psychopathological symptoms according to the localization of the focus...
Medical encyclopedia
- - a significant increase in brain volume, accompanied by an increase in intracranial pressure and dysfunction of the nerve centers...
Medical encyclopedia
- - a pathological process characterized by excessive accumulation fluids in brain tissue. The resulting increase in brain volume leads in most cases to an increase in intracranial pressure...
Medical encyclopedia
- - cm....
Medical encyclopedia
- - see Cerebral hemisphere...
Medical encyclopedia
- - a combination of signs of increased intracranial pressure with focal neurological symptoms, caused by the presence of a space-occupying formation in the cranial cavity...
Medical encyclopedia
- - clinical form mild closed craniocerebral injury, characterized by a predominance of reversible functional changes brain - see Traumatic brain injury...
Medical encyclopedia
- - part of the base of the brain containing the nuclei cranial nerves and vital centers...
Medical encyclopedia
- - see Brain contusion...
Medical encyclopedia
"Brain dislocation" in books
Grandfather Matvey
From the book The Lord Will Rule author Alexander AvdyuginGrandfather Matvey Grandfather Matvey old. He himself says: “They don’t live that long these days.” He speaks correctly, probably because there are no peers left in the district, especially those who went through the war: with trenches, attacks, injuries and other fears, which we can now judge only from books
5. Levi Matvey
From the book Woland and Margarita author Pozdnyaeva Tatyana5. Levi Matthew At the foot of the Mount of Olives, in Bethphage, Yeshua Ha-Nozri met his only disciple Levi Matthew. Yeshua tells about this during interrogation, and although the Yershalaim topography does not indicate the proximity of this small village to the Olivet
Matvey
From the book The Secret of the Name the author Zima DmitryMatvey Meaning and origin of the name: from the Hebrew name Matthew - God's gift granted by the Lord. Energetics and Karma of the name: today the name Matvey is quite rare, although it is possible that it may soon become fashionable. At least today they are
MATVEY
From the book 100 happiest Russian names author Ivanov Nikolay NikolaevichMATVEY Origin of the name: "granted by God" (Jewish). Name day (according to the new style): July 13; August 22; October 11, 18; November 29. Positive character traits: calmness, responsibility, harmony, absence of contradictions, complexes. Matvey is reliable,
Matvey Parisian
From the book Russian-Livonian War of 1240-1242 author Shkrabo DMatthew of Paris Matthew of Paris, French author of the 1st half. 13th century, wrote that the Danish king sent princes Knut and Abel with an army and settlers to settle the Novgorod possessions devastated by the Tatars. He mixed two events: the German-Danish campaign of 1240
Cat Matvey
From the book Knitted toys author Kaminskaya Elena AnatolyevnaCat Matvey Such a knitted cat can not only become your baby’s favorite toy, but also a wonderful gift for a friend for the birth of a child. Cat Matvey You will need 50 g of yarn of the main color, 20 g of white yarn for the face and paws,
Matvey
From the book All the Monarchs of the World. Western Europe author Ryzhov Konstantin Vladislavovich author From the book Orthodox names. Choosing a name. Heavenly patrons. Saints author Pecherskaya Anna IvanovnaMatvey Name meaning: from ancient Hebrew. Mattityahu - “gift of Yahweh” (“given by the Lord”). Main features: honesty, modesty, morality. Character traits. In his family, Matvey is usually a long-awaited child; his parents have high hopes for him. He
Brain dislocation (dislocation syndrome) is a pathology that occurs as a result of displacement of brain tissue in relation to solid formations. This causes the space inside the skull to be restricted and divided.
What causes brain dislocation?
The development of the disease is caused by processes that increase pressure inside the skull:
- abscesses;
- tumors;
- cerebral edema;
- hematomas.
In some cases, cranial hernias are observed, the nature of which is congenital. There are three stages of dislocation syndrome:
- protrusion;
- wedging;
- infringement.
 When a certain area of brain tissue protrudes into a large hole located in the back of the head, or in the cracks, the limit of which is the dura mater of the brain, it develops venous stasis. Also to the number possible consequences include local swelling and small effusions of blood.
When a certain area of brain tissue protrudes into a large hole located in the back of the head, or in the cracks, the limit of which is the dura mater of the brain, it develops venous stasis. Also to the number possible consequences include local swelling and small effusions of blood.
In the wedged area, the growth of local edema does not stop, as a result of which its size increases and its shape becomes hernial.
The pathology in question exists in two types:
- Lateral dislocation. Under the conditions of a literal supratentorial process, the brain area is displaced under the falciform process.
- Axial dislocation (the brain is displaced along the axis into the foramen of the tentorium of the cerebellum and into the foramen magnum in the occipital region).
Forms of brain dislocation
Let us consider the forms of dislocation syndrome, the significance of which is decisive.
Displacement of the cerebellum into the cerebellomedullary cistern
As a rule, this process indicates neoplasms of the posterior cranial fossa. There are known cases of its development when there is cerebral edema. There are signs of increased intracranial pressure:
- severe headache;
- vomit;
- nausea.
Bulbar disturbances are possible.
Dislocation of parts of the temporal lobe (basal) into the foramen of the tentorium of the cerebellum
The result of this type of dislocation is flattening and compression of the adjacent parts of the midbrain.
Impactions of this kind can be either bilateral or unilateral. With this form of dislocation syndrome, intracranial pressure increases sharply. Occlusal crises are possible. In addition, to negative consequences This includes ptosis, mydriasis.
Symptoms of brain dislocation
 With this pathology, in most cases a person is in a coma, but loss of consciousness does not always occur - for example, if the cause of the disorder is a sudden process, infections of the central nervous system and cerebral edema.
With this pathology, in most cases a person is in a coma, but loss of consciousness does not always occur - for example, if the cause of the disorder is a sudden process, infections of the central nervous system and cerebral edema.
Dislocation syndrome can also develop for other reasons, when structures shift at a slower pace. This process is accompanied by the following symptoms:
- convulsions;
- severe headaches;
- transient or persistent decrease in vision;
- repeated vomiting and nausea.
Diagnostic methods
Brain dislocation is diagnosed using the following methods:
- Echoencephalography. Determines how much the midline structures are shifted to any side. Echo-EG data allows us to identify only a lateral dislocation, in which the cerebral hemispheres are displaced under the falciform process.
- Angiography is a method of X-ray contrast examination of blood vessels.
- Computed tomography is a method of layer-by-layer non-destructive examination of an object, or more precisely, its internal structure.
- Magnetic resonance imaging - method radiology diagnostics, which non-invasively allows you to obtain an image internal structures human body.
Treatment
 In order to eliminate the pathological focus, a wide craniotomy is performed, which mandatory is decompressive. However, it may not be resectional. Temporotentorial herniation is an indication for trephination in the lower region of the temporoparietal region. If the symptoms are bilateral, decompressive trepanation is performed on both sides. The dura mater of the brain is not sutured after eliminating the source of pathology.
In order to eliminate the pathological focus, a wide craniotomy is performed, which mandatory is decompressive. However, it may not be resectional. Temporotentorial herniation is an indication for trephination in the lower region of the temporoparietal region. If the symptoms are bilateral, decompressive trepanation is performed on both sides. The dura mater of the brain is not sutured after eliminating the source of pathology.
To lead to normal condition intracranial pressure and minimize the likelihood of herniation processes, life-threatening, the ventricular system undergoes drainage.
The effectiveness of puncture of the cerebral ventricles can be enhanced by drainage carried out on early stages wedging. If the displacement of the ventricles is lateral, entering the brain ventricle (pressed and displaced) is difficult.
In addition, for dislocation syndrome, a number of non-surgical measures can be used: hyperventilation, barbiturate anesthesia, glucocorticoids, moderate hypothermia. Lateral dislocation of the brain in some cases can be eliminated with the help of symptomatic remedies(drugs).
Finally, we bring to your attention a video about a brain tumor - the most common reason development of dislocation syndrome:
According to classical ideas, the symptoms of herniation are caused by the pressure of the brain matter displaced into the rigid openings of the skull (herniation) (as a result of the action of a space-occupying lesion or increased ICP) on other structures of the central nervous system. These ideas have been criticized on the basis of the hypothesis that herniation may be an epiphenomenon that develops later in life. pathological process and is not the cause of the observed changes. However, herniation patterns are used as a useful approximation.
There are several herniation syndromes, 5 of which are the most common:
1. central (transtentorial) herniation
2. temporal herniation (temporal lobe hook)
3. herniation of the cingulate gyrus: the cingulate gyrus can be wedged under the falx (the so-called herniation under the falx). Usually asymptomatic until ACA kinks and occludes, resulting in bilateral infarction frontal lobes. Usually a signal of threatening transtentorial herniation
4. superior cerebellar herniation
5. herniation of the cerebellar tonsils
(1, 2 - supratentorial herniation, 4, 5 - infratentorial herniation)
Coma with supratentorial mass formation
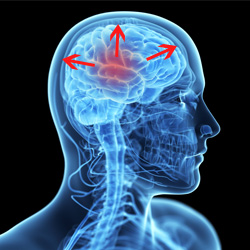
Central and temporal herniation cause different shapes rostral-caudal deterioration. Central herniation leads to sequential damage to the diencephalon, midbrain, pons, and medulla oblongata. “Classical” signs of increased ICP (increased blood pressure, bradycardia, changes in breathing patterns) are usually observed with lesions of the PCF, but may be absent in slowly developing supratentorial formations.
The distinction between central and temporal herniations is difficult to make when the disturbances reach the midbrain and lower regions. Determining the location of a lesion based on dislocation syndrome is unreliable.
Clinical signs to differentiate between temporal and central herniations
Disturbances in the level of consciousness are observed in early period with central herniation and late with temporal herniation
. temporal herniation rarely results in decortication rigidity
Differential diagnosis of the causes of supratentorial herniation
1. vascular: NMC, ICH, SAH
2. inflammatory: brain abscess, subdural empyema, herpetic encephalitis
4. traumatic: EDH, SDH, depressed skull fracture
Coma with infratentorial mass formation
NB: it is very important to identify patients with primary lesions ZCHYA, because they may require emergency surgery.
Differential diagnosis of the causes of infratentorial herniation
1. vascular: brainstem infarction (including OA occlusion), cerebellar infarction or hematoma
2. inflammatory: cerebellar abscess, central pontine myelinolysis, brainstem encephalitis
3. tumor: primary or mts
4. traumatic: EDH or SDH
Superior cerebellar herniation
Sometimes observed with volumetric formations PCF may be aggravated by ventriculostomy. The cerebellar vermis rises above the tentorium, compresses the midbrain, and can compress the PCA → infarction. May compress water supply → HCF.
Herniation of the cerebellar tonsils
The tonsils of the cerebellum are wedged into the cerebral cortex, compressing medulla→ stopping breathing. Death usually occurs quickly.
It is observed both with supra- and infratentorial space-occupying formations or with ICP. May be triggered by LP. In many cases there may simply be pressure on the brainstem without true herniation. There are cases of significant herniation of the tonsils into the thyroid gland while the patient remains conscious.
Greenberg. Neurosurgery

