The size of the ovary is normal. Normal size of the ovaries in women before and after childbirth
1. Uterus, size and shape.
The size of the uterus is affected not only by previous pregnancies, but also by the phase menstrual cycle- the uterus is relatively reduced in the proliferative phase and relatively enlarged at the end of the secretory phase. The size of the uterus may vary slightly depending on the research methodology. With TAI, the thickness of the body can be somewhat reduced due to compression by overfilled bladder, and vice versa, with TWI - slightly increased due to an increase in the tone of the myometrium. The shape of the uterus is pear-shaped, and after multiple pregnancies tends to roundness. The normal myometrium has an average echogenicity comparable to the echogenicity of the parenchyma of the unchanged liver, pancreas, and the cortical layer of the kidneys.
The average size of the uterus:
body length of the uterus - 4.4-5.6 cm,
thickness of the body of the uterus - 3.2-4.3 cm,
the width of the body of the uterus is 3.2-5.5 cm.
Cervical dimensions:
cervical length - 2.8-3.7 cm,
thickness of the cervix - 2.6-3.3 cm,
width of the cervix - 2.9-5.3 cm.
In postmenopause, the uterus gradually decreases in size (with an increase in the duration of menopause).
Neck length - 2.9-2.4 cm,
Neck thickness - 2.4-2.1 cm,
Neck width - 2.7-2.3 cm.
The length of the body of the uterus is 3.8-3.3 cm,
The thickness of the body of the uterus is 3.1-2.5 cm,
The width of the body of the uterus is 3.6-3.1 cm.
2. Endometrium.
Ultrasound anatomy of the endometrium is considered in relation to the various phases of the menstrual cycle in the so-called "ideal" cycle, lasting 28 days, with ovulation on the 14th day.
During menstruation, a thin hyperechoic strip is determined in the uterine cavity, or hyperechoic echo structures (blood clots). Sometimes the cavity looks slightly enlarged due to echo-negative content ( liquid blood).
For 5-7 days of the cycle (phase early proliferation) - the endometrium has a relatively low echogenicity and a homogeneous echostructure. The thickness varies between 3-6 mm, averaging 5 mm. In the center of the M-echo, already during this period, a hyperechoic thin line can be determined, representing the border of contact between the anterior and posterior layers of the endometrium.
For 8-10 days of the cycle (phase of medium proliferation) - the endometrium thickens somewhat - on average up to 8 mm (fluctuations of 5-10 mm). The echostructure remains virtually unchanged compared to the previous period.
On days 11-14 of the cycle (phase of late proliferation) - in addition to further thickening, on average up to 11 mm (fluctuations of 7-14 mm), the echogenicity of the endometrium begins to increase slightly - at this stage it can be called average.
On days 15-18 of the cycle (phase early secretion) - a slower growth rate of the endometrium is characteristic, however, the latter continues to thicken, reaching an average of 12 mm (fluctuations of 10-16 mm). Echogenicity continues to increase, and this occurs from the periphery to the center, as a result, the hypoechoic central fragment of the endometrium takes on a drop-shaped appearance (the wide part in the fundus of the uterus, narrowing towards the cervix). In this phase, the hyperechoic line in the center is no longer clearly visualized.
On days 19-23 of the cycle (middle secretion phase) - the endometrium reaches its maximum thickness - an average of 14 mm (fluctuations 10-18 mm). Echogenicity increases even more, the hyperechoic line in the center is poorly visualized.
For 24-27 days of the cycle (phase of late secretion) - the thickness of the endometrium slightly decreases - an average of 12 mm (fluctuations of 10-17 mm). An essential feature of this period is the high echogenicity of the endometrium in combination with a heterogeneous internal echostructure, due to which the line of closure of the leaves ceases to be visualized.
uterine cavity postmenopausal is an M-echo in the form of a thin hyperechoic line 1-2 mm thick. Permissible upper bound norms in postmenopause should be considered the thickness of the M-echo no more than 4-5 mm.
Dopplerography of the uterus pays attention to changes in both the speed and resistance of blood flow, depending not only on the caliber of the vessel, but also on the phase of the menstrual cycle. Doppler evaluation of the endometrium has special meaning when searching for gynecological pathology and should be performed in the early proliferative phase. It is important to emphasize the lack of visualization of intraendometrial blood flow during this period.
In a Doppler study in postmenopausal women, intraendometrial blood flow is normally not visualized.
3. Ovaries
The ovaries are usually located on the side walls of the pelvis in the so-called ovarian fossae - the recesses of the parietal peritoneum at the point of division of the common iliac artery into external and internal. Sonographically, they can be visualized mainly on the side of the uterus, but often they are determined posterior to it or adjacent to one of the uterine angles. As already mentioned, if it is difficult to find the ovary, the anatomical landmarks can be located in the immediate vicinity of internal iliac artery and vein. Normally, the ovaries are well mobile and quite easily displaced when pressed with a transvaginal sensor. The shape of the ovary is ovoid and flattened from front to back. In the reproductive age, the echographic dimensions of the ovaries fluctuate significantly, and this is in to a large extent depends on a number of factors: age, reproductive history, phase of the menstrual cycle, intake oral contraceptives etc.
Ovarian sizes:
Length - 20-37 mm,
Thickness - 16-22 mm,
Width - 18-30 mm,
Volume - 4.0-10.0 cm3.
The sizes of the right and left ovaries in the early proliferation phase are almost the same, but then they can differ significantly depending on the number and size of the antral and dominant follicles, as well as corpus luteum. Thus, in order to detect a pathological enlargement of the ovaries, the study should be carried out on days 5-7 of the menstrual cycle, while determining not the linear dimensions, but the volume, which normally does not exceed 10 cm3, should be considered decisive.
The internal anatomy of the ovary, as well as the uterus, should be considered in relation to the various phases of the menstrual cycle.
The stroma of the ovary, which is the connective tissue basis of the cortical substance, is visualized sonographically as a zone of medium echogenicity, mainly located in central departments ovary.
The ovarian cortex contains follicles varying degrees maturity (follicular apparatus). Numerous (hundreds of thousands) primordial, primary, and secondary follicles are not detected by echography, since their size does not exceed 400 microns.
For 5-7 days of the cycle (phase of early proliferation or early follicular phase) the visualized part of the follicular apparatus is represented mainly by 5-10 tertiary, or antral follicles. The latter have the appearance of rounded echo-negative inclusions with a diameter of 2-6 mm, located mainly along the periphery of the ovary. A network of spiral vessels around the developing follicle appears already at the beginning of the antral phase. At the same time, the blood flow is visualized in the form of a few color loci in the stroma and along the periphery of the antral follicles.
For 8-10 days of the cycle (middle proliferation or middle follicular phase) a dominant follicle usually appears, which is already 12-15 mm in diameter and continues to increase, while the growth of other follicles stops, and they reach 8-10 mm in diameter, undergo atresia (as determined by sonography in a gradual decrease and disappearance towards the end of the menstrual cycle). The blood supply of the dominant follicle usually comes from two or three stromal arteries, usually visualized along the periphery, or even in the wall of the latter. At the same time, Doppler parameters of stromal arteries and arteries of the dominant follicle do not differ significantly.
On days 11-14 of the cycle (late proliferation phase or late follicular phase) the dominant follicle increases by 2-3 mm per day, reaching 18-25 mm by the time of ovulation (average 20 mm). The prognostic signs of ovulation, indicating that the latter will occur in the next few hours, include: the diameter of the dominant follicle is 18 mm, a double contour around the latter, as well as fragmentary thickening and unevenness of the inner contour of the dominant follicle. Vascularization of the dominant follicle becomes subjectively more noticeable compared to other follicular structures, also only on the eve of ovulation.
About what happened ovulation echographically, it can be judged by the disappearance of the dominant follicle or a decrease in its size with deformation of the walls and the appearance of echogenic contents in the cavity, as well as the appearance of fluid in the Douglas space.
On days 15-18 of the cycle (phase of early secretion or early luteal phase) is characterized by the appearance at the site of ovulation of a corpus luteum with a diameter of 15-20 mm (usually smaller than the dominant follicle), which has an irregular shape, uneven contours, and an extremely diverse internal echostructure of varying degrees of echogenicity. This peculiar echographic polymorphism can be easily explained by the morphological substrate of the nucleus of the corpus luteum, which is blood clot in varying degrees of thrombus formation and lysis.
On days 19-23 of the cycle
(middle secretion phase or middle luteal phase) for the "blooming" corpus luteum, a slight increase in diameter (up to 25-27 mm) is characteristic, as well as the appearance of an unevenly thickened echo-positive roller. The echogenicity of the contents due to lysis can gradually decrease until the formation of a "cystic" corpus luteum.
During the first days after ovulation, a dense, multilayered vascular network is formed around the corpus luteum, which is especially pronounced in the flowering phase. On color Dopplerograms, a pronounced color ring appears around the corpus luteum, the blood flow in which is characterized by high velocity and low impedance. This is typical of violent physiological neovascularization.
For 24-27 days of the cycle
(phase of late secretion or late luteal phase) the "fading" corpus luteum decreases in size (10-15 mm), its echogenicity increases slightly, and the echostructure becomes more homogeneous. At the same time, the corpus luteum is often poorly visualized sonographically. In the absence of pregnancy, the blood supply to the corpus luteum begins to change by about 9 days after ovulation. The tissue of the corpus luteum begins to undergo luteolysis, the capillaries contract and reduce, which is characterized by a noticeable depletion of local blood flow.
During menstruation, the corpus luteum, as a rule, is no longer defined, or a fuzzy echo structure of increased echogenicity with a diameter of 2-5 mm remains in its place ( white body), which usually disappears without a trace during the next menstrual cycle. It has been proven that a non-passing white body in the form of a scar is preserved only after a gravid corpus luteum. Blood circulation in the vessels of the disappearing corpus luteum stops, and the vessels themselves disappear during the first three days of menstruation.
The results of studies of Doppler parameters of intraovarian blood flow conducted by many authors, as well as our own data, demonstrate significant cyclic changes in the rate and peripheral resistance of intraovarian blood flow in the ovulating ovary in different phases of the menstrual cycle.
Postmenopausal
the ovaries are significantly reduced, while the size of the right and left ovaries should be almost the same.
The length of the ovary is 25-20 mm,
The thickness of the ovary is 12-9 mm,
The width of the ovary is 15-12 mm,
The volume of the ovary is 4.5-1.5 cm3.
It should be emphasized that indicators exceeding the limits of the age norm, as well as a difference in the volumes of the right and left ovaries of more than 1.5 cm3, are signs of pathology. An asymmetric increase in one of the ovaries by more than two times should be considered a marker of malignancy.
During the postmenopausal period, the follicular apparatus gradually undergoes an almost complete reduction. The first 5 years after menopause in the ovarian parenchyma "have the right" to visualize single follicles with a diameter<10 мм. В последующем яичники выглядят как образования
овальной формы, эхоструктура которых характеризуется достаточно
однородной средней эхогенностью. Мы убеждены, что после 5-ти лет
постменопаузы визуализация в яичниках персистирующих кистозных
включений любых размеров должна рассматриваться как патология.
Intraovarial perfusion in postmenopausal women is extremely low. If in the first 5 years single color loci are still detected by both color and power Doppler sonography, then already in the next 5 years of postmenopause, the color Dopplerogram is usually completely achromatic and blood flow can only be detected using power Doppler sonography. After 10 years of postmenopause, intraovarian blood flow is usually not visualized even with power Doppler.
Ultrasound diagnostics (ultrasound) is the fastest, safest and most informative method of examination in medicine. Recently, various gynecological pathologies have begun to occur more and more often, so it is important to know the normal size of the uterus and ovaries by ultrasound.
There are different prerequisites according to which a doctor may prescribe an ultrasound. Common ones:
- severe pain during menstruation;
- regular violations of the cycle;
- frequent pain in the area of the ovaries or uterus;
- to establish a possible pregnancy and exclude the formation of an ectopic pregnancy;
- with the appearance of strange vaginal discharge that is not associated with menstruation.
Thanks to ultrasound diagnostics, it is possible to timely identify various pathologies of the internal organs of a woman and prevent the formation of serious complications.
How is the ultrasound
The following methods are used for ultrasound examination:
- transabdominal
- Transvaginal.
Let's take a brief look at each of the methods.
Transabdominal ultrasound diagnostics
This research method is carried out through the abdomen. For a better glide of the device over the skin, a special gel is applied to the diagnosed area by the doctor. For free penetration of ultrasonic waves, an important requirement of this method is a filled bladder.
Transvaginal ultrasound diagnostics
The study is carried out with a special device through the vagina. To avoid infection, a condom is put on the device. With such an examination, the bladder, on the contrary, should be empty. This method is more accurate than the first one.
The diagnostic procedure does not cause any discomfort and pain, and also does not have a negative effect on the female body. However, it is important to know what sizes of the ovaries and uterus are normal according to ultrasound.

The norm of ultrasound diagnostics of the ovaries
Ovarian sizes
The normal size of the ovaries in women are:
- width - 25 mm;
- length - approximately 30 mm;
- thickness - 15 mm;
- the volume of each ovary should not exceed 80 mm ³ .
In the case of an increase in the size of the ovaries, the presence of inflammation or a serious pathology of these organs is possible.
Structure of the ovaries
The correct structure of the ovaries: capsule and follicles. The number of the latter may not be the same in both the right and left organs.
Echogenicity and external contours of the ovaries
Ovaries without pathologies should have a clear and bumpy outer shell, as well as uniform echogenicity. Fuzzy contours indicate the development of inflammatory processes (for example,).
The norm of examination of the uterus by ultrasound
Feeling alarming symptoms, the woman is sent for examination. With the proper functioning of the reproductive organs, all the studied indicators should be normal.
To assess the general condition of the uterus, the doctor examines the following indicators on ultrasound.
Body position
The uterus is located between the upper part of the rectum and the bladder. It is considered correct when the organ is tilted forward towards the rectum or urinary. The doctor carefully examines the location of the uterus and indicates everything in the protocol.
Organ contours
Normally, an organ with a flat and smooth surface is considered. On the body of the uterus there should be no cicatricial changes, neoplasms, thinning. An uneven contour can indicate the presence of inflammation.
Endometrial size
The endometrium is the mucous lining of the uterus. In patients of reproductive age, its thickness may vary depending on the period of the cycle. If the diagnosis was carried out immediately after the end of menstruation, this value is approximately 1-2 mm, after ovulation its width reaches 10-15 mm.
In women during menopause, the thickness of the endometrium does not change throughout the month. Over the years, after the cessation of its functions, the endometrium gradually becomes thinner. At the beginning of menopause, its thickness is about 8.5 mm, and after 10 years it can become less - 1.32 mm.
Uterine size
If the uterus is normal, then its size depends on the age, number of pregnancies and is approximately 45-70 mm. The anterior-posterior size of the body of the uterus varies in the range from 34 mm to 44 mm, width - 45-60 mm.
If the uterus is smaller than normal, underdevelopment of the organ can be suspected. When these indicators are increased, this indicates the presence of pregnancy or.
The nulliparous uterus has the following dimensions:
- length - 4.5 cm;
- thickness - 2 cm;
- width - 2.5 cm.
During the period of pregnancy, the uterus in length increases to 40 cm and becomes heavier. 
Cervical parameters
The cervix, which does not have pathologies, is homogeneous. Its correct size is on average 35-40 mm. The cervical canal should contain a homogeneous fluid (mucus) and be approximately 2-3 mm in diameter.
An increase in the cervical canal or the cervix itself may indicate the development of various pathologies.
echogenicity
This parameter indicates the density of tissues. The norm is homogeneous echogenicity. In the presence of any other indicators, the development of a neoplasm or fibroids is possible.
Presence of free fluid
After ovulation, small amounts of fluid may be observed in the retrouterine zone. But in other periods of the menstrual cycle, the presence of this fluid indicates possible pathologies that are caused by sexual infections.
cavity structure
In a healthy body, the uterine cavity is homogeneous. A blurred structure indicates endometrial disease or the presence of neoplasms.
The doctor enters all the data of the examination into the protocol. By evaluating the above indicators, he can establish an accurate diagnosis.
Ultrasound of the uterus and ovaries is rightfully considered a fairly informative diagnostic method, which is prescribed for violations of the functioning of the organs of the woman's reproductive system. If the ultrasound examination did not help to establish an accurate diagnosis or the doctor has any doubts, the patient is recommended to donate blood for hormones, bacterial culture and other tests.
Ultrasound examination of the uterus and ovaries in gynecology is considered the most affordable and effective method of examination. With the help of ultrasound, the doctor can quickly diagnose various gynecological diseases in women, assess the size, location and structure of the female reproductive organs.
uterus and ovaries
In what cases is the study assigned?
There are certain indications for the appointment of ultrasound diagnostics of the condition of the uterus and ovaries. These include:
- Conducting folliculometry when planning pregnancy.
- Diagnosis of pregnancy, determination of the place of attachment of a fertilized egg (to exclude ectopic pregnancy).
- Ultrasound is done as part of IVF.
- Identification of ovarian cysts.
- Complaints of pain in the lower abdomen.
- Menstrual irregularities.
- Bloody discharge outside of menstruation.
- Profuse, painful menstruation.

Dysmenorrhea
- Pain in the lower back.
- Suspicion of cancer of the uterus and ovary, diagnosis of a uterine polyp.
Types of ultrasound diagnostics in gynecology
There are two main methods for performing ultrasound of the pelvic organs:
- Transvaginal ultrasound - done using a special sensor that is inserted into the woman's vagina. The method is more accurate, it can show pregnancy in the early stages, but in some cases its use is impossible.
- Transabdominal - the doctor makes a scan through the abdominal wall, the organs are better visualized with a full bladder.
How to prepare for the examination?
Preparation for the study directly depends on what methods the doctor will use in diagnosis.
When conducting a transvaginal examination, a woman is advised to prepare - to completely empty her bladder.
With a transabdominal examination, the preparation is that the bladder should be as full as possible. This is due to the fact that ultrasonic waves pass well through the aquatic environment, which significantly improves the visualization of internal organs. Therefore, shortly before the examination, it is recommended to drink about a liter of liquid - plain water or tea.

1.5 hours before the transabdominal examination, you must drink up to 1 liter of water
It is important to find out in advance the method by which the study will be carried out so as not to confuse the method of preparation.
A common point in preparing for both types of research is to limit the use of foods that increase gas formation in the intestines the day before the examination - swollen intestinal loops prevent the passage of ultrasound to the pelvic organs, distorting the results.
When is the best time to do research?
In order to diagnose gynecological diseases, the study is best done in the first days of the cycle - 5-7 days after the onset of menstruation, when the endometrium (the inner lining of the uterus) has the smallest thickness, due to which visualization is better and the likelihood of detecting tumors and polyps increases.
In order not to confuse the days of the cycle and correctly come to the examination, women are advised to keep a calendar in which the days of menstruation should be noted.

Menstruation calendar
To assess ovarian function, it is better to do several ultrasounds within the same menstrual cycle. It is revealed which follicle is dominant, the course of its maturation, the release of a mature egg and the formation of the corpus luteum are monitored. The presence of cysts on the surface is also diagnosed. The correct course of all these processes play a major role in a woman's ability to become pregnant and bear a child.
Interpretation of survey results
When performing ultrasound diagnostics of the pelvic organs, the doctor acts according to the examination protocol, which includes the study of the following parameters:
- Location of the uterus in the pelvis: Normally, the uterus is in the anteflexio position, that is, it is slightly tilted forward.
- External contour of the uterus: normally clear and even. Rough contours can be caused by benign tumors or cancer. When the doctor reveals the blurring of the edges, then we can talk about the inflammatory process of the surrounding tissues.
- Dimensions: average length is 7 cm, thickness 6 cm, length in the anterior-posterior direction can be within 4.5 cm.
- Echogenicity of the myometrium: normally homogeneous, an increase in this parameter raises the question of the development of cancer.
- : this parameter directly depends on what day of the woman's menstrual cycle. To facilitate the diagnosis, changes in the endometrium were divided into phases:
- Regeneration - restoration of the endometrium after menstruation (2-4 days, the beginning of the cycle).
- Proliferation is the growth of the endometrium. The thickness of the mucosa can increase from 3-5 to 10-15 mm (5-14 days).
- Secretory phase - the thickness of the endometrium during this period reaches its maximum values on the day of ovulation - 16-20 mm. The mucous membrane is preparing for a possible pregnancy.

Pathological and normal endometrium
- Assessment of the state of the uterine cavity: uniform with clear and even edges.
- Condition of the cervix: the length of the neck can normally be 36-41 mm, the cervical canal is filled with a mucous mass. The diameter of the endocervix is 2-4 mm. In the case when the diameter is increased, they talk about the presence of inflammation or serious diseases such as cervical cancer and endometriosis.
- Free fluid in the retrouterine space: Normally, in the second half of the menstrual cycle, there may be a small amount of fluid in the pelvis that came out of the ovary when the dominant follicle ruptured. The presence of fluid behind the uterus in the first half of the cycle indicates the presence of an inflammatory process in the small pelvis.
- Evaluation of the condition of the ovaries: during the examination, the doctor pays attention to the contours of the organs - normally clear and bumpy due to the presence of follicles on their surface. The dimensions of the ovaries are normally 2.5 cm wide, 3 cm long and 1.5 cm thick. On ultrasound, one dominant follicle and several ripening follicles should be determined.
Ultrasound examination for various diseases of the uterus and ovaries
ovarian cysts
A cyst is a hollow pathological formation filled with fluid and located on the surface or in the body of the ovary. In most cases, the development of cysts is due to the physiological function of the organ and does not pose a serious danger. However, in some cases, the rupture of the dominant follicle does not occur on the day of ovulation, it increases in size and degenerates into a follicular cyst. Such cysts are called functional, since their appearance is due to the normal functioning of the ovaries. In most cases, the formation goes away on its own within a few cycles and does not interfere with the onset of pregnancy. On ultrasound, an ovarian cyst looks like a rounded bubble filled with hypoechoic fluid.
ovarian cancer
Ovarian cancer is a malignant neoplasm that develops on the surface and in the body of an organ. The exact causes that can cause this serious disease have not yet been identified. One theory is that the cancer is caused by a disruption in the normal healing process on the surface of the ovary after the follicle ruptures during ovulation. There is evidence of a relationship between the disease and hereditary predisposition and the age of the patient - young women get sick less often. Less commonly, cancer occurs in women who have gone through pregnancy and breastfeeding. When conducting an ultrasound, the doctor is able to assume the presence of cancer, noticing on the monitor a pathological formation of various sizes with clear edges. To clarify the diagnosis, laparoscopy is done.
Ultrasound examination of the pelvic organs is of great importance in identifying early gynecological pathologies. Timely diagnosis of serious pathologies can save a woman from serious problems, so it is better to do monitoring at least once a year.
The best way to check the internal organs is an ultrasound. Very often it is used in gynecology. After all, the result can be obtained quickly, safely and accurately.
What is an ultrasound for?
The reasons why a doctor prescribes an ultrasound of the uterus and ovaries are varied. So, for example, they could be:
- a woman may be disturbed by pain in the uterus and ovaries;
- permanent violations of the cycle;
- severe pain that occurs during menstruation;
- in the event of suspicious vaginal discharge, but not related to menstruation;
- in addition, such a study should be done by women in order to determine the presence of pregnancy and to exclude ectopic pregnancy.
Thanks to this method, any deviations from the norm and the onset of diseases can be detected.
Process
Many women are interested in how the ultrasound of the uterus and ovaries goes. Two methods are commonly used for this study.
- Transabdominal ultrasound. This method is based on the study of organs through the abdomen. To do this, the doctor applies a little special gel to the lower abdomen, which allows the sensor to glide better over the skin. In addition, if the doctor prescribes this type of ultrasound, it is necessary that the bladder is full. The fact is that ultrasound waves penetrate well through the aquatic environment, but through the air - on the contrary.
- Transvaginal ultrasound. In this case, a special device is inserted into the woman's vagina, with the help of which the examination is carried out. In order to avoid infections, a special condom is put on it. In this case, on the contrary, it is necessary that the bladder is empty. This method is considered more accurate than the previous one.
The process itself does not cause any pain at all, does not have a negative effect on the body and passes quickly enough.
Uterine parameters
During such an examination, the doctor evaluates certain parameters of the uterus in women.
- Position. The position is considered normal when the uterus is tilted towards the bladder or rectum, i.e. forward. If the organ has a backward deviation, then this may well become a problem during pregnancy, because. this is not considered the norm.
- outer contours. The outer shell of the organ should be even and have a clear boundary. With fibroids or tumor diseases, the contours will, on the contrary, be uneven. If the boundaries are not clear, then this may indicate inflammation.
- Size. It is considered normal when the length of the uterus is in the range from 45 mm to 70 mm, depending on the age of the woman, the number of pregnancies. The width of the body is in the range from 45 mm to 60 mm and also depends on these indicators. Anterior-posterior size - from 34mm to 44mm. If the size of the uterus is less than normal, then this indicates its underdevelopment. If, on the contrary, the values are greater, then this may be a sign of pregnancy or tumor diseases.
- thickness of the endometrium. The doctor must examine this indicator. The fact is that the thickness of the endometrium is different depending on which day of the cycle the ultrasound is performed. Therefore, the doctor looks at the correspondence of this value to the day when the procedure takes place. Immediately after menstruation ends, the thickness of the endometrium is approximately 1-2 mm, but after ovulation occurs, its size varies from 10 to 15 mm.
- echogenicity. This indicator shows the density of the fabric. For the uterus, homogeneous echogenicity is considered normal. If any other indicators are present, then this may indicate the presence of fibroids or tumors.
- The structure of the uterine cavity. The cavity of this organ in healthy women is homogeneous, with clear contours. Its blurring indicates that endometrial diseases are present. In addition, ultrasound may show any neoplasms.
- Cervix. The normal size is from 35 to 40 mm. However, it must be homogeneous. The diameter of the cervical canal is approximately 2-3 mm. There must be liquid inside it. If the canal or the neck itself is dilated, then this indicates possible diseases.
- The presence of free fluid. After ovulation, women may have some fluid in the retrouterine space. However, on any other day of the cycle, the presence of such a liquid indicates possible diseases provoked by sexual infections.
Ovarian parameters

In addition to examining the uterus, doctors necessarily conduct an examination of the ovaries. These are paired organs, during the procedure the condition of one and the other is assessed. What parameters does the specialist consider, and what values \u200b\u200bare considered the norm?
- Location and shape. Both organs are located on the sides of the uterus. Moreover, this arrangement is most often asymmetrical. In healthy women, the ovaries are oval. The follicular apparatus is clearly defined, the follicles are clearly visible in it. If an ultrasound is done on the 8-9th day of the cycle, then the specialist will determine the dominant follicle, which at this time can be from 15 to 25 mm in size. If its size exceeds this value, then this indicates the possibility of a follicular cyst.
- Ovarian size. A normal indicator is when the width of the ovary is 25 mm, the length is about 30 mm, and the thickness is 15 mm. If these values differ upwards, then there may be inflammation or even serious diseases of these organs.
- External contours and echogenicity. The outer shell of the ovaries should be clear and bumpy (due to the growth of follicles). Echogenicity should normally be homogeneous. If the contours are blurred, then this indicates inflammatory processes.
- Structure. The ovaries are composed of follicles and a capsule. The number of the first may differ in the left and right organs.
The fallopian tubes
On ultrasound, the fallopian tubes, if they are in normal condition, should not be visible. If the specialist nevertheless detects them, then we can talk about the inflammatory processes present in them.
Diseases
Often a doctor, when comparing the data obtained with the results of the examination, can determine the presence of any disease. What is the diagnosis?
- Myoma. At the same time, the size of the uterus is larger than normal, its contours are blurred, and a node is determined in the myometrium.
- Endometriosis. This disease occurs as a result of the fact that endometrial cells begin to grow outside the uterus. On ultrasound, it can be seen as a number of bubbles that can be located in the uterus, and in its neck, and in the fallopian tubes.
- Incorrect development of the uterus. These may be her shortcomings in her development, for example, a bicornuate uterus or hypoplasia of this organ.
- Endometritis. In this case, the endometrium becomes thicker, its edema may occur. The size of the uterus also changes in the direction of increase.
- Uterine cancer. In this case, large formations in the cavity of this organ are determined on ultrasound.
- Cervical cancer. At the same time, the specialist sees that the size of the neck is much larger than the norm, and it is deformed due to the disease.
- Cyst. If a formation filled with fluid and exceeding 25 mm in diameter is found in the ovary, then most likely there is a disease such as an ovarian cyst.
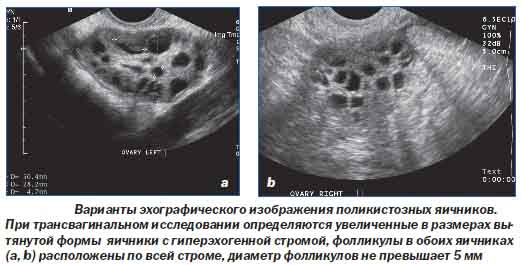
- Polycystic. The size of both ovaries exceeds normal values, they become thicker. In addition, fibrosis is determined.
- Adnexitis. If this disease is present, then the ultrasound clearly shows that the fallopian tubes have rather thick walls, the ovaries become larger in size, their boundaries become fuzzy.
Pregnancy
Ultrasound of the uterus and ovaries during pregnancy is mandatory. Their sizes change. So, for example, the uterus is stretched to a length of about 40 cm. The ovaries also increase in size, but not much. And the reason for this is increased blood flow to the pelvic organs during pregnancy. Besides, ultrasound examination will help to identify pathologies of organs and the fetus if they ever show up. After childbirth, the uterus returns to its normal size, and the ovaries begin to function normally again.
Ultrasound of the uterus and ovaries is a necessary procedure for suspected diseases or pregnancy. This is not a terrible study at all, but it is it that gives the most complete and accurate answer to many questions.
Every woman had to undergo an ultrasound examination of the pelvic organs. Having received the results of the ultrasound, each of us begins to think: are the sizes of the genital organs normal or not? It is necessary to figure out what is the normal size of the ovaries in a woman. The rate depends on many factors.
The ovaries are the female sex glands. They form and mature the basis of life - the egg. The ovaries are located on the left and right sides of the uterus. Determining their exact location is not difficult even for a specialist with little experience. The main landmark is the iliac vein.
The ovaries produce the necessary sex hormones and contain germ cells - follicles. The development of the ovaries begins in the womb and by 5 months they are already clearly visible with follicles inside. Further, the germ cells atrophy and a newborn child has a huge number of them - 0.5 million. Only 500 follicles will mature and the rest will degenerate. With their complete disappearance, menopause and irreversible changes in the female body occur.
In a healthy woman, the ovaries are flattened and very mobile. In reproductive age, the left and right ovaries are not symmetrical and differ in size. This is not a deviation and is considered normal development and functioning.
The size of the ovaries is influenced by a number of factors:
The number of pregnancies and childbirth;
Use of oral agents to prevent unwanted pregnancy;
phase of the menstrual cycle.
The size range is very wide.
To detect the pathological development and size of the ovaries, an ultrasound examination is performed from 5 to 7 days of the menstrual cycle. Pay attention not to the linear size, but to the volume.
The normal volume of the ovaries is considered to be from 4 to 10 cubic centimeters. Overall dimensions should be in the following ranges: thickness 16 - 22 mm, length - 20 - 37 mm, width - 18 - 30 mm.
in the study of internal anatomy, the phase of the menstrual cycle is taken into account. From the outside, the ovaries are covered with a white membrane. Under it there are two layers: first cortical, and then brain. In the cortical (outer) layer during the reproductive age, follicles are located at different stages of maturity: primordial (immature) and prevolutory (mature).
On day 5-7 - the early follicular phase, you can see the protein capsule and up to 10 follicles in the periphery of the ovaries, the size of which can vary from 2 to 6 millimeters.
On days 8-10 of the menstrual cycle - the middle follicular phase, a dominant follicle is visible, the size of which reaches 15 millimeters. He continues his further development, while the rest stopped at 8-10 millimeters.
On days 11-14 during the late follicular phase, the dominant follicle reached 20 millimeters. Every day it adds up to 3 millimeters in diameter. About the imminent onset of ovulation, the size of the follicle is 18 millimeters with a modified internal and external contour.
Day 15-18 of the menstrual cycle is called the early luteal phase. During this period, a corpus luteum of 15-20 millimeters appears at the site of ovulation.
The next 4 days (mid luteal phase) the corpus luteum grows to 27 millimeters. The late luteal phase begins. The corpus luteum becomes smaller - up to 10 millimeters. At the beginning of menstruation and during its continuation, the corpus luteum is completely absent.
If pregnancy occurs, then the corpus luteum continues its development for 12 weeks. It produces progesterone and blocks the release of a new egg.
Increased and active blood flow during pregnancy leads to enlargement of the ovaries. The growing uterus causes them to move upward from the pelvic area.
Before the onset of menopause until the age of 40, ovarian exhaustion and infertility may occur. The patient is prescribed hormonal drugs.
After the onset of postmenopause, the ovaries are significantly reduced in size. Left and right become the same. At this stage, the female body is considered to be noma ovarian volume from 1.5 to 4 cubic centimeters. The linear dimensions must correspond to the following values: thickness - from 9 to 12 millimeters, length - up to 25 millimeters, width - from 12 to 15 millimeters.
If the difference in the ovaries is more than 1.5 cubic centimeters, then they talk about pathology. An increase in one of the ovaries by 2 times compared to the other is also considered a deviation from the norm. The first 5 years, follicles may be present in the ovaries, which are the norm.

