Open penetrating blind head wound. Providing first aid for a gunshot wound
A wound that results in projectile fragments, bullets, and shot entering the human body is called a gunshot wound. Such injuries are classified as fatal, so the person must be immediately taken to medical institution.
First aid for gunshot wound rendered according to a general algorithm, regardless of the damaging object that caused it. However, there are minor differences in emergency actions depending on the location of the injury.
Calling medical workers
Medical assistance for gunshot wounds is the only way to save the victim’s life, so contacting a healthcare facility should be mandatory. However, before calling the emergency dispatcher, you need to determine the severity of the injury and general state victim. At heavy bleeding when observed big loss bleeding, it must be stopped immediately. To do this, for arterial bleeding, and for venous bleeding - pressure bandage. Once the danger of fatal bleeding has been averted, you can call ambulance.
In a conversation with the dispatcher, you need to point out the following facts:
- Type of injury;
- Type and presence of bleeding;
- Localization of the wound.
The type of injury is extremely important in determining the severity of the injury. Doctors divide bullet wounds into 2 types:
- Isolated (one cavity of the human body is damaged);
- Combined (2 or more cavities are injured).
Combined injuries are extremely life-threatening: death after them it reaches 80%.
Note!
If the dispatcher indicates that the ambulance will not be able to arrive at the scene within half an hour, then the victim must be transported independently! To do this, use personal transport or cars following a passing route.
After the issue of delivering the victim has been resolved, they begin to provide first aid for a bullet wound.
Head wounds
Gunshot wounds to the head are varied. They are made from pistols, shotguns, and self-propelled guns. No less dangerous are injuries caused by objects that are not classified as firearms: spearfishing devices, crossbows or pneumatic guns.
A characteristic feature of “modern” head wounds is the “point” location of multiple wounds (no more than 2-3 mm in diameter). Most often they are obtained as a result of being hit by a shot. If a shot is fired at the head from a long distance and the bullet hits scalp head, determine the injury when initial examination difficult. When shot at point-blank range or at close range, the wounds are deep and have a large volume.
Note!
The specificity of a bullet head injury is that its magnitude does not indicate the severity of the injury. A minimal wound opening may conceal deep brain damage. Whereas a tangent with deep damage to the skin and soft tissues will not be so dangerous.
In the case of a head wound, the victim’s condition is assessed based on 3 factors:
- Reaction of the eyes to irritation by sound and pain;
- Verbal answers to asked questions;
- Motor ability.
Wounds to the head area are often accompanied by... Its appearance is provoked by large external or internal blood loss. Therefore, the victim falls into an unconscious state and it is extremely difficult to bring him out of it.
Note!
If the victim has a decrease in the number of heart contractions, this indicates a developing intracranial hematoma. In this case, only emergency surgery can save a person.
In case of a gunshot wound to the head, it is important to try to bring the victim out of shock. For this purpose, analgesics that do not contain narcotic components are used. The use of non-steroidal anti-inflammatory drugs with an analgesic effect is also indicated.
Note!
Bone fragments or foreign objects that have entered the wound cannot be removed independently. This will provoke profuse bleeding. Until the ambulance arrives or the victim is taken to the hospital, you can only apply it to the wound. sterile bandage. When using a pressure bandage.
Considering that foreign objects (bullets, shrapnel) change their location while the patient is being moved to a medical facility, transportation is carried out with extreme caution. If there is no consciousness, the patient is placed on his side. If available in oral cavity vomit, blood and mucus, it must be cleaned before transportation.

Injuries to the chest, abdomen, limbs
Assess the general condition of a person using a survey. Ask him a simple question about his name or how old he is. After a gunshot wound to the chest, abdomen or limbs, a person is most often conscious.
What not to do before the ambulance arrives:
- If a person is unconscious, do not try to revive him;
- During rendering emergency care Do not offer the victim drink or food (it is permissible to wipe his lips with a cloth soaked in water);
- Remove bullets and other foreign objects from the wound;
- Reposition prolapsed internal organs;
- Do not attempt to clean dirt or dried blood from the wound.
Remember the correct position for an unconscious person: his head should be turned to the side. If the victim responds to questions, gently bend his knees.
Note!
When helping a person after a gunshot wound, try to move him as little as possible.
Stop bleeding
If there is bleeding, determine its type.
- Arterial bleeding. The blood is bright red and “comes out” of the body in a pulsating fountain. To stop the loss arterial blood, the vessel is pressed with a finger in the wound. To do this, insert your fingers directly into the bullet hole. If the blood continues to spurt out, slowly move them in the wound until you feel the damaged vessel. Then a tourniquet is applied if the wound is on a limb, or wound tamponade is performed on other parts of the body.
- . It is characterized by viscous dark blood that comes out of the wound without pulsation. To stop it you need to capture a part skin together with the damaged vessel and fix it in this state. If the wound is located above the heart, the vessel is clamped above the wound. In a situation where it is located below the heart, the vessel is clamped below the wound. If blood vessels are damaged on the extremities, apply a pressure bandage. If the chest cavity or abdomen is injured, tamponade is used.
- Capillary bleeding. Blood flows out in drops from damaged vessels. As a rule, its amount is insignificant. The loss of capillary blood can be stopped by applying a pressure bandage or squeezing the capillary with a finger. Before this, the skin around the wound must be treated with an antiseptic.
Note!
In case of a bullet wound to the soft tissues of the leg and arms, stopping the bleeding is necessary. If it is not possible to apply a tourniquet or pressure bandage, close the vessels with your fingers until medical personnel arrive.

Treatment of the wound and application of a bandage
After the bleeding has stopped, a pressure aseptic bandage is applied. Before this, it is necessary to disinfect the surface around the wound. It needs to be processed in the following sequence:
- A little antiseptic is poured onto the skin area near the wound;
- Gently wipe it with a bandage or cloth;
- The next area, located near the wound, is treated in the same way, but with a different bandage or cloth;
- With absence antiseptic use ordinary water.
- Then the cleansed skin is lubricated with iodine or brilliant green.
Note!
It is prohibited to pour antiseptics into the wound itself! It can be sprinkled with Streptocide powder.
The bandage is applied to all bullet holes on the body: incoming and outgoing. First, place a clean bandage or cloth on the wound, then cover it with cotton wool. For thoracic wounds (damage to the chest), the cotton wool is replaced with a bag or oilcloth. If they are absent, the material is generously lubricated with greasy cream, ointment or Vaseline. “Oiled” fabric is used instead of polyethylene.
The finished structure is tightly wrapped to the body using a bandage or other available dressing material (torn clothes, pieces of cloth, even tape).
For abdominal injuries, when internal organs have fallen out abdominal cavity, they are collected in plastic bag and carefully attach it to the body with a bandage. Before medical personnel arrive, they must be constantly watered with water.
After the bandage is applied, place a cold object on it. However, remember that you cannot use snow or icicles. Place the victim in the position that you think will be most comfortable for him. For chest injuries, be sure to bend the person’s knees, giving him a semi-sitting position.
Warm the patient by wrapping him in blankets. This action must be performed regardless of the time of year.
Note!
If the applied bandages become saturated with blood, do not remove them to apply new ones. It is enough to apply another layer of bandage on top of the existing bandage.
When it is possible to administer an antibiotic intramuscularly to the victim, which has a wide spectrum of action. If bullet wound was in the chest, leg or arm, you can give the victim an antibiotic in tablet form. Be sure to give analgesics that do not contain narcotic components.
Before doctors arrive or the victim is taken to a medical facility, you need to constantly talk to him. It is advisable to record vital signs all this time: and heart rate.

Tamponade
Correctly applying a tourniquet is extremely difficult for a beginner who is faced with a critical situation for the first time. Any inaccuracy in this case can cause necrosis (death) of tissue on the limb being pulled. Therefore, doctors recommend using tamponade as a way to stop bleeding on the extremities.
Let's consider how to correctly use this method of stopping blood loss.
- Prepare bandages or materials that replace them (fabric, clean clothes);
- Tear or cut them into strips, the width of which does not exceed 10 cm;
- Place the edge of the resulting tape into the wound, push it as deep as possible;
- Then, sequentially, collecting 2-3 cm of a new piece of tissue with your fingers, immerse it in the wound;
- This is done until the hole is completely closed with a “plug” of material.
Note!
Until the wound is completely covered with tissue, the vessel is closed with a finger.
Bullet wounds - dangerous injury, which leads to death due to . However, it is impossible to recognize and stop internal bleeding in first aid conditions. Therefore, such injury requires immediate hospitalization of the victim.
To provide first aid you need:
* Correctly assess the nature and severity of the injury.
* Knowing the nature of the injury, take the correct steps to provide first aid.
The bullet, penetrating the body, causes damage to the latter. These injuries have certain differences from other injuries to the body that should be taken into account when providing first aid.
First, the wounds are usually deep and the injuring object is often left inside the body.
Secondly, the wound is often contaminated with fragments of tissue, projectile and bone fragments.
These features of a gunshot wound should be taken into account when providing first aid to the victim.
The severity of the injury should be assessed by:
* the location and type of entrance, the behavior of the victim and other signs.
Wounds to the extremities
The first thing you should pay attention to when providing first aid for injured limbs is the presence of bleeding. If the arteries of the thigh or shoulder are destroyed, death from blood loss can occur within a second. So, if you are wounded in the arm (and the artery is damaged), death from blood loss can occur within 90 seconds, and loss of consciousness within 15 seconds. By the color of the blood we determine whether it is venous or arterial bleeding. Venous blood is dark, and arterial blood is scarlet and is knocked out of the wound intensively (a fountain of blood from the wound). Bleeding is stopped by applying a pressure bandage, tourniquet, or wound packing. When a tourniquet is applied, venous bleeding stops below the wound, and arterial bleeding stops above the wound. It is not recommended to apply a tourniquet for more than two hours. This time should be enough to deliver the victim to a medical facility. For venous bleeding, it is advisable to apply a pressure bandage rather than a tourniquet. A pressure bandage is applied to the wound. Wound tamponade for injuries of the extremities is rarely performed. To pack a wound, you can use a long, narrow object to tightly pack the wound with a sterile bandage. The higher the artery is affected, the faster blood loss occurs. The arteries of the limbs are projected onto the inner side of the thigh and shoulder (those areas where the skin is more difficult to tan).
As a result of excessive blood loss, hemorrhagic shock develops. The pain can be so severe that it causes painful shock.
ANTI-SHOCK MEASURES FOR BLOOD LOSS:
1. Immediate stop of bleeding.
2. Giving the victim a body position in which the limbs are slightly elevated.
3. Immediate replenishment of blood deficiency with blood-substituting solutions.
4. Antishock drugs, painkillers.
5. Providing warmth.
6. Call an ambulance.
The second thing to consider is possible bone fractures. In case of fractures, the limb must be immobilized. It is better not to try to move the limb at all, because... broken bones have sharp edges that can damage blood vessels, ligaments and muscles. The wound should be covered with a sterile bandage. Self-transportation of the victim is possible.
GUNSHOT WOUND OF THE HEAD
Does not always cause instant death. Approximately 15% of those injured survive. Wounds to the face are usually accompanied by an abundance of blood due to the large number of vessels located in the facial part of the skull. A head injury should be considered a concussion. The victim may lose consciousness due to the raush and show no signs of life, but the brain may not be damaged. If there is a gunshot wound to the head, the victim is laid horizontally and kept at rest. It is better not to touch the head wound (excluding facial wounds) (cover with a sterile napkin), and immediately call an ambulance. If breathing and heart stop, perform artificial respiration and cardiac massage. Facial wounds with copious discharge blood: clamp the wound with a sterile swab. Self-transportation is not recommended or must be carried out with all precautions.
GUNSHOT WOUND OF THE SPINE
With spinal injuries, a short-term loss of consciousness may occur. The victim is immobilized (layed down). If there is bleeding, apply a bandage. For head and spine injuries, first aid is limited to immobilizing the victim and stopping possible bleeding. In case of respiratory and cardiac arrest, indirect cardiac massage and artificial respiration are performed. Self-transportation is not recommended.
GUNSHOT WOUND OF THE NECK
The injury may be complicated by damage to the larynx and damage to the spine and carotid arteries. In the first case, the victim is immobilized, and in the second, the bleeding is immediately stopped. Death from blood loss when the carotid artery is injured can occur within 10-12 seconds. The artery is pinched with your fingers, and the wound is immediately tightly packed with a sterile bandage. Gentle transportation.
GUNSHOT WOUND IN THE CHEST AND ABDOMEN
All organs located in the human body are divided into three sections: pleural cavity, abdominal cavity and pelvic organs. The organs located in the pleural cavity are separated from the organs located in the abdominal cavity by the diaphragm, and the abdominal organs are separated from the pelvic organs by the peritoneum. When wounded internal organs, blood does not always pour out, but accumulates in these cavities. Therefore, it is not always easy to judge whether large arteries and veins are affected by such injuries. Stopping bleeding is difficult. Injuries to the organs of the pleural cavity may be complicated by internal bleeding, pneumothorax, hemothorax, or pneumohemothorax.
Pneumothorax is the entry of air through the wound opening into the pleural cavity. Occurs with knife and gunshot wounds to the chest, as well as with open fractures ribs The volume of the chest is limited. When air gets there, it interferes with breathing and heart function because... occupies the volume used by these organs.
Hemothorax is the entry of blood into the pleural cavity. Occurs with knife and gunshot wounds to the chest, as well as with open rib fractures. The volume of the chest is limited. When blood gets there, it interferes with breathing and heart function because... occupies the space used by these organizations. Pneumothorax is the entry of both blood and air into the pleural cavity.
To prevent air from entering the pleural cavity, it is necessary to apply an airtight bandage to the wound - a gauze pad coated with boron ointment or petroleum jelly, a piece of polyethylene, or, in extreme cases, tightly clamp the wound with the palm of your hand. The victim is placed in a semi-sitting position. Stopping bleeding is difficult. Transportation is gentle.
If there is a wound in the heart area, the worst is assumed. External signs such as rapid (instant) deterioration of the victim’s condition, sallow complexion, quick loss consciousness. It should be noted that death as a result of acute heart failure (when the heart is injured) does not always occur. Sometimes there is a gradual decline in the body’s activity as a result of the pericardium filling with blood and, as a result, difficulty in the functioning of the heart. Assistance in such cases should be provided by a specialist (pericardial drainage, suturing of a cardiac wound), who should be called immediately.
The pericardium is the cavity in which the heart is located. When the heart is injured, blood can enter this cavity and compress the heart, interfering with its normal functioning.
GUNSHOT WOUND OF THE ABDOMINAL CAVITY
For injuries to the abdominal organs, I place the victim in a semi-sitting position. Prevention of wound infection. In case of severe blood loss - antishock therapy.
Prevention of wound infection:
*disinfect the edges of the wound;
*apply a sterile napkin.
GUNSHOT WOUND OF THE PELVIC ORGANS
Injuries to the pelvic organs can be complicated by fractures of the pelvic bones, ruptures of arteries and veins, and nerve damage. Emergency care for wounds in the pelvic area - anti-shock measures and prevention of wound infection. When wounded in the gluteal region, profuse bleeding may occur, which is stopped by tight tamponade of the bullet entry hole. For fractures of the pelvic bones and hip joint the victim is immobilized. Gentle transportation. Self-transportation is not advisable.
USEFUL TIPS
When providing first aid, dressing material is always needed. When it is not at hand, you have to use a handkerchief, parts of clothing; but if you find a place to store the gun, then maybe a sterile bag will fit in your pocket. A first aid kit is required in the car. At home, it is advisable to have a first aid kit no worse than a car one. The most necessary thing for blood loss is blood replacement solutions, sold in pharmacies without a prescription along with an intravenous injection machine.
Do not forget that some advice can be obtained over the phone when calling an ambulance. It is better if by the time you call an ambulance you have correctly determined the injury and condition of the victim. Remember that there are often cases when the victim could not be saved due to the fact that, based on the message from those who called the ambulance, the operator sent a doctor of a different profile to the scene of the incident.
In some cases, self-delivery of the victim to the hospital is preferable (faster). City hospitals are on duty on a rotating basis. The address of the duty hospital can be found by calling the ambulance phone. The dispatcher can warn the emergency room of the hospital where you intend to deliver the wounded person about the nature of the injury so that the medical staff can prepare to receive the victim.
HOW TO REMOVE A BULLET
According to statistics, per one inhabitant of the planet there is one and a half Kalashnikov assault rifles, considering that there are 30 rounds in the clip, this is quite enough to fill you with lead like a mincemeat, so if you faint at the sight of blood and, if you pinch your finger, blow on it in the old fashioned way , as in childhood, it’s better to immediately forget about military field surgery.
However, if you are not a timid person, then here we will tell you how to remove a bullet after a gunshot wound (as an option, remove a shell fragment) and about the rules that an improvised operating room must comply with if you really find yourself in military field conditions, and there is no longer an infirmary, because it had just been bombed.
Immediately after injury
Do not rush to immediately pull out a foreign object from the body; a large one may be affected blood vessel and after removing the object, severe bleeding will occur.
Apply a tourniquet to arterial bleeding (blood bright color and flows like a fountain) above the wound site (the bandage is located between the wound and the heart), and when a vein is wounded, a tight compressive bandage is applied lower along the vessel (the wound is located between the bandage and the heart).
Do not forget that you should not stop the blood supply to the wounded limb for more than 2 hours, then give at least 15 minutes to restore normal blood flow, after which you can reapply the tourniquet (in case of dangerous arterial bleeding).
Provide warmth to the wounded person and place his body in a position in which his arms and legs are above body level.
If a gunshot or shrapnel wound is located in the chest area, there is a possibility of pneumohemothorax, which occurs if blood and air enter the pleural cavity located in the chest. This can be avoided by bandaging the wound with an airtight bandage (an ordinary napkin covered with a layer of Vaseline will also work),
a piece of polyethylene or, if nothing is at hand, simply clamp it with your palm.
You need to have time to tightly clamp the wound on the artery with your fingers and quickly pack it with a sterile bandage. And remember, for the first time you have 10 seconds at most.
Operating room rules
Only a certified surgeon can carry out successful operations in military field conditions, and in extreme situations, a person who is at least somewhat familiar with anatomy, so that when pulling out a bullet in passing, you do not immobilize a limb, accidentally cut a tendon, or hit an important vessel. Everyone else needs to focus on sterilizing instruments and ensuring maximum comfortable conditions surgeon and patient during the operation.
The most effective tools for carrying out an operation in military field conditions are a knife and tweezers.
Everything needs to be sterilized, including gauze bandages or a respirator from a surgeon, soak the metal in alcohol and keep it on fire, harden the steel, then put it back in alcohol until the operation itself. A sterile apron and thoroughly washed and soaked hands in alcohol, if you do not have sterile rubber gloves.
How to remove a bullet
Before removing the bullet, check to see if it has gone through. You need to remove the bullet (fragment) as soon as possible, otherwise it will begin to slowly poison the body due to metal oxidation products. The exception is such serious injuries when vital organs, the head or spinal cord, or there is a possibility that the wounded person may die from blood loss during the operation. This is again the case if help will come not soon and all the rules of the operating room in the conditions of military field surgery were observed.
If the wounded person is conscious, then it is necessary to give alcohol as an anesthesia and squeeze something between the teeth so that you do not harm yourself with your teeth and tongue. It is very difficult to pull out a bullet alone; blood will constantly pour into the wound, preventing you from properly seeing the situation. It would be best to take on your “team” an assistant who will suck out the interfering blood, for example with a pre-sterilized enema, not to mention the fact that the responsibility for carrying out such an operation can also be shared with him. Remember, it is the blood that fills the gunshot wound that will VERY hinder the removal of the bullet quickly.
The patient is breathing, the bullet was used as a souvenir, but it was just brought into the wound great amount microbes You can disinfect it with alcohol, or you can be more extreme - pour gunpowder into the wound and set it on fire. The method is also good because it stops bleeding, but most likely it will lead to suppuration, especially if the wound is deep.
Combat injuries to the skull and brain account for gunshot injuries(bullet, shrapnel wounds, MVR, blast injuries), non-gunshot injuries(open and closed mechanical injuries, non-gunshot wounds) and their various combinations.
The operation of craniotomy was known back in Ancient Egypt. Surgical treatment of traumatic brain injuries was performed by many famous surgeons of the past: J.L. Petit, D.J. Larrey, H.W. Cushing etc. However, military neurosurgery as a branch of military field surgery was formed only during the Great Patriotic War Patriotic War, when the system of specialized medical (including neurosurgical) care was first born and field surgical hospitals were created for those wounded in the head, neck and spine ( N.N. Burdenko, A.L. Polenov, I.S. Babchin, V.N. Shamov). The experience of treating combat trauma to the skull and brain in local wars and armed conflicts of recent decades has made it possible to supplement modern military neurosurgery with a number of new provisions and formulate the concept of early specialized neurosurgical care ( B.A. Samotokin, V.A. Khilko, B.V. Gaidar, V.E. Parfenov).
14.1 GUNSHOT INJURIES OF THE SKULL AND BRAIN
14.1.1. Terminology, classification
According to data from the period of the Great Patriotic War, gunshot injuries to the skull and brain accounted for 6-7% of all gunshot injuries; in the armed conflicts of recent decades in the North Caucasus, their frequency increased to 20%.
There are isolated, multiple and combined injuries (wounds) of the skull and brain. Isolated called a trauma (wound) in which there is one damage. Simultaneous damage to one or more MS of the skull and brain
called in several places multiple trauma (wound) of the skull and brain . Simultaneous damage to the skull and brain, as well as the organ of vision, ENT organs or maxillofacial area is called multiple head trauma (wound) . Simultaneous damage to the skull and brain with other anatomical areas of the body (neck, chest, abdomen, pelvis, spine, limbs) is called combined traumatic brain injury (wound) .
The basis for the classification of gunshot wounds of the skull and brain is their division into 3 large groups, proposed by N.N. Petrov in 1917: soft tissue injuries, constituting 50%; non-penetrating skull wounds, making up 20%; penetrating injuries of the skull and brain, accounting for 30% of all gunshot wounds of the skull and brain.
Soft tissue injuries of the skull characterized by damage to the skin, aponeurosis, muscles or periosteum. With gunshot wounds of soft tissues, there are no fractures of the skull bones, but the brain can be damaged in the form of a concussion, bruise and even compression (hematoma) due to the energy of the lateral impact of the MS.
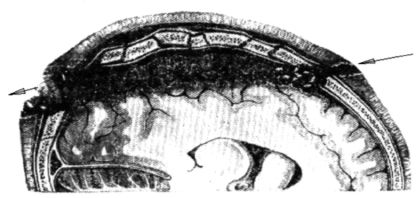
Non-penetrating skull wounds characterized by damage to soft tissues and bones while maintaining the integrity of the hard meninges. This type injuries are always accompanied by brain contusion, subarachnoid hemorrhage, and rarely by compression of the brain (bone fragments, epi- or subdural hematoma). Despite skull fractures and microbial contamination of the wound, the dura mater in most cases prevents the spread of infection to the brain tissue(Fig. 14.1).
Penetrating injuries to the skull and brain characterized by damage to the integument, bones, membranes and substance of the brain, characterized by severity and high mortality (up to 53%, according to the period of the Great Patriotic War, 30% in local wars). The severity of penetrating injuries is determined by the formations through which the MS passes (cortex, subcortex, ventricles of the brain, basal ganglia or brain stem) and the degree of their damage (Fig. 14.2).
Injuries to the stem and deep parts of the brain are particularly severe. With penetrating wounds, severe IOs most often develop - meningitis, meningoencephalitis and brain abscess, the frequency of development of which reached 70% during the Great Patriotic War and 30% in modern wars.
However, this information is not enough to make a complete diagnosis of a traumatic brain injury. For this purpose it is used nosological classification of gunshot wounds of the skull and brain(Table 14.1).
Rice. 14.1. Non-penetrating skull injury with bone fracture

Rice. 14.2. Tangent penetrating injury to the skull and brain
Table 14.1. Classification of gunshot wounds of the skull and brain

Gunshot wounds of the skull and brain are divided according to a number of characteristics. According to etiology there are bullet, shrapnel wounds and MVR - they differ in the volume and nature of the damage, because bullets have greater kinetic energy than fragments, and MVRs are distinguished by the combined nature of damage.
Penetrating injuries to the skull can be through and blind , and according to the location of the wound channel they are divided into tangent, segmental and diametrical (O.M. Kholbek, 1911).
The wound is called tangent(tangential), when a bullet or fragment passes superficially and damages the bone, dura mater and superficial parts of the brain (Fig. 14.2). It should be noted that in case of tangential wounds, despite the superficial location of the wound channel and the insignificant scale of destruction of the medulla formed along the course of the MS, the morphological and functional disorders often spread to neighboring areas of the brain. This is explained by the fact that the substance of the brain is a medium containing a large amount of fluid and is located in a closed space limited by the dense membranes and bones of the skull.
The wounds are called segmental, when MS passes through the cranial cavity along one of chords within one or two lobes of the brain, and the wound channel is located at some depth from the surface of the brain; at the same time, it has a fairly significant extent (Fig. 14.3).
Rice. 14.3. Segmental penetrating injury of the skull and brain
With all segmental wounds, small fragments of bone, hair, and sometimes pieces of headgear are carried into the depths of the wound channel. Destruction of the brain matter, as with any gunshot wound, is not limited to the area of passage of the projectile, but spreads to the sides and is expressed in the formation of hemorrhages and foci of contusion of brain tissue at a considerable distance from the wound canal.
At diametrical In wounds, the wound channel lies deeper than in segmental wounds, passing along the large chord (diameter) of the circumference of the skull (Fig. 14.4).
Diametrical wounds are the most severe, because the wound channel in these cases runs at great depth, damaging the ventricular system, the brainstem and other deep-lying vital formations. Therefore, diametrical wounds are accompanied by high mortality, and deaths occur early as a result of direct damage to vital centers of the brain.
A type of diametrical wounds are diagonal, in which the wound channel also runs along the diameter of the skull, but in a different plane, located closer to the sagittal. With these wounds, the entrance hole of the wound canal is usually located in facial areas, jaws, neck, and the output - on the convexital (convex) surface of the skull. This location of the wound channel is accompanied by primary damage to the brain stem and defines these injuries as fatal.

Rice. 14.4. Diametric penetrating wound of the skull and brain
Blind Skull wounds have one entrance hole and a wound channel of varying length, at the end of which lies a bullet or fragment. By analogy with through wounds, blind wounds are divided into simple, radial, segmental and diametrical (Fig. 14.5).
The severity of the blind wound is determined depth of the wound channel and its size. The most severe are blind wounds running along the base of the brain.
Among penetrating gunshot wounds of the skull, sometimes there are so-called ricocheting wounds (according to R. Payr, 1916), characterized by the fact that in the presence of one wound hole (entrance) in the depths of the wound channel, only bone fragments of the skull are found, and the RS is absent - it hit the convex

Rice. 14.5. Scheme of blind penetrating wounds of the skull and brain: 1 - simple; 2 - radial; 3 - segmental; 4 - diametrical
surface of the skull, causes damage and sharply changes the flight path (ricochets), moving away from the skull ( external rebound). At internal rebound The RS changes its trajectory upon contact with the concave surface of the skull on the opposite side from the entrance opening of the wound canal.
Since determining the severity of brain damage and diagnosing the life-threatening consequences of gunshot injuries to the skull and brain are based on identifying a number of clinical symptoms and syndromes, they are presented separately in section 14.1.3.
14.1.2. Clinic and diagnosis of gunshot wounds of the skull and brain
In field conditions at the advanced stages of medical evacuation (medical evacuation, first aid department, medical hospital), the opportunities and time for full neurological examination wounded with gunshot trauma to the skull and brain. Sorting of the wounded and making a diagnosis is carried out by military doctors and general surgeons. Therefore they objectives are: 1) identification of life-threatening consequences of injury for the timely provision of emergency medical care and 2) formulation of a diagnosis of injury according to the algorithm proposed in the textbook for making the correct triage decision.
At the advanced stages of medical evacuation, the diagnosis of gunshot trauma to the skull and brain is based on identifying general and local symptoms of gunshot trauma, symptoms of acute impairment of vital functions, general cerebral and focal symptoms brain damage.
The examination of any casualty at the triage area begins with an assessment of the severity of his condition and the active identification of acute impairment of vital functions. Symptoms not associated with brain damage are referred to in this chapter as general symptoms. Identifying and assessing them is important because 60% of injuries to the skull and brain are combined with injuries to other areas of the body: neck, chest, abdomen, pelvis, spine or extremities. Damage to the skull and brain is not always the leading one, and in some cases a severe craniocerebral injury is combined with severe damage to another area: often to the limbs, less often to the chest, abdomen, and pelvis. Therefore, when triaging the wounded, it is important not to randomly determine common symptoms, A targeted identification of four main syndromes .
It manifests itself bluishness of the skin and lips, restless behavior of the wounded, frequent and noisy breathing . The main reasons for the development of this syndrome are asphyxia or severe chest injuries with ARF.
It manifests itself pallor of the skin and lips, lethargy of the wounded, rapid and weak pulse, low SBP - less than 100 mm Hg. The main reason for the development of this syndrome is acute blood loss. Most often it is caused by severe concomitant injuries to the abdomen, chest or pelvis, and less commonly to the extremities.
Traumatic coma syndrome. It manifests itself lack of consciousness, speech contact, limb movements, motor response to pain. In deep coma, respiratory and circulatory disorders of central origin are possible (with the exception of chest damage and sources of bleeding). This syndrome is caused by severe brain damage.
Syndrome terminal state . It manifests itself gray (sallow) color of the skin and lips, pronounced lethargy of the wounded person up to stupor, frequent (heart rate more than 140 per minute) and weak pulse only in the carotid arteries, blood pressure is not determined, breathing is rare and fading. The causes of the terminal condition can be: extremely severe trauma of any location, but most often - severe MVR, severe injuries to several areas of the body, severe injuries to the abdomen or pelvis with acute massive blood loss, gunshot wounds of the skull with extremely severe brain damage.
After assessing general symptoms wounds and other injuries are examined- there may be several of them on the head and in other areas of the body. When examining a cranial wound, its location, depth, area, and the nature of the damaged tissue are determined, that is, the local symptoms. In this case, superficial gunshot wounds are easily identified, and in case of bleeding, its sources are clarified. Important information can be obtained when, upon examination of the wound, bone fragments of the skull, leakage of cerebrospinal fluid or destroyed brain matter (cerebral detritus) are visible - they indicate the penetrating nature of the wound (Fig. 14.6).
Deep wounds of the skull in a serious condition of the wounded should not be specially examined, because the harm from this may be greater than the benefit when, for example, bleeding or liquorrhea resumes when a blood clot is accidentally removed.

Rice. 14.6. The flow of cerebral detritus from the wound in a blind penetrating wound of the skull in the left temporal region
In general, of the local symptoms for making a triage decision, the following are most important: external bleeding and leakage of cerebrospinal fluid or cerebral detritus from the wound; the rest, if possible, clarify the diagnosis. That's why important rule The staged treatment of head wounds is as follows: at the advanced stages of medical evacuation, the bandage previously applied to the head wound, which lies well on it, is not removed to diagnose the wound. It is removed only in case of heavy contamination with earth, radioactive substances or HTV. If the bandage is intensively soaked with blood: in the medical unit (med) it is bandaged, in the medical hospital it is removed in the operating room, where the wounded person is taken to stop external bleeding.
The basis for the diagnosis and prognosis of gunshot TBI is the determination of the severity of brain damage and its life-threatening consequences.
Diagnosis of the severity of brain damage is based on active identification of the wounded person cerebral and focal symptoms, and symptoms of violation of vital functions.
General cerebral symptoms most characterize the severity of brain damage and are accessible to determination
at the advanced stages of medical evacuation. Indicates minimal brain damage loss of consciousness at the time of injury and amnesia to events preceding or after injury. Less informative symptoms of brain damage are headache, dizziness, tinnitus, nausea, vomiting, lethargy or motor agitation.
The most informative symptom of brain damage is impaired consciousness . Moreover, the more pronounced the degree of impairment of consciousness, the more severe the brain damage. Therefore, it is necessary to have a good knowledge of the degree of impairment of consciousness to make a diagnosis of gunshot TBI and make a triage decision. There are many subjective and objective methods and scales for impairment of consciousness (Glasgow coma scale, Shakhnovich scale, etc.), but for the advanced stages of medical evacuation, today the most convenient is the domestic descriptive methodology, distinguishing six degrees of impairment of consciousness.
1. Moderate stun- the wounded person is conscious, answers questions, but is inhibited or agitated, disoriented in space and time.
2. The stun is deep- the wounded is in a state of sleep, but with strong impact to him (shout, slaps on the cheeks) he answers questions in monosyllables and sluggishly.
3. Sopor- consciousness is absent, speech contact is impossible, tendon reflexes and motor reflexes are preserved defensive reactions for pain, opening eyes.
4. Coma moderate- consciousness is absent, speech contact is absent, tendon reflexes and motor protective reactions to pain are absent; Spontaneous breathing, swallowing, pupillary and corneal reflexes were preserved.
5. Coma deep- consciousness is absent, speech contact is absent, tendon reflexes and motor protective reactions to pain are absent; pupillary and corneal reflexes are absent, swallowing is impaired; hemodynamics are relatively stable, spontaneous breathing is ineffective, but rhythmic.
6. Coma beyond measure- to the symptoms of deep coma are added: instability of hemodynamics of central origin [decrease in sBP less than 90 mm Hg, tachycardia (heart rate more than 140 per 1 min), less often - bradycardia (heart rate less than 60 per 1 min)] and pathological respiratory rhythms, bilateral mydriasis
Focal symptoms to a lesser extent characterize the severity of brain damage. However they have great importance in the diagnosis of brain compression - a life-threatening consequence of a traumatic brain injury - and in determining the location of the injury. At the stages of providing first medical and qualified medical care, it is possible to identify only bright focal symptoms.
Anisocoria- is often a manifestation of a space-occupying process in the cranial cavity (intracranial hematoma, hydroma, local cerebral edema in the area of the brain wound) on the side of the dilated pupil.
Fixing the eyeballs and head to the side(right or left) often indicates a volumetric process in the cranial cavity on the side of fixation (“the patient’s fixed gaze shows the surgeon on which side to perform the trepanation”).
Crooked mouth; cheek, which takes the shape of a “sail” when breathing; smoothness of the nasolabial fold, non-closure of the eyelid are signs of damage to the facial nerve on the same side.
Local limb cramps it is often a manifestation of a space-occupying process in the cranial cavity on the opposite side.
Limb paralysis it indicates damage to the motor areas of the brain or a space-occupying process in the cranial cavity on the opposite side.
Symptoms such as: speech, hearing and vision impairments- especially on one ear, eye.
Symptoms of acute impairment of vital functions indicate either extremely severe brain damage, or the development of cerebral edema and its infringement in the foramen of the cerebellar tentorium or in the foramen magnum of the skull base (dislocation). Violation of vital functions occurs as a result of primary or secondary (due to infringement) damage to the brain stem, in which the nuclei of the vasomotor and respiratory centers are located. They manifest themselves as pronounced hemodynamic disorders: persistent arterial hypertension(SBP more than 150 mmHg) , or arterial hypotension(SBP less than 90 mmHg), tachycardia(heart rate more than 140 per minute) or bradycardia(heart rate less than 60 per minute). The most typical manifestation of violations of vital functions is breathing rhythm disorder requiring the use of mechanical ventilation.
14.1.3. Determining the severity of brain damage, diagnosing life-threatening consequences of gunshot injuries to the skull and brain
At the stages of providing first medical and qualified medical care, diagnosis of the severity of brain damage is carried out by military doctors and general surgeons, so it should be based on simple and accessible symptoms.
From this perspective, there are three degrees of severity of brain damage: light, heavy and extremely heavy. It should be clearly understood that this division of gunshot injuries to the skull and brain is used only at the advanced stages of medical evacuation (medical evacuation, first aid, medical hospital), where the sorting of the wounded is carried out without removing the bandages, without undressing and, naturally, without a full neurological examination. The main task of triaging the wounded at these stages of evacuation is not making an accurate diagnosis, but identifying 4 triage groups:
those in need of elimination of life-threatening consequences of injury, that is, emergency care measures;
subject to evacuation in 1st priority;
subject to evacuation in the 2nd stage;
agonizing.
Formulation of the final diagnosis and assessment of the severity of the traumatic brain injury is carried out only in a specialized neurosurgical hospital. Therefore, the criteria for assessing the severity of brain damage at the advanced stages of medical evacuation are: stability of the wounded person’s condition and absence of disturbances in vital functions for the triage period, and not the neurological deficit that will remain in the wounded person after final recovery.
Minor brain damage. In pathogenetic and morphological terms, mild injuries are characterized by damage only to superficial cortical structures on the convexital (convex) surface of the brain. Subcortical formations and trunk are intact. Mild brain injuries often occur with injuries to the soft tissues of the skull and with non-penetrating wounds of the skull, rarely with penetrating blind (superficial) and tangential wounds.
The main clinical criterion for non-severe brain damage is preserved consciousness: clear, moderate stupor or deep stupor. Focal symptoms in mild brain injuries may be absent, or they can be very vivid, for example, with a penetrating blind wound to the left temporal lobe(speech disorders, etc.), anterior central gyrus (motor disorders). There are no dysfunctions of vital organs. In prognostic terms, this is the most favorable group of wounded, therefore, in case of non-penetrating and especially penetrating wounds of the skull, they should be quickly taken to a specialized hospital before non-life-threatening complications develop.
Triage conclusion at the advanced stages of medical evacuation - evacuation in the 2nd stage to VPNhG.
Severe brain damage. In pathogenetic and morphological terms, severe injuries are characterized by damage to the cortical structures of the brain on its basal surface and subcortical formations. The brain stem can be involved in the pathological process during swelling and dislocation, that is, it can be pinched in the openings of the skull. Severe brain injuries are more common with penetrating blind (deep) and through segmental wounds.
The main criterion for severe brain damage is the absence of consciousness - its disturbances in the form of stupor and moderate coma. Focal symptoms in severe brain damage are poorly expressed, since they are masked by the absence reflex activity and pronounced general cerebral symptoms (extrapyramidal syndrome, diencephalic-catabolic syndrome). It usually manifests itself only as pupillary and oculomotor disturbances. Violations of vital functions manifest themselves only in the circulatory system: persistent arterial hypertension (blood pressure more than 150 mm Hg), tachycardia (heart rate more than 120 per minute). In prognostic terms, this group is characterized by high (about 50%) mortality, a high incidence of complications and long-term consequences. Most of the wounded with severe brain damage due to penetrating wounds of the skull do not return to duty.
Triage conclusion at the advanced stages of medical evacuation - evacuation to the 1st stage in VPNhG.
Extremely severe brain damage. In pathogenetic and morphological terms, extremely severe injuries are characterized by primary damage to the brain stem. As a rule, they occur with penetrating diametric and diagonal wounds.
The main criteria for extremely severe brain damage are: severe impairment of consciousness in the form of deep or extreme coma and impairment of vital functions. There are no focal symptoms due to deep coma, that is, complete absence reflex activity. Violations of vital functions are manifested by persistent hypotension (SBP less than 90 mm Hg), tachycardia (heart rate more than 140 per minute) or bradycardia (heart rate less than 60 per minute) and respiratory rhythm disturbances requiring mechanical ventilation. In terms of prognosis, wounded people with extremely severe brain damage have no prospects for survival, with mortality approaching 100%. Therefore, starting from the stage of providing qualified medical care, they belong to the triage category of “agoning”.
Life-threatening consequences of gunshot trauma to the skull and brain- pathological processes that develop immediately after injury due to damage to vital organs and tissues. A distinctive feature of life-threatening consequences is the inability of the body’s defense mechanisms to eliminate them independently. Consequently, in the absence of emergency medical care, the life-threatening consequences of injuries lead to death. Therefore, at all advanced stages of medical evacuation, emergency medical care is carried out not for wounds or injuries, but for their life-threatening consequences. Gunshot injuries to the skull and brain can result in three types of life-threatening consequences: external bleeding, compression of the brain and asphyxia.
External bleeding is a life-threatening consequence of a gunshot injury to the skull and brain in cases where it does not stop on its own or under a conventional aseptic dressing. The frequency of its occurrence, according to recent armed conflicts, is low and amounts to 4%. Sources of severe external bleeding are:
Arterial vessels of the integumentary tissues of the skull and the main one - a. temporalis superficialis with its branches;
Arteries of the dura mater, primarily branches a. menin-gea media; sinuses of the dura mater;
Cerebral vessels located in a brain wound. Brain compression- a pathological process that lasts from several hours to several days and often leads to death if it is not eliminated. Most often, compression of the brain in gunshot wounds is caused by intracranial hematomas (Fig. 14.7., 14.8.), less often by local cerebral edema in the wound area or a depressed fracture of the skull bones (Fig. 14.9.).
With gunshot craniocerebral wounds, compression of the brain is relatively rare - in 3% of cases.
For a long time, there were incorrect opinions about the mechanism of development of intracranial hematomas, which affected therapeutic tactics. It was believed that an intracranial hematoma is formed by a pumping mechanism, increasing with each portion of blood and compressing the brain after the volume of the hematoma exceeds the size of the reserve intrathecal spaces: 80 ml for epidural

Rice. 14.7. Compression of the brain by an epidural hematoma in the right fronto-parietal-temporal region (computer tomogram)

Rice. 14.8. Subdural hematoma in the left temporal region (intraoperative photograph)

Rice. 14.9. Depressed by a fracture of the left parietal region (intraoperative photograph)
and 180 ml - for the subdural space. In accordance with this, unfounded calls for immediate trephination at any stage of treatment and simplified ideas about the technique of eliminating compression were practiced: craniotomy - removal of the hematoma - ligation of the bleeding vessel - recovery. In practice, such situations turned out to be rare with non-gunshot TBI; with gunshot wounds they never occur.
Special studies by employees of the Leningrad Research Institute of Neurosurgery named after. A.L. Polenov under the leadership of Yu.V. Zotov showed that the main volume of intracranial hematoma is formed during the first 3-6 hours, at the same time a blood clot is formed, which subsequently interacts with the damaged area of the brain, causing its local edema, a decrease in the reserve intrathecal space and - cerebral compression syndrome. The smaller the volume of brain damage and the greater the reserve volume of the subthecal space (for example, with hematomas formed as a result of damage to the meningeal vessels by fragments of the skull bones), the slower the compression of the brain is formed: from 1 day to 2 or more weeks. In case of gunshot wounds, when the brain damage is extensive, the main role in the formation of brain compression belongs not so much to the hematoma as to the reactions of the damaged brain.
Classic neurological picture of compression of the head

Rice. 14.10. Typical hemilateral syndrome due to compression of the brain (Yu.V. Zotov, V.V. Shchedrenok)
brain in the form of pupil dilation on the compression side and central hemiplegia on the opposite side is described in many textbooks - and it should always be remembered when examining a wounded person with a craniocerebral injury (Fig. 14.10).
In conditions of staged treatment, when triaging head wounds, it is necessary to actively identify all the most informative symptoms of brain compression.
"Lucid interval"- the length of time between loss of consciousness at the time of TBI (injury) and repeated loss of consciousness at the time of examination; During this period of time, the wounded person is conscious (usually this is clarified with those accompanying him). This symptom is characteristic of mild brain damage, against the background of which compression develops. With severe brain damage, disorders of consciousness progress, often from stupor to coma. The diagnostic reliability of this symptom is very high.
Fixation of the head and gaze in the direction of compression of the brain. A very reliable, but not often encountered symptom of brain compression. It is determined when examining a wounded person at the triage area, when the doctor places the wounded person’s head in the middle position, and the wounded person reflexively turns it with effort to its previous position. Similar to the position of the head, the eyeballs are also fixed.
Local limb cramps on the side opposite to the compression of the brain, are also easily identified at the triage site. It is impossible not to notice them, since they are uncontrollable - you have to administer anticonvulsants (which, by the way, is ineffective). The diagnostic value of the symptom increases significantly if the arm or leg of the same name is affected by convulsions (hemilateral convulsive syndrome).
Anisocoria - a symptom that is easily determined by a careful examination of the wounded, but its diagnostic value in relation to compression of the brain and, especially, aspects of the pathological process is relatively small and amounts to 60%.
Bradycardia - Heart rate below 60 per minute. An important symptom indicating the likelihood of compression of the brain, but its specificity is low - it is also a manifestation of damage to the brain stem and a number of extracranial injuries (cardiac contusion, adrenal contusion). Its diagnostic value increases significantly when it is combined with one of the above symptoms. Important
remember that with combined craniocerebral injuries (traumas) accompanied by acute blood loss, for example, with simultaneous injuries to the abdomen or pelvis, a heart rate below 100 per minute should be regarded as relative bradycardia.
Hemiplegia, monoplegia, less often - paresis of the limbs on the side opposite to the compression of the brain, are important but nonspecific symptoms of cerebral compression because they are often neurological manifestation gunshot wound. At the sorting site, where special neurological techniques are not used, only gross motor disorders in the form of lack of limb movements are detected. This increases their diagnostic value, especially in combination with other symptoms.
The diagnostic significance of the listed symptoms for identifying compression of the brain increases significantly when they are combined: the more symptoms there are, the greater the likelihood of compression of the brain.
Asphyxia- acutely developing respiratory distress (suffocation) as a result of obstruction of the upper respiratory tract - with gunshot injuries of the skull and brain it is rare - up to 1% of cases. More often, asphyxia occurs with multiple head injuries, when injuries to the skull are combined with injuries to the face and jaws. In these cases, the cause of asphyxia is the flow of blood from the wounds of the maxillofacial area into the oropharynx and larynx against the background of impaired innervation of the epiglottis or a decrease in the cough-left reflex. In severe isolated craniocerebral injuries, the aspiration mechanism of asphyxia is realized due to the entry of vomit into the respiratory tract. With extremely severe injuries to the skull and brain, dislocation asphyxia develops as a result of retraction of the tongue: as a result of damage to the trunk, the activity of the glossopharyngeal and hypoglossal nerves is disrupted, the tongue loses muscle tone and sinks into the oropharynx, blocking the airways.
All life-threatening consequences of injuries must be actively identified. The wounded with external bleeding and asphyxia should be provided with emergency care at all stages of medical evacuation, and the wounded with compression of the brain should be urgently evacuated (by helicopter) to a specialized neurosurgical hospital - only there they can be provided with full emergency care.
Examples of diagnoses of gunshot wounds of the skull:
1. Multiple fragmentation blind wound soft tissue right half heads.
2. Bullet Tangent non-penetrating wound skull in the left parietal-temporal region with mild brain damage, with an incomplete fracture of the right parietal bone.
3. Shrapnel blind penetrating wound of the skull in the right parietal region with severe brain damage, with a perforated fracture of the parietal bone. Traumatic coma(Fig. 14.11 color illustration)).
4. Bullet through segmental penetrating wound of the skull in the left frontotemporal region with severe brain damage, with comminuted fractures of the frontal and temporal bones. Compression of the brain. Traumatic coma.
5. Bullet through-diametric bihemispheric penetrating wound of the skull in the temporal regions with extremely severe brain damage, with splintered fractures of the temporal bones. Continued external bleeding. Terminal state.
6. Severe mine blast wound. Combined mechanothermal combined trauma of the head, chest, extremities.
Plural gunshot injury heads. Shrapnel blind penetrating left-sided fronto-orbital wound of the skull with severe brain damage, multiple fractures of the orbital walls and destruction of the left eyeball.
Closed chest injury with multiple rib fractures on the right and lung damage. Right-sided tension pneumothorax.
Separation of the left tibia at the level middle third with extensive destruction of soft tissue and skin detachment up to the lower third of the thigh. Continued external bleeding.
Flame burn of lower extremities
Acute massive blood loss. Terminal state.
14.2. NON-GUNSHOT SKULL INJURIES
AND BRAIN
14.2.1. Terminology and classification
Based on etiology, non-gunshot injuries to the skull and brain are divided into mechanical (closed and open) TBI and non-gunshot wounds. In combat conditions, mechanical TBIs occur
quite often, accounting for 10-15% of the total combat pathology of this localization.
TO closed TBI These include injuries to the skull and brain in which the integrity of the skin as a natural biological barrier is preserved. TBIs with skin damage are open ; They may be non-penetrating And penetrating depending on the integrity of the dura mater . Fractures of the base of the skull with external oto or nasolorrhea are considered as an open penetrating TBI, since at the base of the skull the dura mater is tightly fused with the bone and during fractures is necessarily damaged along with it.
Non-gunshot wounds of the skull and brain (stab wounds, stab wounds, dowel wounds from a construction pistol, etc.) are rare in combat conditions and do not amount to big problem and are described in neurotraumatology manuals.
As with gunshot trauma to the skull and brain, with non-gunshot TBI there are combinations of injuries various departments head and anatomical areas of the body. The combination of brain damage with damage to the eyes, ENT organs, face and jaws refers to multiple head injuries, and the combination of TBI with damage to other areas of the body - to combined TBI.
In 1773, a French surgeon J.L. Petit proposed to distinguish 3 types of TBI: concussion, bruise and compression of the brain. In most textbooks, this division of TBI with varying degrees of detail for each type has been preserved to this day. One circumstance was unclear: why can compression develop with any type and severity of brain damage? The answer to this question was found by military field surgeons when in the 1990s. New principles for the classification of combat injuries were formed, an objective assessment of the severity of injuries and a new methodology for formulating a diagnosis were introduced in the system of staged treatment of the wounded.
From this point of view, compression of the brain does not characterize the type or severity of TBI (injury), but is its life-threatening consequence. Compression of the brain develops when damage enters the morphological substrate large vessels, liquor ducts, large bone fragments of the skull.
Thus, the basis classification of non-gunshot TBI They are divided into the following types:
Brain concussion;
Mild brain contusion;
Moderate brain contusion;
Severe brain contusion.
This classification reflects not only the type, but also the severity of TBI, both clinically and morphological manifestations. In this case, the severity of TBI increases from the surface of the brain in depth: from a concussion (functional impairment at the cortical level, clear consciousness) to a severe injury (damage to the brain stem, deep or extreme coma).
To correctly formulate the diagnosis of non-gunshot trauma to the skull and brain, it is used nosological classification(Table 14.2.)
As can be seen from the classification, one of the sections in formulating a diagnosis is the condition of the intrathecal spaces. It should be borne in mind that their importance increases in later periods traumatic illness, in progress specialized treatment. They are not detected at the advanced stages of medical evacuation. It is important to know that epidural and subdural hemorrhages are diagnosed only in peacetime with CT or MRI or when forensic autopsy. They are fundamentally different from epidural and subdural hematomas in their small volume, cape-like flat nature and, most importantly, in that they do not cause compression of the brain.
Calvarial fractures may also not be detected during the advanced stages of medical evacuation - and this is not strictly necessary. Fractures of the bones of the base of the skull are identified by indirect signs. “Symptom of glasses” (periorbital hematomas) or nasal liquorrhea (leakage of cerebrospinal fluid from the nose) indicate fractures of the bones of the base of the skull in the anterior cranial fossa. Symptoms of damage to the facial (distortion of the mouth, parousitis of the cheek, eyelid does not close, lacrimation or dry eye) or auditory (unpleasant tinnitus) nerves are signs of a pyramidal fracture temporal bone.
The life-threatening consequences of non-gunshot injuries to the skull and brain are manifested by the same symptoms as with a gunshot injury.
Table 14.2. Classification of non-gunshot injuries of the skull and brain

Examples of diagnoses of non-gunshot TBI:
1. Open traumatic brain injury. Brain concussion. Lacerated and bruised wound of the right parietotemporal region.
2. Closed craniocerebral injury. Mild brain contusion. Subarachnoid hemorrhage.
3. Open penetrating traumatic brain injury. Moderate brain contusion. Subarachnoid hemorrhage. Fracture of the left temporal bone with transition to the base of the skull. Lacerated and bruised wound of the left temporal region. Left-sided otohematoliquorrhea.
4. Open traumatic brain injury. Severe brain contusion. Subarachnoid hemorrhage. Fracture frontal bone on right. Lacerated and bruised wound of the frontal region on the right. Traumatic coma.
5. Closed craniocerebral injury. Severe brain contusion. Subarachnoid hemorrhage. Fracture of the bones of the cranial vault. Brain compression intracranial hematoma in the left fronto-parietal-temporal region. Traumatic coma.
6. Severe combined trauma of the head, abdomen, and limbs. Open penetrating traumatic brain injury. Severe brain contusion. Intraventricular hemorrhage. Fractures of the bones of the vault and base of the skull.
Closed abdominal injury with damage to internal organs. Continuing intra-abdominal bleeding.
Closed multiple limb injury. Closed fracture of the right femur in the middle third. Closed fracture of both bones of the left leg in the lower third.
Acute massive blood loss. Traumatic coma.
14.2.2. Clinic and diagnosis of non-gunshot traumatic brain injury
In field conditions, opportunities and time for a full examination of wounded people with non-gunshot injuries to the skull and brain are extremely limited. That's why you should remember the main symptoms of TBI and focus on them in the process of medical triage of the wounded. Usually wounded with non-severe TBI move independently around the units of the triage and evacuation department, complain of headache, tinnitus, disorientation - they need to be laid down, calmed down, examined, carried out medical care measures and sent on a stretcher to the evacuation room
tent. Wounded from severe TBI are delivered on a stretcher, often unconscious, which creates significant difficulties in diagnosis.
Examination of a wounded person with non-gunshot TBI begins with active identification (see section 14.1.2.) 4 main syndromes of acute impairment of vital functions. Based on their presence and severity, an assessment of the general condition of the wounded is formed. Like gunshot wounds, non-gunshot TBI in 60% of cases is combined with damage to other areas of the body.
Syndrome acute disorders breathing indicates asphyxia (often as a result of aspiration of vomit, cerebrospinal fluid, less often - dislocation of the tongue) or severe concomitant damage to the chest.
Acute circulatory disorder syndrome(as traumatic shock) develops with acute massive blood loss as a result of collateral damage abdomen, pelvis, limbs.
Traumatic coma syndrome clearly indicates severe brain damage, and terminal illness syndrome- about extremely severe brain damage or severe combined injury.
For closed non-gunshot TBI local symptoms poorly expressed. More often than others, subcutaneous hematomas of the scalp, periorbital hematomas are detected, and less often - liquorrhea from the nose and ears. Since the cerebrospinal fluid flowing from the ears and nose is often mixed with blood, they use "double spot" symptom. Liquor with blood spilled onto a white sheet or towel forms a double-circuit round spot: inner part- pink, outer - white, yellow. In case of open non-gunshot TBI, local symptoms are also the location, nature and depth of the wound in the integumentary tissues of the skull.
General cerebral and focal symptoms brain damage in non-gunshot TBI is of primary importance in determining the severity of brain damage, and identification syndrome acute disorders vital functions central origin - important prognostic value. They allow the triage physician to make the correct triage decision. The characteristics of these symptoms and identification methods are similar to those used when examining wounded people with gunshot trauma to the skull and brain (see section 14.1.2).
From the nosological classification of non-gunshot TBI it is clear that for diagnosis separate forms TBI (such as brain contusion
mild and moderate severity) the condition of the intrathecal liquor spaces, the presence and nature of fractures of the skull bones are of great importance. To identify the first, it is necessary to perform a lumbar puncture, which is a general medical procedure and can easily be performed by a surgeon or anesthesiologist at the stage of providing CCP. In this case, the cerebrospinal fluid pressure is determined (normally it is 80-180 mm water column for a lying position) and the presence of blood in the cerebrospinal fluid - subarachnoid hemorrhage. Diagnosis of skull fractures is also possible in the medical hospital by performing radiography of the skull in frontal and lateral projections.
At the same time, determining the state of the cerebrospinal fluid spaces and x-ray detection of skull fractures are not of fundamental importance for making a triage decision. Besides lumbar puncture itself may be accompanied by the development of brain dislocation (the wedging of the brain stem into the foramen magnum of the skull): due to the jet release of cerebrospinal fluid from the needle, a sharp decrease in cerebrospinal fluid pressure in the basal cistern, a sudden stop in breathing occurs on the dressing table and death. The rule to remember is: Lumbar puncture is contraindicated at the slightest suspicion of cerebral compression!
Non-severe TBI. In pathogenetic and morphological terms, they are characterized either only by functional disorders of the central nervous system, or by damage to the vessels of the arachnoid membrane, or by foci of hemorrhage and destruction of the cortical structures of the brain. Subcortical formations and trunk are intact.
The main clinical criterion for non-severe TBI is preserved consciousness: clear, moderate stupor, deep stun. From this point of view, the group of non-severe TBI includes: concussion, bruises of mild and moderate severity.
Brain concussion- most light form TBI, in which morphological changes are absent in the brain and its membranes, and pathogenetic and clinical manifestations are caused by functional changes in the central nervous system. The main clinical symptoms are: short-term (several minutes) loss of consciousness at the time of injury and retrograde amnesia. Such wounded people usually move independently (consciousness is clear), but complain of headache, nausea, dizziness, and sometimes vomiting. They belong to the category of lightly wounded and are evacuated in the 2nd turn by any transport to the VPGLR, where there is
a specialized neurological department for the treatment of this category of wounded.
Mild brain contusion- this is also a mild form of TBI, in which, unlike a concussion, there are not only functional changes CNS, but also morphological in the form of damage to the vessels of the arachnoid membrane. The latter are detected during lumbar puncture in the form of blood in the cerebrospinal fluid - subarachnoid hemorrhage. Basically, the clinical manifestations are the same as for a concussion, but the following are found: moderate stupor in terms of level of consciousness, headache and nausea are more pronounced, and vomiting occurs more often. In conditions of staged treatment Lumbar puncture is not performed for differential diagnosis, therefore, in practice, these wounded are also classified as lightly wounded and are sent to the VPGLR.
Moderate brain contusion eat. This form of brain injury lives up to its name - it occupies an intermediate position between mild and severe forms of TBI. However, since there is no “moderately severe” triage group in military field surgery, wounded people with moderate brain contusions belong to the “non-severe TBI” triage group. This is both prognostic and theoretically justified: there are no deaths, complications are rare, the treatment period does not exceed 60 days, and treatment is usually conservative. At the same time, with this form of TBI, Fractures of both the vault and base of the skull, and the morphological substrate of the injury is small foci of contusion (hemorrhage, subpial destruction), located only in the cortical structures of the brain. Therefore, the second (after skull fractures) pathognomonic symptom of moderate brain contusions is focal symptoms brain damage. Most often, in the conditions of staged treatment, oculomotor disorders (paresis of the oculomotor, abducens cranial nerves), innervation disorders (paresis, paralysis) of the facial or auditory nerves, speech and vision disorders, and paresis of the limbs are less common. These wounded are delivered, as a rule, on a stretcher, the state of consciousness is stunned (moderate or deep), vital functions are within normal limits, stable. The wounded with moderate brain contusions are also evacuated in the second place by any transport, but not to the VPGLR, but to the VPNH or to the VPNhG, since focal symptoms may still be a sign of slowly developing compression of the brain.
Severe TBI. In pathogenetic and morphological terms, they are characterized not only by damage to the cortical structures of the brain, but also to subcortical formations and the upper parts of the brain stem.
The main clinical criterion for severe TBI is the absence of consciousness - there are disturbances of consciousness in the form of stupor and moderate coma.
Since damage to these structures has a characteristic clinical picture, extrapyramidal and diencephalic forms of severe brain contusion are distinguished according to the level of damage.
Extrapyramidal form of severe brain contusion. As a result of damage to the subcortical formations in this form of severe contusion, the clinical picture is clearly dominated by hypokinetic rigid or hyperkinetic syndrome. The first syndrome is manifested by waxy rigidity of all muscle groups of the wounded person, a mask-like face with an absence of facial expressions, the second, on the contrary, by constant athetoid (worm-like) movements of the limbs (especially the upper ones). Consciousness - stupor, focal symptoms - not expressed (rarely - anisocoria, oculomotor disorders), vital functions are stable. The prognosis for life is favorable (mortality rate less than 20%), the social prognosis is often favorable.
Diencephalic form of severe brain contusion. With this form of severe contusion as a result of damage to the interstitial brain, where the main autonomic centers are located, the clinical picture appears bright diencephalic-catabolic syndrome. It is characterized by : arterial hypertension, tachycardia, muscle hypertension, hyperthermia, tachypnea. Consciousness - moderate coma. The pupils are usually evenly constricted, the eyeballs are fixed in the center. Focal symptoms are practically absent. Vital functions are at the level of subcompensation (see Appendix 1, scales “VPH-SP”, “VPH-SG”), that is, their stability is relative, sometimes correction is required during evacuation in the form of mechanical ventilation. The prognosis for life is relatively favorable, because mortality reaches 50%; the social prognosis is often unfavorable, since most wounded people become disabled after receiving a severe TBI.
The wounded with severe TBI, despite the relative stability of vital functions, do not delay at the stages of providing qualified assistance for intensive corrective therapy. After normalization of external respiration either by installing an air duct or tracheal intubation with mechanical ventilation, they are urgently evacuated to the VPNhG in the 1st place.
Extremely severe TBI. In pathogenetic and morphological terms, they are characterized by damage to the brain stem. The main clinical criterion for extremely severe TBI is the absence of consciousness - its disturbance in the form of a deep or extreme coma. Damage to the brain stem has a characteristic clinical picture in the form of mesencephalobulbar syndrome. Therefore, such forms of TBI are called mesencephalobulbar form of severe brain contusion. First of all, this form is manifested by pronounced disturbances of vital functions: persistent arterial hypotension refractory to infusion therapy, uncontrolled tachycardia (bradycardia) and arrhythmia, severe tachycardia or bradypnea or pathological breathing rhythms requiring mechanical ventilation. The eyeballs are fixed in the center, the pupils are wide, there is no reaction to light. It should be remembered that with extremely severe TBI
absolutely unfavorable prognostic signs are paralytic bilateral mydriasis and Magendie's symptom (unequal position of the eyeballs relative to the horizontal axis: one is higher, the other is lower). Without intensive correction of vital functions, death occurs within a few hours. Even in specialized centers, the mortality rate for this type of TBI is close to 100%. Therefore, the wounded with extremely severe TBI at the advanced stages of medical evacuation are classified as dying.
Life-threatening consequences with non-gunshot TBIs develop in 5-8% of cases. External bleeding from the sinuses of the dura mater with multiple open fractures of the bones of the calvarium is relatively rare - up to 0.5% and asphyxia (aspiration of cerebrospinal fluid, blood, vomit, dislocation of the tongue) - up to 1.5%. In other cases, the life-threatening consequences of TBI are represented by compression of the brain by intracranial (meningeal, intracerebral) hematomas, hydromas, and depressed fractures of the calvarial bones. The clinical picture and symptoms of life-threatening consequences in non-gunshot TBI are similar to those in gunshot injuries.
14.3. ASSISTANCE AT THE STAGES OF MEDICAL EVACUATION
The main principle of staged treatment of head wounded people is the fastest possible delivery to the VPNhG, bypassing even the stage of providing qualified surgical care.
First aid. Apply to the head wound aseptic dressing. To prevent aspiration of blood and vomit during vomiting and nosebleeds, the upper respiratory tract is cleaned. If the tongue is retracted, the orderly opens the wounded man's mouth with a mouth dilator, the tongue is removed using a tongue holder, the oral cavity and pharynx are cleaned of vomit from the mouth and pharynx with a napkin, and an air duct (breathing tube TD-10) is inserted. The wounded, who are unconscious, are carried out in a position on their side or stomach (a folded overcoat, duffel bag, etc. is placed under the chest).
In case of severe wounds to the head, promedol from a syringe tube is not administered due to the threat of respiratory depression.
First aid carried out by a paramedic who monitors the correctness of previously carried out measures and corrects their shortcomings. Elimination of asphyxia is carried out using the same methods as when providing first aid. If breathing is impaired, mechanical ventilation is performed using a manual breathing apparatus and oxygen inhalation. If the bandage gets wet with blood, it is bandaged tightly.
First medical aid. During armed conflict first medical aid is provided as pre-evacuation preparation for aeromedical evacuation of wounded with severe and extremely severe injuries - directly to the 1st echelon MVG to provide early specialized surgical care.
IN large scale war Those wounded in the head after first medical aid are evacuated to the medical hospital (omedo).
During medical triage There are 4 groups of wounded with gunshot or non-gunshot injuries to the skull and brain.
1. Those in need of emergency first aid measures in the dressing room - wounded with ongoing external bleeding from head wounds and wounded with asphyxia.
2. The wounded, for whom first medical aid can be provided at the triage area with subsequent evacuation to the 1st stage, - wounded with signs of brain compression and wounded with severe brain damage.
3. The wounded, for whom first medical aid can be provided at the sorting site with subsequent evacuation to the 2nd stage, - wounded with mild brain damage.
4. Agonizing- wounded with extremely severe brain damage - are sent to a triage tent in a specially equipped place (fenced off with sheets from the rest of the wounded). It should be remembered that the group of those in agony at the stage of providing first medical aid is identified only when there is a massive influx of wounded. IN normal conditions any casualty with detectable blood pressure should be evacuated .
In the dressing room, the upper respiratory tract is cleared for unconscious wounded people. An air duct is inserted to prevent tongue retraction. In case of ineffective spontaneous breathing, the anesthesiologist-resuscitator performs tracheal intubation and mechanical ventilation. If it is impossible to intubate the trachea, a conicotomy or tracheostomy is performed.
When the bandage becomes heavily saturated with blood, it becomes tightly bandaged. Continuing bleeding from the soft tissue arteries visible in the wound is stopped by ligating them or applying a pressure bandage with the introduction of napkins moistened with a 3% solution of hydrogen peroxide into the wound.
The rest of those wounded in the head receive assistance in the triage and evacuation department. They are given antibiotics and tetanus toxoid, cardiovascular drugs are used according to indications. Narcotic analgesics are not administered for penetrating craniocerebral injuries, because they depress the respiratory center. A full bladder in wounded patients with impaired consciousness is emptied with a catheter.
After first medical aid is provided, the wounded are sent to the evacuation room, from where they are evacuated in accordance with the triage conclusion. We should strive to evacuate those wounded in the head by helicopter immediately to the VPNhG.
Qualified medical care. The basic principle of providing CCP to the wounded with severe wounds and head injuries is do not delay them at this stage of evacuation .
In progress medical triage There are 5 groups of wounded with gunshot and non-gunshot injuries to the skull and brain.
1. Those in need of urgent qualified surgical care: wounded with asphyxia are sent to the dressing room for the seriously wounded, where a special dentist’s table is deployed for them; wounded with intense external bleeding are sent to the operating room. After assistance is provided, evacuation to VPNhG is the first priority.
2. Stretch wounded with lack of consciousness, but stable vital functions ( with severe brain damage, cerebral compression) - need preparation for evacuation in a ward intensive care, less often - evacuation ( only restoration and maintenance of breathing, up to intubation and mechanical ventilation ), after which evacuation is carried out to VPNhG in the 1st place.
3. Stretch wounded with preserved consciousness ( with mild brain damage) - are sent to evacuation tents for evacuation to VPNhG in the 2nd turn.
4. Walking head wounded- are sent to the triage tent for the lightly wounded, where they prepare for evacuation to the VPGLR in the 2nd line.
5. Agonizing- wounded with extremely severe brain damage with fading vital functions and signs of fatal injury (diagonal, diametrical with the outflow of cerebral detritus) - sent to the ward symptomatic therapy, allocated specifically in the hospital department.
The wounded are sent to the operating room with ongoing external bleeding, which cannot be stopped by tightly bandaging the bandage. Surgical interventions performed for ongoing external bleeding should include only measures to stop the bleeding. When hemostasis is achieved, the surgical intervention should be stopped, the wound covered with a bandage, and the wounded person sent to the VPNhG, where a specialist will perform exhaustive surgical treatment of the cranial wound.
Surgery for ongoing external bleeding carried out under general anesthesia and can consist of 3 elements: stopping bleeding from a soft tissue wound; trephination
bones in the area of the fracture (if bleeding continues from under the bone); stopping bleeding from the dura mater, sinuses and (or) brain wounds.
The first stage of the operation is dissection of the soft tissue wound. In this case, bleeding from soft tissues is stopped by diathermocoagulation or ligation and suturing of the bleeding vessel. Then the bone wound is examined, and if bleeding continues from under the bone, the bone wound is expanded with bone forceps-nippers (Fig. 14.12.).
The dimensions of the burr hole can vary, but most often - up to the border of the intact dura mater. Bleeding from the vessels of the dura mater is stopped by diathermocoagulation or suturing.
The following methods are used to stop bleeding from the dural sinus. During complete or almost complete breaks, sinus ligation. It can be done

Rice. 14.12. Expansion of bone wound
be only if the bone defect is of sufficient size by making incisions in the dura mater on the sides of the sinus, after which a silk thread is passed around the sinus with a round needle and tied (Fig. 14.13, 14.14).
It is impossible to ligate the sinus behind the Rolandic groove and especially at the confluence of the sinuses, because this may cause death.

Rice. 14.13. Ligation of the superior sagittal sinus. The needle is placed under the sinus

Rice. 14.14. The needle is passed through the falx of the brain ( falx cerebri)
The simplest and most commonly used method - sinus tamponade, which can be done with a piece of muscle or gauze turundas (Fig. 14.15).
Suturing the sinus wall succeeds only with small linear wounds. Application of a side ligature possible, but only with minor damage. If the condition of the wounded person is very serious, you can apply clamps to the sinus wound and leave them for the period of evacuation. In this case, one should strive to preserve the lumen of the sinus.
If bleeding continues from under the dura mater, it is cut through the wound with thin scissors. Visible bone fragments are removed from the wound canal using thin tweezers. To stop bleeding from the vessels of the brain, diathermocoagulation and tamponing with turundas with hydrogen peroxide are used. The new method proposed Yu. A. Shulevym, is to stop bleeding from a deep brain wound with a fibrin-thrombin mixture, which is prepared immediately before injection into the wound and fills the wound canal in the form of an impression, stopping the bleeding. Human fibrinogen in an amount of 1 g, diluted in 20.0 ml of 0.9% sodium chloride solution and 200 activity units (EA) thrombin in 5 ml of the same solution through an elastic plastic tube connected to a tee, two syringes are simultaneously injected into the wound, the cavity of which is filled with the resulting mixture (Fig. 14.16).
After stopping the bleeding, the wound is loosely packed with napkins, not sutured, and the wounded person is evacuated to the VPNhG for final surgical treatment.
For asphyxia in the dressing room, the upper respiratory tract is sanitized, removing vomit, mucus and blood clots, an air duct is inserted or the trachea is intubated. If there is simultaneous injury to the maxillofacial area or neck, an atypical or typical tracheostomy may be indicated.
Technique for performing tracheostomy the following: the position of the wounded person on his back with his head thrown back, a cushion placed under the shoulder blades. Under local anesthesia A 0.5% novocaine solution makes a longitudinal incision in the skin, subcutaneous tissue and fascia of the neck along the midline of the neck from the thyroid cartilage to a point immediately above the notch above the sternum. The skin, subcutaneous tissue and muscles are bluntly pulled apart with a clamp in the lateral direction. The exposed isthmus of the thyroid gland is retracted upward, if impossible, it is crossed and bandaged. The pretracheal fascia is then opened and the anterior wall of the trachea is exposed. Trachea

Rice. 14.15. Stopping bleeding in wounds of the superior sagittal sinus with tight tamponade

Rice. 14.16. Scheme of filling the wound channel with fibrin-thrombin mixture

Rice. 14.17. Stages of performing longitudinal tracheostomy: a - incision line; b - muscle dilution; c - capture of the trachea with a single-pronged hook; d - section of the trachea; d - view after insertion of a tracheostomy tube into the trachea
It is grabbed with a sharp hook, lifted, and then cut. The trachea is opened with a T-shaped incision: between the 2nd and 3rd rings transversely (cut length up to 1.0 cm), then longitudinally - through the 3rd and 4th rings up to 1.5-2.0 cm long cm. After the trachea incision is made, a tracheal dilator is inserted into it, the hole is widened, and then a previously prepared tracheostomy tube is inserted into it (Fig. 14.17).
The wound should be sutured without tension to prevent the occurrence of subcutaneous emphysema. Applicable only skin sutures. The tracheostomy cannula is held in place by tying it around the neck with gauze.
If there are signs of severe acute respiratory failure, mechanical ventilation is performed.
Everyone else wounded in the head medical care (bandaging, injection of non-narcotic analgesics for pain, repeated administration of antibiotics according to indications, etc.) is carried out in the triage and evacuation department in the scope of first medical aid.
Wounded in the head after preparing for evacuation must be evacuated to GB immediately in the presence of transport, since neurosurgical operations are not performed at the stages of providing qualified medical care. All stretcher wounded are evacuated to VPNhG, walking ones - to VPGLR.
Specialized surgical care for gunshot and non-gunshot injuries of the skull and brain is based on two basic principles: 1) assistance as soon as possible after injury; 2) full, comprehensive and complete nature of surgical interventions(Fig. 14.18.) .
All stretcher wounded with gunshot and non-gunshot brain injuries receive specialized neurosurgical care at the VPNhG.

Rice. 14.18. Tidal drainage after PSO surgery of a craniocerebral wound
Walking wounded with gunshot and non-gunshot head injuries, in whom the medical hospital has not identified focal symptoms of brain damage and the penetrating nature of the injury has been excluded, are sent for treatment to the VPGLR, where there is a specialized neurological department for them.
Control questions:
1. Name the signs of penetrating injury to the skull and brain.
2. What criteria underlie the distinction between open craniocerebral injuries and penetrating injuries of the skull? Name the possible complications of penetrating head wounds.
3. How is it different? clinical picture bruise of the brain from a concussion?
4. What is the difference between the clinical picture of a moderate brain contusion and lung bruise degrees?
5. Name the main thing clinical difference severe traumatic brain injuries from non-severe ones.
6. What degrees of impairment of consciousness are characteristic of severe brain contusions and how do they differ?
7. Name the main reasons for the development of cerebral compression.
8. What clinical picture is characteristic of the development of cerebral compression?
Any head injury is considered dangerous, as there is a high probability of injury. In this case, swelling of the brain tissue rapidly develops, which leads to wedging of part of the brain into the foramen magnum. The result of this is a disruption of the activity of vital centers that are responsible for breathing and blood circulation - a person quickly loses consciousness, and the likelihood of death is high.
Another reason for the high risk of head injuries is the excellent blood supply to this part of the body, which leads to large blood losses in case of injury. And in this case, it will be necessary to stop the bleeding as quickly as possible.
It is important for everyone to know how to correctly provide first aid for head injuries - correctly carried out measures can really save the life of the victim.
Head contusions and soft tissue damage
 TO soft tissues The head includes skin, muscles and subcutaneous tissue. If they are bruised, pain occurs, a little later swelling may appear (the well-known “bumps”), the skin at the site of the bruise becomes red, and a bruise subsequently forms.
TO soft tissues The head includes skin, muscles and subcutaneous tissue. If they are bruised, pain occurs, a little later swelling may appear (the well-known “bumps”), the skin at the site of the bruise becomes red, and a bruise subsequently forms.
In case of a bruise, it is necessary to apply cold to the injured area - this could be a bottle of cold water, a heating pad with ice, or a bag of meat from the freezer. Next, you need to apply a pressure bandage and be sure to take the victim to medical institution, even if he feels great. The fact is that only a specialist can give objective assessment health condition, to exclude damage to the cranial bones and/or.
Damage to soft tissue can also be accompanied by intense bleeding, and possible detachment of skin flaps - doctors call this a scalp wound. If the blood flows slowly and is dark in color, then you need to apply a tight bandage with sterile material to the wound - for example, a regular bandage or piece of fabric ironed on both sides with a hot iron will work as a means at hand. If the blood spurts out, this indicates damage to the artery and the pressure bandage in this case becomes absolutely useless. It will be necessary to apply a tourniquet horizontally above the forehead and above the ears, but only if the scalp is damaged. If the victim has minor blood loss (help was provided quickly), then he is taken to the hospital in a sitting or lying position - he is strictly forbidden to stand. If the blood loss is extensive, then the victim’s skin quickly becomes pale, cold sweat appears on his face, excitement may occur, which turns into lethargy - it is necessary urgent hospitalization and strictly accompanied by an ambulance crew.
First aid procedure:
- The victim is placed on a flat surface, which is covered with something - a jacket, a blanket, any clothing. A cushion is placed under the shins.
- If the patient is in a position, then you need to place your palms on both sides under his lower jaw and slightly tilt his head back, while simultaneously pushing his chin forward.
- The victim's mouth should be cleared of saliva with a clean handkerchief, and then the head should be turned to the side - this will prevent vomit from entering the respiratory tract.
- If the wound contains foreign body, then under no circumstances should you move it or try to remove it - this can increase the volume of brain damage and significantly increase bleeding.
- The skin around the lesion is cleaned with a towel or any cloth, then a pressure bandage is applied to the wound: several layers of cloth/gauze, then any hard object (TV remote control, bar of soap) is placed on top of the wound and bandaged well so that the object compresses the vessel.
- If the bleeding is too severe and it is not possible to apply a bandage, then you need to press the skin around the wound with your fingers so that the blood stops flowing. Such finger pressure must be carried out before the ambulance team arrives.
After the bleeding has stopped, you can apply ice or a bottle of cold water to the wound, carefully cover the victim and urgently take him to any medical facility.
Note:if there is a torn skin flap, then it must be wrapped in sterile cloth (or any other rag), placed in a cold place (application to ice is prohibited!) and sent along with the victim to a medical facility - most likely, surgeons will be able to use this flap of skin for performing operations to restore soft tissues.
Closed head injuries
 If the upper part of the skull occurs, then it is almost impossible to determine whether there is a fracture without. Therefore, if you hit the scalp, it would be a mistake to think that it was just a bruise. The victim must be placed on a stretcher without a pillow, ice applied to the head and taken to a medical facility. If such an injury is accompanied by disturbances of consciousness and breathing, then assistance should be provided in accordance with the existing symptoms, including chest compressions and artificial respiration.
If the upper part of the skull occurs, then it is almost impossible to determine whether there is a fracture without. Therefore, if you hit the scalp, it would be a mistake to think that it was just a bruise. The victim must be placed on a stretcher without a pillow, ice applied to the head and taken to a medical facility. If such an injury is accompanied by disturbances of consciousness and breathing, then assistance should be provided in accordance with the existing symptoms, including chest compressions and artificial respiration.
The most severe and dangerous head injury is a fracture of the base of the skull. This injury often occurs when falling from a height, and is characterized by brain damage. Distinctive feature Fracture of the base of the skull - discharge of colorless fluid (CSF) or blood from the ears and nose. If an injury to the facial nerve also occurs, the victim will experience facial asymmetry. The patient has a rare pulse, and a day later hemorrhage develops in the orbital area.
Note:Transportation of a victim with a fracture of the base of the skull should be extremely careful, without shaking the stretcher. The patient is placed on a stretcher on his stomach (in this case, it is necessary to constantly monitor the absence of vomiting) or on his back, but in this position his head should be carefully turned to the side if he begins to vomit. To avoid tongue retraction when transporting on the back, the patient’s mouth is opened slightly and a bandage is placed under the tongue (it is pulled slightly forward).
Maxillofacial trauma
 In case of a bruise, severe pain and swelling will be noted, the lips quickly become inactive. First aid in this case consists of applying a pressure bandage and applying cold to the injury site.
In case of a bruise, severe pain and swelling will be noted, the lips quickly become inactive. First aid in this case consists of applying a pressure bandage and applying cold to the injury site.
When the lower jaw is fractured, the victim cannot speak; profuse drooling. A fracture of the upper jaw is extremely rare and is accompanied by acute pain and rapid accumulation of blood in the subcutaneous tissue, which radically changes the shape of the face.
What to do in case of jaw fractures:

Note:Transportation of such a patient to a medical facility is carried out lying on his stomach. If the victim suddenly turns pale, then you need to lift the lower end of the stretcher (or just the legs when transporting yourself) so that a rush of blood flows to the head, but you need to be careful not to increase the bleeding.
Dislocation of the lower jaw
This injury is very common because it can happen when laughing, yawning too widely, when hitting, and in older people the usual dislocation of the jaw occurs.
Signs of the condition in question:
- open mouth;
- severe drooling;
- there is no speech (the victim makes mooing sounds);
- jaw movements are difficult.
 Help is to reduce the dislocation. To do this, the person providing assistance needs to stand in front of the victim sitting on a chair. Injected into the mouth thumbs along the lower molars. Then the jaw is forced back and down. If the manipulation was carried out correctly, the victim’s jaw movements and speech are immediately restored.
Help is to reduce the dislocation. To do this, the person providing assistance needs to stand in front of the victim sitting on a chair. Injected into the mouth thumbs along the lower molars. Then the jaw is forced back and down. If the manipulation was carried out correctly, the victim’s jaw movements and speech are immediately restored.
Note:when realigned, the victim’s jaw spontaneously closes with great amplitude and force. Therefore, before carrying out the procedure, you need to wrap your fingers with any cloth and try to immediately pull your hands out of the victim’s mouth immediately after the characteristic click appears (this is the joint snapping into place). Otherwise, injury may be caused to the person providing assistance.
Even with a small wound. The safest wounds are those on the front of the skull, although they look terrifying. It should be remembered that a small wound on the back of the head is much more dangerous than a huge torn surface in the cheek area.
For head injuries the volume first aid, which can be provided to the victim is very small, since in such situations qualified medical assistance is necessary. Therefore, the main help for a victim with a head wound is actually his prompt delivery to a medical facility and stopping the bleeding.
Algorithms for providing first aid for head injuries differ according to two factors - the presence or absence of a foreign object in the wound. Let's consider both algorithms separately.
Algorithm for providing first aid to a victim with a foreign object in a head wound
1. Estimate the likely speed of arrival of the ambulance. If the ambulance medical service can arrive within half an hour, you should call her immediately and then begin providing first aid to the victim. If the ambulance does not arrive within 20 - 30 minutes, then you should begin providing first aid, and then organize the delivery of the victim to the hospital on your own (in your own car, on passing transport, by calling friends, acquaintances, etc.);
2.
3.
If a person is unconscious, his head should be tilted back and turned to the side, since it is in this position that air can freely pass into the lungs, and vomit will be removed outward without threatening to clog the airways;
4.
If any foreign object is sticking out of your head (knife, rebar, chisel, nail, axe, sickle, shell fragment, mines, etc.), do not touch or move it. Do not try to remove an object from the wound, as any movement can increase the amount of damaged tissue, worsen the person's condition and increase the risk of death;
5.
First, inspect the head for bleeding. If there is one, it should be stopped. To do this, you need to apply a pressure bandage. in the following way: Place a piece of clean cloth or gauze folded in 8 to 10 layers at the site of bleeding. Place a hard object on top of the gauze or fabric that will put pressure on the vessel, stopping the bleeding. You can use any small, dense object with a flat surface, for example, a box, a TV remote control, a bar of soap, a comb, etc. The object is tied to the head with a tight bandage made of any available material - bandage, gauze, piece of fabric, torn clothing, etc.;
6.
If it is impossible to apply a pressure bandage, then you should try to stop the bleeding by pressing the vessels with your fingers to the bones of the skull near the site of the injury. In this case, the finger should be held on the vessel until blood stops oozing from the wound;
7.
An object sticking out in the wound should simply be fixed so that it does not move or shift while the victim is being transported. To do this, make a long ribbon (at least 2 meters) from any dressing material at hand (gauze, bandages, fabric, pieces of clothing, etc.) by tying several short pieces into one. The tape is thrown over the object exactly in the middle to form two long ends. Then these ends are tightly wrapped around the protruding object and tied into a tight knot;
8.
After fixing the foreign object in the wound and stopping the bleeding, if any, cold should be applied as close to it as possible, for example, an ice pack or a heating pad with water;
9.
The victim is wrapped in blankets and transported in a horizontal position with the leg end raised.
Algorithm for providing first aid for head injuries without a foreign object in the wound
 1.
Estimate the likely speed of arrival of the ambulance. If the ambulance can arrive within half an hour, you should call it immediately and then begin providing first aid to the victim. If the ambulance does not arrive within 20 - 30 minutes, then you should begin providing first aid, and then organize the delivery of the victim to the hospital on your own (in your own car, on passing transport, by calling friends, acquaintances, etc.);
1.
Estimate the likely speed of arrival of the ambulance. If the ambulance can arrive within half an hour, you should call it immediately and then begin providing first aid to the victim. If the ambulance does not arrive within 20 - 30 minutes, then you should begin providing first aid, and then organize the delivery of the victim to the hospital on your own (in your own car, on passing transport, by calling friends, acquaintances, etc.); 2.
Place the person in a horizontal position on a flat surface, for example, the floor, ground, bench, table, etc. Place a cushion made of any material under your feet so that the lower part of the body is raised by 30 - 40 o;
3.
If a person is unconscious, his head should be tilted back and turned to the side, since it is in this position that air can freely pass into the lungs, and vomit will be removed out without threatening to block the airways;
4.
If there is an open wound on the head, do not try to wash it, feel it, or push the fallen tissue back into the skull cavity. If there is an open wound, you should simply place a clean napkin on top of it and tape it loosely to your head. All other dressings should be applied without affecting this area;
5.
Then examine the surface of the head for bleeding. If bleeding occurs, it must be stopped by applying a pressure bandage. To do this, place a piece of clean cloth or gauze folded in 8 to 10 layers directly on the place from which the blood is flowing. Place a hard object on top of the gauze or fabric that will put pressure on the vessel, stopping the bleeding. You can use any small, dense object with a flat surface, for example, a box, a TV remote control, a bar of soap, a comb, etc. The object is tied to the head with a tight bandage made of any available material - bandage, gauze, piece of fabric, torn clothing, etc.;
6.
If a pressure bandage cannot be applied, then the head is simply wrapped tightly with any dressing material (bandages, gauze, pieces of fabric or clothing), covering the place from which the blood is oozing;
7.
If there are no materials for applying a bandage, then you should stop the bleeding by firmly pressing the damaged vessel with your fingers to the bones of the skull. The vessel should be pressed against the bones of the skull 2–3 cm above the wound. Keep the vessel clamped until blood stops oozing from the wound;
8.
After stopping the bleeding and isolating the open wound with a napkin, it is necessary to place the victim in a lying position with his legs elevated and wrap him in blankets. Then you should wait for an ambulance or transport the person to the hospital yourself. Transportation is carried out in the same position - lying down with legs raised.

