Medicines affecting blood function. Drugs affecting the blood system
"For the life of every body is its blood,
she is his soul..."
(Bible. Old Testament. Leviticus. Chapter 17)
Blood is a type of tissue. Basic functions of blood, the hemostatic system that supports blood functions. Medicines that promote and prevent blood clotting. Agents that dissolve blood clots and reduce the risk of thrombosis. Hematopoiesis, drugs that stimulate this process.
Since ancient times, the belief has been preserved that it is in the blood that the most important thing is hidden, which determines the character, fate, and essence of a person. Blood has always been surrounded by an aura of holiness.
We say “hot blood”, “it’s in his blood”, “blood calls for revenge or heroism” and so on.
The mystical idea of blood as a carrier of a person’s spiritual qualities reached the point that even doctors wondered whether a blood transfusion could strengthen friendship, reconcile discordant spouses, and warring brothers and sisters.
A few more examples from history that demonstrate the importance people attached to blood. Homer's hero Odysseus gave blood to the shadows of the underworld to restore their speech and consciousness. Hippocrates recommended that seriously ill patients drink the blood of healthy people. The blood of dying gladiators was drunk by the patricians of Ancient Rome. And to save the life of Pope Innocent VIII, a medicine was prepared from the blood of three young men.
What is blood, and what is the reason for this attitude towards it?
Life originated in the ocean. And when multicellular organisms came to land, they took with them a particle of the ocean - sea water. This water, which has turned into blood, circulates under the pressure of the pump (heart) through a closed system (vessels) and allows cells to exchange nutrients, removes cellular decay products from them, evenly distributes heat between them, and so on, that is, it does everything that allows individual cells, sometimes located at a great distance from each other, to merge into a single organism.
Blood is a type of connective tissue. It continuously moves through the blood vessels. Blood movement is supported by the cardiovascular system, in which the heart and smooth muscles of the walls of arteries and veins play the role of a pump. Blood is one of the three components of the internal environment that ensures the normal functioning of the body as a whole. The other two components are lymph and intercellular (tissue) fluid. Blood is necessary to transport substances throughout the body. Blood is 55% plasma, and the rest is suspended in it blood cells - red blood cells, white blood cells and platelets. In addition, it contains cells ( phagocytes ) And antibodies , protecting the body from pathogenic microbes.
If a person weighs 65 kg, he has 5.2 kg of blood (7-8%); out of 5 liters of blood, about 2.5 liters are water.
As can be easily seen from the figure, blood clotting is based on the conversion of soluble plasma protein fibrinogen into dense protein - fibrin . The agents of the process include calcium ions and prothrombin. If you add a small amount of sodium oxalate or sodium citrate (sodium citrate) to fresh blood, coagulation will not occur, since these compounds bind calcium ions so strongly. This is used when storing donor blood. Another substance that is required for the normal blood clotting process is the previously mentioned prothrombin. This plasma protein is produced in the liver, and its formation requires vitamin K. The components listed above (fibrinogen, calcium ions and prothrombin) are always present in the blood plasma, but under normal conditions coagulation does not occur.
The fact is that the process cannot begin without one more component - thromboplastin - an enzyme protein contained in platelets and in the cells of all tissues of the body.
When you cut your finger, thromboplastin is released from the damaged cells. Thromboplastin is also released from platelets that are destroyed during bleeding. When thromboplastin interacts with prothrombin in the presence of calcium ions, the latter is cleaved and forms the enzyme thrombin, which converts the soluble protein fibrinogen into insoluble fibrin. Platelets play an important role in the mechanism of stopping bleeding. As long as the vessels are not damaged, platelets do not stick to the walls of the vessels, but if their integrity is violated or pathological roughness appears (for example, “atherosclerotic plaque”), they settle on the damaged surface, stick together and release substances that stimulate blood clotting . This forms a blood clot, which, as it grows, turns into a thrombus.
Thus, it becomes clear that the process of thrombus formation is a complex chain of interactions of various factors and consists of several stages. At the first stage, tomboplastin is formed. A number of plasma and platelet coagulation factors take part in this phase. In the second phase, thromboplastin, in combination with blood coagulation factors VII and X and in the presence of calcium ions, converts the inactive protein prothrombin into the active enzyme thrombin. In the third phase, the soluble protein fibrinogen (under the influence of thrombin) is converted into insoluble fibrin. Fibrin threads, woven into a dense network, with captured platelets form a clot - a thrombus - covering the defect of the blood vessel.
The fluid state of the blood under normal conditions is maintained by an anticoagulant substance - antithrombin . It is produced in the liver and its role is to neutralize small amounts of thrombin that appear in the blood. If, nevertheless, the formation of a blood clot occurs, then the process of thrombolysis or fibrinolysis begins, as a result of which the clot gradually dissolves and the patency of the vessel is restored. If you look again at, or rather at its right side, you can see that the destruction of fibrin occurs under the action of the enzyme plasmin . This enzyme is formed from its predecessor plasminogen under the influence of certain factors called plasminogen activators .
Special preparations obtained from plasma and containing individual blood clotting factors also have coagulant properties. For example, antihemophilic factor VIII and factor IX complex. Such drugs are used to normalize hemostasis in patients hemophilia .
Thrombin and fibrinogen (isolated from the blood) are also used to stop bleeding. Both are natural components of the coagulation system (see above). To avoid extensive generalized thrombosis, thrombin is used only locally. Fibrinogen, as a precursor of fibrin (and not the clot-forming protein itself), can be administered both locally and intravenously. Combination drug Tissucol Kit consists of two sets, mixed before use, and contains fibrinogen and thrombin.
Drugs in this group inhibit blood clotting and/or promote the resolution of existing blood clots. There are direct and indirect anticoagulants.
Direct anticoagulants include heparin and its derivatives. Heparin is a natural anticoagulant found in mast cells (connective tissue cells) and released in response to increased thrombin activity. Medical heparin is obtained from the lungs of cattle.
Anticoagulants of the heparin group ( heparin sodium, nadroparin calcium, reviparin sodium, enoxaparin sodium) have a rapid effect because they bind (inhibit) coagulation factors directly in the blood.
Another group of anticoagulants consists of drugs that reduce the activity of vitamin K, which ensures the synthesis of prothrombin and a number of other coagulation factors in the liver. Since they do not affect the activity of already formed coagulation factors, their effect develops slowly and reaches a maximum when reserves of, for example, prothrombin are depleted. Typically, the effect of such medications begins 12-24 hours after administration. Such drugs are called indirect anticoagulants.
In the late 20s and early 30s in North America, cases of death of cattle from bleeding due to seemingly ordinary reasons - dehorning, castration, injuries - became frequent. An initially unclear connection was established between these cases and the use of overripe clover affected by mold as food. A long search began for a substance contained in clover that caused bleeding in animals. This search was crowned with success in 1939, when K. Link, a professor at the University of Wisconsin, and his collaborator Campbell obtained dicoumarin crystals. Subsequently, dicoumarin became the first drug in the group of indirect anticoagulants. Coumarins are found in many plants and are widely used in the perfume industry. The presence of coumarin is responsible for the unforgettable smell of freshly cut grass and hay. Coumarin derivatives are widely used drugs: acenocoumarol, warfarin, ethyl biscoumacetate. In addition to coumarins, indanedione derivatives have the properties of indirect anticoagulants, for example, phenindione.
Anticoagulants of both direct and indirect action are used for prevention and treatment thrombosis , thrombophlebitis And embolism for venous diseases, heart diseases, including vascular operations.
These drugs destroy blood clots by either dissolving fibrin itself or promoting the formation of the enzyme plasmin from its inactive precursor, plasminogen. Recall Figure 2.6.1 at the beginning of the chapter. It is plasmin that causes the destruction of fibrin (fibrinolysis), the protein that forms the basis of the blood clot. Therefore, by activating its precursor, plasminogen, it is possible to cause increased fibrinolysis. Enzymes have these properties streptokinase And urokinase, as well as tissue plasminogen activator alteplase, obtained by genetic engineering.
Preparations based on these substances are indicated for multiple pulmonary embolism , thrombosis of central veins , at peripheral vascular diseases and at acute myocardial infarction .
In contrast to fibrinolytics, substances in this group stabilize fibrin and help stop bleeding. Occupying the binding sites of plasmin (plasminogen) in the fibrin molecule, they deprive it of the ability to dissolve fibrin. This is how they act tranexamic acid, aminocaproic acid And para-aminomethylbenzoic acid. Other substances, e.g. aprotinin(obtained from the lungs of cattle), are natural inhibitors of proteolytic enzymes ( trypsin , chymotrypsin ), including plasmin. Therefore, in addition to fibrinolytic properties, they reduce the level of proteases in tissues and blood and are used for inflammation of the pancreas. All these drugs are effective for bleeding caused by increased fibrinolytic activity of blood and tissues, after operations and injuries, before, during and after childbirth, and for complications arising as a result of thrombolytic therapy.
As mentioned earlier, platelets play an important role in stopping bleeding by adhering to the walls of damaged vessels and forming aggregates around which a blood clot forms. However, this same property of platelets causes narrowing of the lumen and even blockage of intact vessels if their inner surface ( endothelium ) is broken for some reason. During normal functioning, platelets do not unite (no aggregation), this is regulated by the ratio of two prostaglandins : thromboxane (in platelets) and prostacyclin (in the endothelium). Thromboxane stimulates, and prostacyclin inhibits platelet adhesion. With a coordinated ratio of these prostaglandins, which are transformation products arachidonic acid , the vascular endothelium does not attract platelets, as it contains a large amount of prostacyclin. There is little prostacyclin under the endothelium, and when a defect forms in the endothelium, platelets, under the influence of thromboxane, begin to adhere to the vessel wall. Prostacyclin is not formed in atherosclerotic plaques, which explains the increased adhesion of platelets in these areas of the vessels.
Now it becomes clear what needs to be done to reduce platelet adhesion and, thereby, reduce the risk of thrombosis. It is necessary to shift the balance of thromboxane - prostacyclin towards the latter, either inhibiting the formation of thromboxane, or stimulating the production of prostacyclin. Medicines that act in this way are called antiplatelet agents, since they reduce the ability of platelets to adhere to the walls of blood vessels and unite (aggregate).
What is the connection between the Eskimo diet and myocardial infarction? In Eskimos, the incidence of myocardial infarction is low, and this is directly related to the nature of their diet. The fact is that the body of animals living in cold waters contains many polyunsaturated fatty acids, in particular eicosapentaenoic acid, which helps them survive in the difficult conditions of the North. The consumption of fat from these animals by Eskimos helps to reduce the content of arachidonic acid and increase the content of eicosapentaenoic acid in platelets. Eicosapentaenoic acid is converted in platelets into the inactive form of thromboxane, but in the endothelium it turns into active prostacyclin. Thus, the prerequisites are created for normal platelet circulation, and the likelihood of developing coronary heart disease, and therefore myocardial infarction, is reduced.
Antiplatelet properties are possessed by drugs of various pharmacological groups that block the synthesis of substances (in particular, thromboxane) that stimulate platelet adhesion. These drugs include, first of all, acetylsalicylic acid, dipyridamole, pentoxifylline And ticlopidine. Acetylsalicylic acid in small doses (50-125 mg) prevents the formation of thromboxane, but not prostacyclin. Therefore, it is used for the prevention of myocardial infarction and vascular complications in patients who have suffered a myocardial infarction. Dipyridamole acts on another link in the aggregation mechanism. It inhibits the enzyme phosphodiesterase, which, in turn, destroys substances in platelets that reduce adhesion. Pentoxifylline has similar properties, which, in addition, has a vasodilating effect. Differences in the mechanisms of action of acetylsalicylic acid and dipyridamole make it possible to use them together in the treatment of diseases of the cardiovascular system.
Ticlopidine inhibits platelet aggregation, preventing their binding to fibrinogen, but does not affect the adhesion mechanism. This same link in the aggregation mechanism is affected by abciximab- a new drug based on monoclonal antibodies.
Antiplatelet agents are used to prevent postoperative thrombosis , in complex treatment thrombophlebitis , cerebrovascular accidents , to prevent thromboembolic complications during coronary heart disease And myocardial infarction .
Hematopoiesis, or hematopoiesis, is the process of formation and development of blood cells. It compensates for the continuous destruction of formed elements. In the human body, the balance between the production of cellular blood elements and their destruction is maintained by a number of regulatory mechanisms, in particular hormones and vitamins. With a lack of iron and vitamin B 12 in the body ( cyanocobalamin)And folic acid, under the influence of ionizing radiation, with the use of chemotherapeutic agents, alcohol and in a number of pathological conditions, this balance shifts towards the destruction of blood cells, therefore, under these conditions, stimulation of hematopoiesis is necessary.
Iron is primarily necessary for the formation of hemoglobin - an erythrocyte protein that performs the most important function - the transfer of oxygen from the lungs to other tissues. After the destruction of red blood cells, the released iron is again used in the synthesis of hemoglobin. Vitamin B 12 and folic acid are involved in the construction of DNA, without which there will be neither normal division nor maturation of blood cells. A lack of these substances or a violation of their absorption and metabolism in the body leads to the development of anemia ( anemia ) - a condition characterized by a decrease in hemoglobin content in the blood, usually with a simultaneous decrease in the number of red blood cells.
The amount of iron in the body is 2-6 g (for men 50 mg/kg, for women - 35 mg/kg). About 2/3 of the total iron supply is part of hemoglobin, the remaining 1/3 is “stored” in the bone marrow, spleen and muscles.
The body of a healthy person absorbs 1-4 mg of iron from food per day. Its daily loss does not exceed 0.5-1 mg. However, during menstruation, a woman loses about 30 mg of iron, so its balance becomes negative. Additional iron intake (approximately 2.5 mg per day) is also required for pregnant women, taking into account the need for it in the developing fetus, the process of placenta formation and blood loss during childbirth.
Iron supplements are indicated for the treatment and prevention of iron deficiency anemia, which can occur due to blood loss, in women during pregnancy and lactation, in premature infants and in children during periods of intensive growth. These preparations contain both inorganic and organic iron compounds. It is still unclear which of these drugs is more effective, so there is no point in using more expensive drugs if there are no serious side effects when taking cheaper ones. Typically, in therapeutic doses (100-200 mg of elemental iron per day), side effects are minimal and manifest themselves in the form of dysfunction of the gastrointestinal tract. However, in case of overdose, they can cause severe irritation of the gastrointestinal tract. There are even cases of death from taking large numbers of iron sulfate tablets. Ascorbic and succinic acids increase the absorption of iron, which should be taken into account when taken together. At the same time, the introduction of these acids into the drug makes it possible to reduce the dosage of iron and reduce the frequency of gastrointestinal disorders. Dosage forms that slowly release iron are more gentle on the gastrointestinal tract. If iron absorption is impaired, its preparations are administered bypassing the digestive tract ( parenterally ), for example intravenously.
Vitamin B 12 is synthesized by microorganisms in the gastrointestinal tract or supplied with food. The normal need for this vitamin is only 2 mcg per day (approximately 3000-5000 mcg is stored in the liver of an adult), and deficiency occurs primarily when the absorption of this vitamin in the body is impaired. This deficiency, as well as a lack of folic acid, leads to severe anemia, as well as a decrease in the formation of leukocytes and platelets, disorders of the gastrointestinal tract, and can cause neurological disorders.
Folic acid owes its name to the leaves (folium - leaf) of spinach, where it was first discovered. This acid belongs to the B vitamins and, in addition to green plants, is found in yeast and animal liver. Folic acid itself is inert, but is activated in the body and participates in the synthesis of RNA and DNA. The reserves of folic acid in the body are low, and the need for it is high (50-200 mcg, and in pregnant women up to 300-400 mcg per day), so nutrition cannot always compensate for its consumption in the body. In these cases, medications containing folic acid are used.
The development, differentiation and reproduction of blood cells in the bone marrow - the main organ of the hematopoietic system - is regulated by hormones erythropoietin And colony-stimulating factors . The first of them was isolated, studied and obtained by genetic engineering as a drug, erythropoietin. This hormone is released in the kidneys when oxygen enters the tissues in insufficient quantities and stimulates the formation of red blood cells. For certain forms of anemia, erythropoietin preparations are very useful.
Colony-stimulating factors are also produced using genetic engineering methods, and their action is specific to certain types of blood cells. Drugs based on them are used in chemotherapy that suppresses the bone marrow, after bone marrow transplantation , at malignant bone marrow diseases And congenital hematopoietic disorders .
Drugs affecting hematopoiesis:
1.Medicines that stimulate erythropoiesis.
2. Medicines that stimulate leukopoiesis.
Drugs that affect blood clotting processes:
1. Anticoagulants:
Anticoagulants of direct and indirect action.
Fibrinolytics (thrombolytics).
Antiplatelet agents.
2. Drugs that increase blood clotting:
Coagulants of direct and indirect action.
Agents that inhibit fibrinolysis. Fibrinolysis inhibitors.
Stimulators of platelet aggregation.
Angioprotectors. Agents that reduce vascular permeability.
Medicinal plants with hemostatic effect.
Plasma replacement agents by functional purpose:
Detoxification solutions.
Solutions with hemodynamic effect.
Solutions regulating water-salt balance.
Solutions for parenteral nutrition.
Antiplatelet agents inhibit the aggregation of platelets and erythrocytes, reduce their ability to bond and adhere (adhesion) to the endothelium of blood vessels. By reducing the surface tension of red blood cell membranes, they facilitate their deformation when passing through capillaries and improve blood fluidity. Antiplatelet agents can not only prevent aggregation, but also cause disaggregation of already aggregated blood platelets.
Cyclooxygenase inhibitors (nonsteroidal anti-inflammatory drugs: acetylsalicylic acid, indomethacin, sulfinpyrazone, brufen, ketasone, naproxen, etc.).
Inhibitors of cAMP phosphodiesterase and adenylate cyclase (dipyridamole, ticlopidine, recornal, pentoxifylline). Antioxidants: ionol, bioquinol, etc.
Selective thromboxane synthetase inhibitors (imidazole derivatives).
Stimulators of prostacyclin synthesis (pyrazoline derivatives; pentoxifylline; calcitonin; angiotensin II; coumarin and nicotinic acid derivatives).
Ca++ antagonists (verapamil, nifedipine, diltiazem).
Prostanoids (prostacyclin, including synthetic analogs, prostaglandins E2 and D2).
Inhibitors of the release of platelet components (vasoactive drugs: suloctidil, piracetam).
Anticoagulants. Recently, it has been generally accepted that two natural anticoagulants with direct antithrombotic activity constantly circulate in the blood: heparin and antithrombin III. Heparin alone has an antithrombotic effect only in large doses, which are not usually used in the clinic. Under normal conditions, heparin, forming a complex with antithrombin III, converts it into its active form. Antithrombin III is able to quickly bind thrombin in the blood. The thrombin-antithrombin III complex is inactive in coagulation terms and is quickly eliminated from the bloodstream. Without heparin, antithrombin III can only very slowly inactivate thrombin in the blood. In addition to its main property of binding thrombin, activated antithrombin III blocks the conversion of factors XII, XI, II and fibrinolytic enzymes into the active form.
It is obvious that the pharmacodynamic activity of heparin is largely related to the level of antithrombin III in the blood, which can be reduced in some conditions. This makes it necessary in some cases to adjust the dose of heparin by determining the content of antithrombin III in the blood, and even combine it with antithrombin III drugs.
When complex compounds of heparin are formed with other biologically active substances (hormones, peptides, etc.), non-enzymatic (plasmin-independent) fibrin breakdown is possible. Along with hypocoagulative properties, heparin increases pulmonary ventilation, blocks a number of enzymes, inhibits inflammation, increases coronary blood flow, and activates lipoprotein lipase. T1/2 of heparin is 1-2 1/2 hours.
After intravenous administration, heparin is rapidly distributed into tissues. It is partially destroyed by heparinase, and some is excreted unchanged in the urine. Its maximum content in the blood after intravenous or intramuscular administration is achieved after 15-30 minutes, the therapeutic concentration remains for 2-6 hours and depends on the dose of the drug. The most prolonged hypocoagulation effect is observed with subcutaneous administration of the drug.
The pharmacokinetics of antithrombin III has not been sufficiently studied. To maintain the concentration in the blood, the drug, depending on the purpose (prevention or treatment), is administered, respectively, from 1 to 4-6 times a day intravenously or subcutaneously.
Indirect anticoagulants are mainly represented by coumarin derivatives. These drugs are antagonists of vitamin K, which is necessary for the synthesis of coagulation factors in the liver (factor II, V, VII, VIII, IX, etc.). Coumarin drugs in therapeutic doses do not affect platelet function, although some drugs affect the synthesis of prostaglandins in the vascular wall. With long-term use, they somewhat increase the fibrinolytic activity of the blood and can increase vascular permeability. T1/2 of coumarins - about 2 days.
The bioavailability of coumarin drugs is good: 80% of them are absorbed in the gastrointestinal tract. The maximum effect of coumarins usually occurs after 36-48 hours; the drugs are metabolized in the liver and, in the form of coumarin derivatives, are excreted in the urine and partly in the feces. The pharmacokinetics of coumarin derivatives changes in patients with liver and kidney damage. Coumarin derivatives displace pyrazolones from their binding to protein and interfere with the metabolism of a number of drugs.
Fibrinolytics, or fibrinolytic agents, cause the destruction of the formed fibrin threads; they contribute mainly to the resorption of fresh (not yet organized) blood clots.
Fibrinolytic agents are divided into groups of direct and indirect action. The first group includes substances that directly affect the blood plasma, a clot of fibrin strands, effective in vitro and in vivo (fibrinolysin, or plasmin, is an enzyme formed when the profibrinolysin contained in the blood is activated).
The second group includes enzymes that are activators of profibrinolysin (alteplase, streptokinase, etc.). They are inactive when directly acting on fibrin filaments, but when introduced into the body they activate the endogenous fibrinolytic system of the blood (convert profibrinolysin into fibrinolysin). Currently, the main use as fibrinolytic agents are drugs related to indirect fibrinolytics.
Rp.: Tab. Clopidogreli 0.075
D.t.d.N. thirty
S. Take 1 tablet orally 1 time per day.
Medicines affecting the blood system, classification. Pharmacological characteristics of aggregates, coagulants, fibrinolysis inhibitors. Recipe for aminocaproic acid.
Related information.
Drugs affecting the blood system. Influencing hematopoiesis 1) drugs affecting erythropoiesis (this is one of the types of the process of hematopoiesis (hematopoiesis), during which red blood cells (erythrocytes) are formed). Stimulating erythropoiesis: Inhibiting erythroesis (Drug: radioactive phosphorus. Prescribed for erythremia (excess of red blood cells). The disease is extremely rare in malignant lesions of the bone marrow. 2) drugs affecting leukopoiesis (the formation of leukocytes; usually occurs in the hematopoietic tissue of the bone marrow). Stimulating leukopoiesis Inhibiting leukopoiesis Affecting coagulation
 Drugs that stimulate erythropoiesis v Drugs used for hypochromic anemia For iron deficiency anemia (Iron preparations, Cobalt drugs) For non-iron deficiency anemia v Drugs used for hyperchromic anemia
Drugs that stimulate erythropoiesis v Drugs used for hypochromic anemia For iron deficiency anemia (Iron preparations, Cobalt drugs) For non-iron deficiency anemia v Drugs used for hyperchromic anemia
 Drugs that stimulate erythropoiesis Drugs in this group are used to treat anemia. Red blood cells mature in the bone marrow, enter the blood, perform their functions, after which they die and are replaced by new ones. A lack of red blood cells in the blood leads to anemia. Causes of anemia: iron deficiency. suppression of bone marrow function, intense destruction of red blood cells, massive bleeding
Drugs that stimulate erythropoiesis Drugs in this group are used to treat anemia. Red blood cells mature in the bone marrow, enter the blood, perform their functions, after which they die and are replaced by new ones. A lack of red blood cells in the blood leads to anemia. Causes of anemia: iron deficiency. suppression of bone marrow function, intense destruction of red blood cells, massive bleeding
 Iron deficiency anemia Accounts for 80% of all anemias. Fe deficiency in the body can occur in the following cases: - insufficient dietary intake (meat, fish, leafy vegetables, apples, citrus fruits, tomatoes, bananas) - impaired absorption in the intestines (inflammation of the mucous membrane, milk, Ca salts, phosphates, tetracyclines, lack of protein food) - increased need (children during the period of intensive growth # for small children and infants is 3-5 times higher than for men # pregnancy, lactation, menstruation, donors, chronic bleeding).
Iron deficiency anemia Accounts for 80% of all anemias. Fe deficiency in the body can occur in the following cases: - insufficient dietary intake (meat, fish, leafy vegetables, apples, citrus fruits, tomatoes, bananas) - impaired absorption in the intestines (inflammation of the mucous membrane, milk, Ca salts, phosphates, tetracyclines, lack of protein food) - increased need (children during the period of intensive growth # for small children and infants is 3-5 times higher than for men # pregnancy, lactation, menstruation, donors, chronic bleeding).
 Medicines used for iron deficiency anemia ü Preparations of 2-valent iron (used only internally) iron sulfate tardiferon (retard tablets), “feroplex” (with vitamin C), “ferrogard-C” (with vitamin C), actiferrin. The bulk of iron preparations. Highest bioavailability. Lowest toxicity. iron ferrous lactate Ferramide (rarely used, high toxicity, many adverse reactions) iron gluconate Totema (4th place in toxicity) iron fumarate Ferronate (2nd place in toxicity) iron protein succinate Ferlatum (3rd place in toxicity)
Medicines used for iron deficiency anemia ü Preparations of 2-valent iron (used only internally) iron sulfate tardiferon (retard tablets), “feroplex” (with vitamin C), “ferrogard-C” (with vitamin C), actiferrin. The bulk of iron preparations. Highest bioavailability. Lowest toxicity. iron ferrous lactate Ferramide (rarely used, high toxicity, many adverse reactions) iron gluconate Totema (4th place in toxicity) iron fumarate Ferronate (2nd place in toxicity) iron protein succinate Ferlatum (3rd place in toxicity)
 Medicines used for iron deficiency anemia ü Trivalent iron preparations (used orally and parenterally) For parenteral administration Ferrum-lek for IM (only) iron complex with maltose Maltofer (For oral administration)
Medicines used for iron deficiency anemia ü Trivalent iron preparations (used orally and parenterally) For parenteral administration Ferrum-lek for IM (only) iron complex with maltose Maltofer (For oral administration)
 Oral agents. Preference is given to 1) long-acting drugs, since they have less Pb. D 2) combination products, which in addition to Fe include a) vitamins (Vit. C, Vit. Gr. B), b) Cu, Mn, CO, Mg, Zn c) organic acids and other organic compounds that improve the absorption of Fe . Simple Fe salts cause irritation of the gastrointestinal mucosa. Modern preparations containing Fe in the form of organic complexes have higher bioavailability and do not have these disadvantages.
Oral agents. Preference is given to 1) long-acting drugs, since they have less Pb. D 2) combination products, which in addition to Fe include a) vitamins (Vit. C, Vit. Gr. B), b) Cu, Mn, CO, Mg, Zn c) organic acids and other organic compounds that improve the absorption of Fe . Simple Fe salts cause irritation of the gastrointestinal mucosa. Modern preparations containing Fe in the form of organic complexes have higher bioavailability and do not have these disadvantages.
 Oral agents. Inorganic Fe salts without additives Actiferrin – capsules, drops, syrup Ferro-gradument – tablet Tardiferon – tablet. Hemofer prolangatum – tablets Hemofer – drops
Oral agents. Inorganic Fe salts without additives Actiferrin – capsules, drops, syrup Ferro-gradument – tablet Tardiferon – tablet. Hemofer prolangatum – tablets Hemofer – drops
 Oral agents. Fe in the form of organic salts and complexes Sorbifer Durules (ascorbic acid) Ferroplex (ascorbic acid), Dragee gyno-tardiferon (folic acid), Ferritab Comb tablets (folic acid), Actifferin compositum tablets (folic acid), Ferlatum capsules (Iron protein succinylate) solution for oral administration Ferrum Lek (chew tablet, syrup) (iron (III) hydroxide polymaltosate) Containing vitamins Fenuls, Ferrofolgama, Ferro-vital. containing microelements of Totem - Cu, Mn - ampoules, solution inside.
Oral agents. Fe in the form of organic salts and complexes Sorbifer Durules (ascorbic acid) Ferroplex (ascorbic acid), Dragee gyno-tardiferon (folic acid), Ferritab Comb tablets (folic acid), Actifferin compositum tablets (folic acid), Ferlatum capsules (Iron protein succinylate) solution for oral administration Ferrum Lek (chew tablet, syrup) (iron (III) hydroxide polymaltosate) Containing vitamins Fenuls, Ferrofolgama, Ferro-vital. containing microelements of Totem - Cu, Mn - ampoules, solution inside.
 Oral agents. PC: - treatment of hidden Fe deficiency, - treatment of iron deficiency anemia, - prevention of iron deficiency during pregnancy, lactation, heavy menstruation, group B hypopolyvitaminosis, prolonged bleeding, malnutrition, etc. The minimum course of treatment is 1 month, the average course of treatment is 2 -3 months . It may take 3-6 months for the body to replenish its full iron supply (until the serum ferritin concentration, which reflects the body's Fe reserves, normalizes).
Oral agents. PC: - treatment of hidden Fe deficiency, - treatment of iron deficiency anemia, - prevention of iron deficiency during pregnancy, lactation, heavy menstruation, group B hypopolyvitaminosis, prolonged bleeding, malnutrition, etc. The minimum course of treatment is 1 month, the average course of treatment is 2 -3 months . It may take 3-6 months for the body to replenish its full iron supply (until the serum ferritin concentration, which reflects the body's Fe reserves, normalizes).
 Oral agents. Interaction with other drugs: Fe absorption is worsened by antacids, tetracyclines, adsorbents, Ca++ salts, hormonal contraceptives, carbamazepine. Solid foods, bread, cheese, cereals, dairy products, eggs, tea. Pb. D: Gastrointestinal tract - constipation, nausea, vomiting, diarrhea, pain in the epigastric region, sensations of fullness, distension, blackening of the stool (old drugs caused changes in tooth enamel, blackening of teeth), allergic reactions.
Oral agents. Interaction with other drugs: Fe absorption is worsened by antacids, tetracyclines, adsorbents, Ca++ salts, hormonal contraceptives, carbamazepine. Solid foods, bread, cheese, cereals, dairy products, eggs, tea. Pb. D: Gastrointestinal tract - constipation, nausea, vomiting, diarrhea, pain in the epigastric region, sensations of fullness, distension, blackening of the stool (old drugs caused changes in tooth enamel, blackening of teeth), allergic reactions.
 In severe forms of the disease, if it is necessary to quickly replenish the deficiency or impaired absorption of Fe in the gastrointestinal tract, drugs for parenteral management are used: FERRUM LEK – amp. (i.m.) VENOFER – i.v. (slow stream or drip) FERKOVEN (old drug). Parenteral drugs are administered in the clinic under supervision. Pb. D: phlebitis, chest pain, hypotension, allergic reactions, etc.
In severe forms of the disease, if it is necessary to quickly replenish the deficiency or impaired absorption of Fe in the gastrointestinal tract, drugs for parenteral management are used: FERRUM LEK – amp. (i.m.) VENOFER – i.v. (slow stream or drip) FERKOVEN (old drug). Parenteral drugs are administered in the clinic under supervision. Pb. D: phlebitis, chest pain, hypotension, allergic reactions, etc.
 Medicines used for hypochromic anemia Cobalt preparations Coamide (anemia in chronic renal failure) Medicines used for hypochromic anemia (without iron deficiency) Erythropoiesis stimulants - human recombinant erythropoietin (for anemia associated with chronic renal failure, rheumatoid arthritis, malignant tumors, AIDS , with anemia in premature babies.
Medicines used for hypochromic anemia Cobalt preparations Coamide (anemia in chronic renal failure) Medicines used for hypochromic anemia (without iron deficiency) Erythropoiesis stimulants - human recombinant erythropoietin (for anemia associated with chronic renal failure, rheumatoid arthritis, malignant tumors, AIDS , with anemia in premature babies.
 Medicines used for hyperchromic anemia B 12 (cyanocobalamin) – Absent in plant foods. Contained in meat and dairy foods. The depot of vitamins B 12 is the liver (with proper nutrition, the reserve in the liver of B 12 is for 5 years, s/p - 2 mcg, reserve 3000 -5000 mcg). For the absorption of B 12 into the blood, an “intrinsic factor” is required - a glycoprotein that is produced by the gastric mucosa and ensures the absorption of B 12 in the small intestine. Various diseases of the gastrointestinal tract (dysfunction of the mucous membrane), worms (wide tapeworm), vegetarianism, etc. → loss of “internal factor” → deficiency of vitamin B 12.
Medicines used for hyperchromic anemia B 12 (cyanocobalamin) – Absent in plant foods. Contained in meat and dairy foods. The depot of vitamins B 12 is the liver (with proper nutrition, the reserve in the liver of B 12 is for 5 years, s/p - 2 mcg, reserve 3000 -5000 mcg). For the absorption of B 12 into the blood, an “intrinsic factor” is required - a glycoprotein that is produced by the gastric mucosa and ensures the absorption of B 12 in the small intestine. Various diseases of the gastrointestinal tract (dysfunction of the mucous membrane), worms (wide tapeworm), vegetarianism, etc. → loss of “internal factor” → deficiency of vitamin B 12.
 Deficiency of B 12: a) ↓ hematopoiesis (erythrocytes + leukocytes + platelets); b) neurological disorders (the formation of the myelin sheath of nerve fibers is disrupted) c) atrophic changes in the mucous membrane of the gastrointestinal tract (tongue) B 12, obtained synthetically, is poorly absorbed from the gastrointestinal tract. First administered intramuscularly in large doses to restore reserves in the liver, then maintenance therapy (once a month, if necessary, for life). Folic acid improves the absorption of B 12 Pb. D: very rare: allergic reactions, tachycardia, nervous excitement. PC: a) megaloblastic anemia, b) diseases of the liver and nervous system. F.v. Cyanocobolamine – amp. 1 ml each,
Deficiency of B 12: a) ↓ hematopoiesis (erythrocytes + leukocytes + platelets); b) neurological disorders (the formation of the myelin sheath of nerve fibers is disrupted) c) atrophic changes in the mucous membrane of the gastrointestinal tract (tongue) B 12, obtained synthetically, is poorly absorbed from the gastrointestinal tract. First administered intramuscularly in large doses to restore reserves in the liver, then maintenance therapy (once a month, if necessary, for life). Folic acid improves the absorption of B 12 Pb. D: very rare: allergic reactions, tachycardia, nervous excitement. PC: a) megaloblastic anemia, b) diseases of the liver and nervous system. F.v. Cyanocobolamine – amp. 1 ml each,

 Medicines used for hyperchromic anemia Folic acid (Fc) - isolated from spinach leaves in 1941 (leafy vegetables, liver, eggs, buckwheat and oatmeal) F. reserves in the body are not large (for 3 - 5 months), but the need is high (50 - 200 mcg/day, pregnant women 300 -400 mcg/day; protection against teratogenic factors), so poor nutrition cannot always compensate for the consumption. F. deficiency may be associated with the use of antitumor drugs—antimetabolites. F. k.: well absorbed in the duodenum and 65% bound to proteins. Metabolizes in the liver, excreted by the kidneys, partly with feces. Pb. D: toxicity is very low. PK: a) for megablastic anemia, it is prescribed only together with B 12, since PK alone does not eliminate all symptoms (neuralgic) b) for macrocentral anemia, it is prescribed independently (in newborns, during pregnancy, gastrointestinal diseases, medications (anticonvulsants) ) c) iron deficiency anemia (improves Fe absorption)
Medicines used for hyperchromic anemia Folic acid (Fc) - isolated from spinach leaves in 1941 (leafy vegetables, liver, eggs, buckwheat and oatmeal) F. reserves in the body are not large (for 3 - 5 months), but the need is high (50 - 200 mcg/day, pregnant women 300 -400 mcg/day; protection against teratogenic factors), so poor nutrition cannot always compensate for the consumption. F. deficiency may be associated with the use of antitumor drugs—antimetabolites. F. k.: well absorbed in the duodenum and 65% bound to proteins. Metabolizes in the liver, excreted by the kidneys, partly with feces. Pb. D: toxicity is very low. PK: a) for megablastic anemia, it is prescribed only together with B 12, since PK alone does not eliminate all symptoms (neuralgic) b) for macrocentral anemia, it is prescribed independently (in newborns, during pregnancy, gastrointestinal diseases, medications (anticonvulsants) ) c) iron deficiency anemia (improves Fe absorption)
 It is well absorbed in the duodenum and is 65% protein bound. Metabolizes in the liver, excreted by the kidneys, partly with feces. Pb. D: toxicity is very low. PK: a) for megablastic anemia, it is prescribed only together with B 12, since PK alone does not eliminate all symptoms (neuralgic) b) for macrocentral anemia, it is prescribed independently (in newborns, during pregnancy, gastrointestinal diseases, medications (anticonvulsants) ) c) iron deficiency anemia (improves Fe absorption)
It is well absorbed in the duodenum and is 65% protein bound. Metabolizes in the liver, excreted by the kidneys, partly with feces. Pb. D: toxicity is very low. PK: a) for megablastic anemia, it is prescribed only together with B 12, since PK alone does not eliminate all symptoms (neuralgic) b) for macrocentral anemia, it is prescribed independently (in newborns, during pregnancy, gastrointestinal diseases, medications (anticonvulsants) ) c) iron deficiency anemia (improves Fe absorption)
 Agents that stimulate leukopoiesis. A decrease in the number of leukocytes in the blood is called leukopenia. Causes: - radiation sickness - autoimmune diseases - exposure to toxic substances (poisons) - drug-induced leukopenia (pyrazolone derivatives, antiepileptic drugs, chloramphenicol, cytostatics).
Agents that stimulate leukopoiesis. A decrease in the number of leukocytes in the blood is called leukopenia. Causes: - radiation sickness - autoimmune diseases - exposure to toxic substances (poisons) - drug-induced leukopenia (pyrazolone derivatives, antiepileptic drugs, chloramphenicol, cytostatics).
 Agents that stimulate leukopoiesis. The following can be used as leukopoiesis stimulants: A) non-steroidal anabolics Methyluracil and Pentoxyl. M.D.: accelerate the processes of cellular regeneration, wound healing, activates the immune system. Can be used for slow-healing wounds, fractures, burns, ulcers. Pentoxyl - tab. , has an immunostimulating effect → no local forms. Methyluracil - table. , ointment, suppositories x 4 times a day. Pb. D: headache, dizziness, allergies (rashes).
Agents that stimulate leukopoiesis. The following can be used as leukopoiesis stimulants: A) non-steroidal anabolics Methyluracil and Pentoxyl. M.D.: accelerate the processes of cellular regeneration, wound healing, activates the immune system. Can be used for slow-healing wounds, fractures, burns, ulcers. Pentoxyl - tab. , has an immunostimulating effect → no local forms. Methyluracil - table. , ointment, suppositories x 4 times a day. Pb. D: headache, dizziness, allergies (rashes).
 Agents that stimulate leukopoiesis. B) Sodium nucleospermate – a mixture of Na salts of nucleic acid derivatives (RNA, DNA). More purified and active than older drugs. Fur. actions: enhances the production of endogenous colony-stimulating factors (accelerates the formation of granulocytes at all stages, their number in the peripheral blood increases). F.v. : – amp. , fl. (i.m., s.c.) PC: treatment and prevention of leukopenia (decrease in the number of leukocytes per unit volume of blood) during radiation and chemotherapy. Pb. D: Body temperature for a short time (380), local hyperemia, pain.
Agents that stimulate leukopoiesis. B) Sodium nucleospermate – a mixture of Na salts of nucleic acid derivatives (RNA, DNA). More purified and active than older drugs. Fur. actions: enhances the production of endogenous colony-stimulating factors (accelerates the formation of granulocytes at all stages, their number in the peripheral blood increases). F.v. : – amp. , fl. (i.m., s.c.) PC: treatment and prevention of leukopenia (decrease in the number of leukocytes per unit volume of blood) during radiation and chemotherapy. Pb. D: Body temperature for a short time (380), local hyperemia, pain.
 Agents that stimulate leukopoiesis B) The most promising are recombinant preparations of colony-stimulating factors (CSF). CSF – tissue-specific hormones. They can be produced by bone marrow cells, vascular endothelium, T-lymphocytes, macrophages, etc. They control the differentiation of blood cells, their division and maturation.
Agents that stimulate leukopoiesis B) The most promising are recombinant preparations of colony-stimulating factors (CSF). CSF – tissue-specific hormones. They can be produced by bone marrow cells, vascular endothelium, T-lymphocytes, macrophages, etc. They control the differentiation of blood cells, their division and maturation.
 Drugs that stimulate leukopoiesis Medicines are obtained using genetic engineering. The structure of glycoproteins. Molgramostim (Leukomax) – bottle of 50 – 500 mcg. CSF granulocytes and monocytes (macrophages) Lenograstim (granocyte) CSF - granulocytes Filgrastim (Neupogen, Neipomax) 0.3 g per vial. (neutrophils) F.v. : bottles with lyophilized powder, i.v. , s.c. Pegfilgrastim (neulastim) is a conjugate of filgrastim with polyethylene glycol. It has a prolonged effect, since excretion through the kidneys slows down. Solution for subcutaneous injection, administration via syringe tube 0.6 ml. PC: inhibition of leukopoiesis due to chemotherapy, infection, bone marrow transplant, aplastic anemia (this is a group of diseases that arise due to suppression of bone marrow function, as a result of which it is not able to produce enough blood cells), HIV and other immunodeficiency. Pb. D: rarely allergies, liver, “bone pain”.
Drugs that stimulate leukopoiesis Medicines are obtained using genetic engineering. The structure of glycoproteins. Molgramostim (Leukomax) – bottle of 50 – 500 mcg. CSF granulocytes and monocytes (macrophages) Lenograstim (granocyte) CSF - granulocytes Filgrastim (Neupogen, Neipomax) 0.3 g per vial. (neutrophils) F.v. : bottles with lyophilized powder, i.v. , s.c. Pegfilgrastim (neulastim) is a conjugate of filgrastim with polyethylene glycol. It has a prolonged effect, since excretion through the kidneys slows down. Solution for subcutaneous injection, administration via syringe tube 0.6 ml. PC: inhibition of leukopoiesis due to chemotherapy, infection, bone marrow transplant, aplastic anemia (this is a group of diseases that arise due to suppression of bone marrow function, as a result of which it is not able to produce enough blood cells), HIV and other immunodeficiency. Pb. D: rarely allergies, liver, “bone pain”.
 Agents that inhibit hematopoiesis. Antitumor agents: myelosan, chlorobutin, procarbazine sodium phosphate. Leukemia is a malignant tumor; there are a lot of immature formed elements in the blood. Methotrexate, mercaptopurine, cytarabine. Rubomycin Vinblastine La asparaginase Glucocorticoids
Agents that inhibit hematopoiesis. Antitumor agents: myelosan, chlorobutin, procarbazine sodium phosphate. Leukemia is a malignant tumor; there are a lot of immature formed elements in the blood. Methotrexate, mercaptopurine, cytarabine. Rubomycin Vinblastine La asparaginase Glucocorticoids
 MEDICINES AFFECTING BLOOD CLOTTING Blood clotting (hemostasis) is a protective biological reaction in which a large number of coagulation factors found in blood plasma, formed elements and tissues take part. When bleeding, the blood vessels narrow, blood clotting is activated, a blood clot is formed, and the bleeding stops. Excessive thrombus formation does not occur, since along with the blood coagulation system, an anticoagulation system (fibrinolysis) functions in the body. When the activity of certain factors changes, the dynamic balance between them is disrupted, which leads to serious consequences: with an increase in blood clotting, thrombosis and embolism occur, and with a decrease, bleeding occurs.
MEDICINES AFFECTING BLOOD CLOTTING Blood clotting (hemostasis) is a protective biological reaction in which a large number of coagulation factors found in blood plasma, formed elements and tissues take part. When bleeding, the blood vessels narrow, blood clotting is activated, a blood clot is formed, and the bleeding stops. Excessive thrombus formation does not occur, since along with the blood coagulation system, an anticoagulation system (fibrinolysis) functions in the body. When the activity of certain factors changes, the dynamic balance between them is disrupted, which leads to serious consequences: with an increase in blood clotting, thrombosis and embolism occur, and with a decrease, bleeding occurs.
 Classification I. Drugs used for the prevention and treatment of thrombosis. 1. Antiplatelet agents (Aggregation - gluing of TCs to each other). 2. Anticoagulants (reduce clotting) 3. Fibrinolytics (medicines that destroy (dissolve) newly formed blood clots.) II. Drugs that help stop bleeding (increasing blood clotting) 1. Coagulants 2. Antifibritolytics
Classification I. Drugs used for the prevention and treatment of thrombosis. 1. Antiplatelet agents (Aggregation - gluing of TCs to each other). 2. Anticoagulants (reduce clotting) 3. Fibrinolytics (medicines that destroy (dissolve) newly formed blood clots.) II. Drugs that help stop bleeding (increasing blood clotting) 1. Coagulants 2. Antifibritolytics
 Drugs that reduce platelet aggregation (Antiplatelet agents) Aspirin - suppresses platelet aggregation, inhibits thromboxane synthesis. As an antiplatelet agent (acts in small doses as an antiplatelet agent - ¼ tablet in the morning after breakfast. (Thrombo - ass 50 mg, 100 mg, Aspirincardio, Thrombopol, Kardiask) Used orally to prevent thrombus formation in ischemic heart disease, after myocardial infarction, in case of cerebrovascular accident, thrombophlebitis.
Drugs that reduce platelet aggregation (Antiplatelet agents) Aspirin - suppresses platelet aggregation, inhibits thromboxane synthesis. As an antiplatelet agent (acts in small doses as an antiplatelet agent - ¼ tablet in the morning after breakfast. (Thrombo - ass 50 mg, 100 mg, Aspirincardio, Thrombopol, Kardiask) Used orally to prevent thrombus formation in ischemic heart disease, after myocardial infarction, in case of cerebrovascular accident, thrombophlebitis.
 Agents that reduce platelet aggregation (Antiplatelet agents) Dipyridamole (Curantil) Most often used for the prevention of thrombosis in atherosclerosis of the cerebral, coronary and peripheral vessels. Clopidogrel (Plavix) tab. 75 mg 1 time / day Prevention of thrombotic complications in patients with myocardial infarction, ischemic stroke
Agents that reduce platelet aggregation (Antiplatelet agents) Dipyridamole (Curantil) Most often used for the prevention of thrombosis in atherosclerosis of the cerebral, coronary and peripheral vessels. Clopidogrel (Plavix) tab. 75 mg 1 time / day Prevention of thrombotic complications in patients with myocardial infarction, ischemic stroke
 Drugs that reduce blood clotting (Anticoagulants) Direct anticoagulants Affect factors located directly in the blood. The effect develops very quickly and manifests itself both in the body and in vitro (in vivo, in vitro). Heparin is a natural blood clotting factor. In the body it is predominantly produced by mast cells (connective tissue) and basophils. Carries a strong “-” charge. Due to this, it binds to proteins that are blood clotting factors.
Drugs that reduce blood clotting (Anticoagulants) Direct anticoagulants Affect factors located directly in the blood. The effect develops very quickly and manifests itself both in the body and in vitro (in vivo, in vitro). Heparin is a natural blood clotting factor. In the body it is predominantly produced by mast cells (connective tissue) and basophils. Carries a strong “-” charge. Due to this, it binds to proteins that are blood clotting factors.
 Drugs that reduce blood clotting (Anticoagulants) In the Heparin molecule, only 1/3 has anticoagulant properties, the rest is ballast, therefore, an allergy. The drugs "Fraxiparin" and "Enoxaparin" are low-molecular fractions of g., which contain more active part and less ballast. - When administered intravenously, the effect occurs immediately and lasts up to 810 hours; - Drip, intramuscular, subcutaneous. Dosed in units. PC: - thrombosis of coronary vessels; - prevention of thrombosis and thromboembolitis during operations (CVS, orthopedics, etc.); hemodialysis, artificial circulation; thrombophlebitis of superficial veins. Pb. D: - hemorrhages (s/c, nasal, gastric, intramuscular): - allergies.
Drugs that reduce blood clotting (Anticoagulants) In the Heparin molecule, only 1/3 has anticoagulant properties, the rest is ballast, therefore, an allergy. The drugs "Fraxiparin" and "Enoxaparin" are low-molecular fractions of g., which contain more active part and less ballast. - When administered intravenously, the effect occurs immediately and lasts up to 810 hours; - Drip, intramuscular, subcutaneous. Dosed in units. PC: - thrombosis of coronary vessels; - prevention of thrombosis and thromboembolitis during operations (CVS, orthopedics, etc.); hemodialysis, artificial circulation; thrombophlebitis of superficial veins. Pb. D: - hemorrhages (s/c, nasal, gastric, intramuscular): - allergies.
 Complex preparations with Heparin: “Hepatrombin” ointment, gel, “Lioton” - gel; "Gepatrombin G." ointment, rectal suppositories
Complex preparations with Heparin: “Hepatrombin” ointment, gel, “Lioton” - gel; "Gepatrombin G." ointment, rectal suppositories
 Anticoagulants (Anticoagulants) Sodium citrate PC: blood preservation (Only!) (4 -5% solution). Introduction into the body can lead to undesirable consequences (inhibition of other Ca-dependent processes). Gerudin (gerudotherapy) is an enzyme in leech saliva that inhibits thrombin.
Anticoagulants (Anticoagulants) Sodium citrate PC: blood preservation (Only!) (4 -5% solution). Introduction into the body can lead to undesirable consequences (inhibition of other Ca-dependent processes). Gerudin (gerudotherapy) is an enzyme in leech saliva that inhibits thrombin.
 Drugs that reduce blood clotting (Anticoagulants) indirect anticoagulants. They are antagonists of vitamin K. Coumarin derivatives. In nature, coumarin in the form of sugars is found in many plants (aster, sweet clover, bison). In its isolated form, these are crystals that smell like fresh hay. Its derivative (dicoumarin) was isolated in 1940 from rotting sweet clover and was first used to treat thrombosis. This discovery of pharmacists was prompted by veterinarians who, in the 20s of the last century, discovered that cows in the USA and Canada, grazing in meadows overgrown with clover, began to die from massive bleeding. After this, dicoumarin was used for some time as a rat poison, and later began to be used as an anti-clotting drug. Subsequently, dicoumarin was replaced from pharmaceuticals by neodicoumarin and warfarin. List of drugs: Warfarin (Warfarex, Marevan, Warfarin sodium), Neodicoumarin (Ethylbiscoumacetate), Acenocoumarol (Sincumar).
Drugs that reduce blood clotting (Anticoagulants) indirect anticoagulants. They are antagonists of vitamin K. Coumarin derivatives. In nature, coumarin in the form of sugars is found in many plants (aster, sweet clover, bison). In its isolated form, these are crystals that smell like fresh hay. Its derivative (dicoumarin) was isolated in 1940 from rotting sweet clover and was first used to treat thrombosis. This discovery of pharmacists was prompted by veterinarians who, in the 20s of the last century, discovered that cows in the USA and Canada, grazing in meadows overgrown with clover, began to die from massive bleeding. After this, dicoumarin was used for some time as a rat poison, and later began to be used as an anti-clotting drug. Subsequently, dicoumarin was replaced from pharmaceuticals by neodicoumarin and warfarin. List of drugs: Warfarin (Warfarex, Marevan, Warfarin sodium), Neodicoumarin (Ethylbiscoumacetate), Acenocoumarol (Sincumar).
 The most popular indirect anticoagulant today is Wafarin Warfarin, under various commercial names, is available in tablets of 2, 5, 3 and 5 mg. If you start taking the tablets, they will begin to act after 36-72 hours, and the maximum therapeutic effect will appear by 5-7 days from the start of treatment. If the drug is discontinued, normal functioning of the blood coagulation system will return after 5 days. Indications for prescribing warfarin are most often all typical cases of thrombosis and thromboembolism. Side effects Among the side effects of warfarin are bleeding, nausea and vomiting, diarrhea, abdominal pain, skin reactions (urticaria, itching, eczema, necrosis, vasculitis, nephritis, urolithiasis, hair loss).
The most popular indirect anticoagulant today is Wafarin Warfarin, under various commercial names, is available in tablets of 2, 5, 3 and 5 mg. If you start taking the tablets, they will begin to act after 36-72 hours, and the maximum therapeutic effect will appear by 5-7 days from the start of treatment. If the drug is discontinued, normal functioning of the blood coagulation system will return after 5 days. Indications for prescribing warfarin are most often all typical cases of thrombosis and thromboembolism. Side effects Among the side effects of warfarin are bleeding, nausea and vomiting, diarrhea, abdominal pain, skin reactions (urticaria, itching, eczema, necrosis, vasculitis, nephritis, urolithiasis, hair loss).
 Warfarin There is a whole list of foods that should be consumed with caution or completely excluded during treatment with warfarin, as they increase bleeding and increase the risk of bleeding. These are garlic, sage and quinine contained in tonics, papaya, avocado, onions, cabbage, broccoli and Brussels sprouts, cucumber peel, lettuce and watercress, kiwi, mint, spinach, parsley, peas, soybeans, watercress, turnips , olive oil, peas, cilantro, pistachios, chicory. Alcohol also increases the risk of bleeding. It should be remembered that independent initiation of use and selection of doses of Warfarin are strictly prohibited, due to the high risks of bleeding and strokes. Only a doctor who can competently assess the clinical situation and risks can prescribe anticoagulants and titrate doses.
Warfarin There is a whole list of foods that should be consumed with caution or completely excluded during treatment with warfarin, as they increase bleeding and increase the risk of bleeding. These are garlic, sage and quinine contained in tonics, papaya, avocado, onions, cabbage, broccoli and Brussels sprouts, cucumber peel, lettuce and watercress, kiwi, mint, spinach, parsley, peas, soybeans, watercress, turnips , olive oil, peas, cilantro, pistachios, chicory. Alcohol also increases the risk of bleeding. It should be remembered that independent initiation of use and selection of doses of Warfarin are strictly prohibited, due to the high risks of bleeding and strokes. Only a doctor who can competently assess the clinical situation and risks can prescribe anticoagulants and titrate doses.
 Fibrinolytics (thrombolytics) Fibrinolysis activators are used to dissolve fresh blood clots and emboli as first aid agents. Fibrinolysis is the dissolution of fibrin filaments. Fibrinolysin can be used to stimulate fibrinolysis. Fibrinolysin, having a large molecular weight, does not penetrate deep into the thrombus, acts only on fresh, loose fibrin clots before their retraction and, like any protein, causes the formation of antibodies, and allergic reactions often occur to it. Fv: lyophilisate for preparing a solution for infusion Indications: thromboembolism of the pulmonary artery, cerebral vessels, myocardial infarction, acute thrombophlebitis.
Fibrinolytics (thrombolytics) Fibrinolysis activators are used to dissolve fresh blood clots and emboli as first aid agents. Fibrinolysis is the dissolution of fibrin filaments. Fibrinolysin can be used to stimulate fibrinolysis. Fibrinolysin, having a large molecular weight, does not penetrate deep into the thrombus, acts only on fresh, loose fibrin clots before their retraction and, like any protein, causes the formation of antibodies, and allergic reactions often occur to it. Fv: lyophilisate for preparing a solution for infusion Indications: thromboembolism of the pulmonary artery, cerebral vessels, myocardial infarction, acute thrombophlebitis.
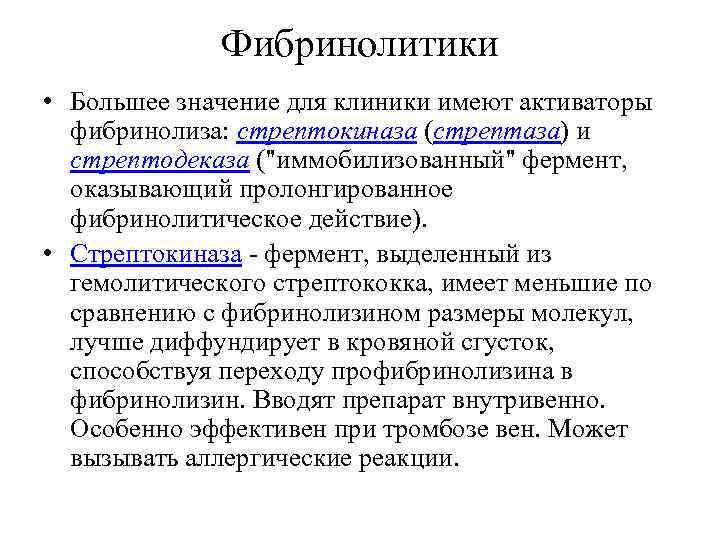 Fibrinolytics Activators of fibrinolysis are of greater clinical importance: streptokinase (streptase) and streptodecase (an “immobilized” enzyme that has a prolonged fibrinolytic effect). Streptokinase, an enzyme isolated from hemolytic streptococcus, has smaller molecular sizes compared to fibrinolysin and diffuses better into the blood clot, facilitating the transition of profibrinolysin to fibrinolysin. The drug is administered intravenously. Particularly effective for vein thrombosis. May cause allergic reactions.
Fibrinolytics Activators of fibrinolysis are of greater clinical importance: streptokinase (streptase) and streptodecase (an “immobilized” enzyme that has a prolonged fibrinolytic effect). Streptokinase, an enzyme isolated from hemolytic streptococcus, has smaller molecular sizes compared to fibrinolysin and diffuses better into the blood clot, facilitating the transition of profibrinolysin to fibrinolysin. The drug is administered intravenously. Particularly effective for vein thrombosis. May cause allergic reactions.
 Fibrinolytics An active and low-toxic fibrinolytic is urokinase, an enzyme produced in the kidneys and acting similarly to streptokinase. However, the difficulty of obtaining and the high cost of the drug limits the possibility of its use. Alteplase (Actilyse) Myocardial infarction (in the first 6–12 hours), acute massive pulmonary embolism.
Fibrinolytics An active and low-toxic fibrinolytic is urokinase, an enzyme produced in the kidneys and acting similarly to streptokinase. However, the difficulty of obtaining and the high cost of the drug limits the possibility of its use. Alteplase (Actilyse) Myocardial infarction (in the first 6–12 hours), acute massive pulmonary embolism.
 Coagulants are used to stop bleeding from small vessels (capillaries, arterioles). There are drugs of direct and indirect action, for local and resorptive use. By origin: a) natural blood clotting factors, b) synthetic, c) herbal agents
Coagulants are used to stop bleeding from small vessels (capillaries, arterioles). There are drugs of direct and indirect action, for local and resorptive use. By origin: a) natural blood clotting factors, b) synthetic, c) herbal agents
 Vikasol is a synthetic water-soluble analogue of vitamin K 3. Vitamin K is involved in the synthesis of various blood coagulation factors in the liver (I, II, VII, IX, X). Obtained from food (bile), synthesized in the intestines. The effect of the drug develops after 12-18 hours, maximum after 24 hours or more. PC: bleeding associated with a lack of prothrombin, with hepatitis, peptic ulcer, after surgery, hemorrhoids, parenchymal bleeding, etc. F.V. - table. , amp.
Vikasol is a synthetic water-soluble analogue of vitamin K 3. Vitamin K is involved in the synthesis of various blood coagulation factors in the liver (I, II, VII, IX, X). Obtained from food (bile), synthesized in the intestines. The effect of the drug develops after 12-18 hours, maximum after 24 hours or more. PC: bleeding associated with a lack of prothrombin, with hepatitis, peptic ulcer, after surgery, hemorrhoids, parenchymal bleeding, etc. F.V. - table. , amp.
 Natural blood clotting factors Fibrinogen - obtained from donor blood plasma, F.V. sterile powder in vials; IV, drip. PC: bleeding associated with a lack of fibrinogen in the body, in surgical practice, obstetrics and gynecology, traumatology. There are local dosage forms with fibrinogen (fibrin isogenic film, sponge).
Natural blood clotting factors Fibrinogen - obtained from donor blood plasma, F.V. sterile powder in vials; IV, drip. PC: bleeding associated with a lack of fibrinogen in the body, in surgical practice, obstetrics and gynecology, traumatology. There are local dosage forms with fibrinogen (fibrin isogenic film, sponge).
 Natural blood clotting factors Thrombin - obtained in powder form from blood plasma. Has a powerful and fast effect. Systemic use is unacceptable as it causes widespread thrombosis. Apply only topically! Swabs and napkins are moistened with the prepared solution. A hemostatic sponge can be used locally to stop bleeding.
Natural blood clotting factors Thrombin - obtained in powder form from blood plasma. Has a powerful and fast effect. Systemic use is unacceptable as it causes widespread thrombosis. Apply only topically! Swabs and napkins are moistened with the prepared solution. A hemostatic sponge can be used locally to stop bleeding.
 Herbal products are most often used in gynecological practice in the form of infusions 10: 200 ml, 1 tbsp. spoon, in the form of tinctures and liquid extracts, 30-50 drops; prescribed orally before meals 3-4 times a day. Can be used for hemorrhagic diathesis, hemorrhoidal, nasal and other bleeding. Nettle leaves Yarrow herb Water pepper herb - liquid extract Knotweed herb - infusion Arnica flowers - tincture. Viburnum bark - extract, decoction.
Herbal products are most often used in gynecological practice in the form of infusions 10: 200 ml, 1 tbsp. spoon, in the form of tinctures and liquid extracts, 30-50 drops; prescribed orally before meals 3-4 times a day. Can be used for hemorrhagic diathesis, hemorrhoidal, nasal and other bleeding. Nettle leaves Yarrow herb Water pepper herb - liquid extract Knotweed herb - infusion Arnica flowers - tincture. Viburnum bark - extract, decoction.
 Antifibrinolytics In some pathological conditions, when the anticoagulant system prevails over the blood coagulation system (fibrinolysis is activated). Fibrinolysis must be suppressed. Drugs in this group stabilize fibrin and help stop bleeding.
Antifibrinolytics In some pathological conditions, when the anticoagulant system prevails over the blood coagulation system (fibrinolysis is activated). Fibrinolysis must be suppressed. Drugs in this group stabilize fibrin and help stop bleeding.
 Synthetic agents: Aminocaproic acid (ACA) Bleeding during surgical interventions on organs rich in fibrinolysis activators (lungs, thyroid gland, stomach, cervix, prostate gland). Diseases of internal organs with hemorrhagic syndrome; premature placental abruption, complicated abortion. Well absorbed from the gastrointestinal tract; inside, i.v. Pb. D; nausea, diarrhea, dizziness, drowsiness (low toxicity). Aminomethylbenzoic acid (AMBA) (AMBEN). Table , amp. Pb. D: + pressure fluctuations, increased heart rate. PC: local and generalized fibrinolytic bleeding (surgeries, trauma, gynecology, urology, ENT, dentistry, streptokinase overdose). Tranexamic acid (tranexam) Bleeding caused by increased general and local fibrinolysis (treatment and prevention): hemophilia, hemorrhagic complications of fibrinolytic therapy, thrombocytopenic purpura, aplastic anemia, leukemia, bleeding during surgery and in the postoperative period, uterine during childbirth, pulmonary, nasal , gastrointestinal
Synthetic agents: Aminocaproic acid (ACA) Bleeding during surgical interventions on organs rich in fibrinolysis activators (lungs, thyroid gland, stomach, cervix, prostate gland). Diseases of internal organs with hemorrhagic syndrome; premature placental abruption, complicated abortion. Well absorbed from the gastrointestinal tract; inside, i.v. Pb. D; nausea, diarrhea, dizziness, drowsiness (low toxicity). Aminomethylbenzoic acid (AMBA) (AMBEN). Table , amp. Pb. D: + pressure fluctuations, increased heart rate. PC: local and generalized fibrinolytic bleeding (surgeries, trauma, gynecology, urology, ENT, dentistry, streptokinase overdose). Tranexamic acid (tranexam) Bleeding caused by increased general and local fibrinolysis (treatment and prevention): hemophilia, hemorrhagic complications of fibrinolytic therapy, thrombocytopenic purpura, aplastic anemia, leukemia, bleeding during surgery and in the postoperative period, uterine during childbirth, pulmonary, nasal , gastrointestinal
 Animal origin Antienzyme preparations (from tissues of slaughter cattle) - contrical trasylol, gordox Bleeding caused by hyperfibrinolysis, including after operations and injuries; before, during and after childbirth; hemorrhagic complications arising during thrombolytic therapy, acute pancreatitis, prevention of postoperative pancreatitis and fat embolism. M. d.: bind active fibrinolysin. The resulting complex does not have a fibrinolytic effect.
Animal origin Antienzyme preparations (from tissues of slaughter cattle) - contrical trasylol, gordox Bleeding caused by hyperfibrinolysis, including after operations and injuries; before, during and after childbirth; hemorrhagic complications arising during thrombolytic therapy, acute pancreatitis, prevention of postoperative pancreatitis and fat embolism. M. d.: bind active fibrinolysin. The resulting complex does not have a fibrinolytic effect.
 Drugs used for hemophilia Hereditary deficiency of blood clotting factors VIII, IX, XI (one or more). Obtained from a large volume of blood plasma. Expensive. Use according to specifications. indications.
Drugs used for hemophilia Hereditary deficiency of blood clotting factors VIII, IX, XI (one or more). Obtained from a large volume of blood plasma. Expensive. Use according to specifications. indications.
Blood is a liquid tissue of the body that belongs to the connective tissue. In essence, it is an environment that provides the opportunity for the cells of the body to carry out their vital processes.
For the first time, a holistic idea of blood as a system was created by the domestic physiologist Georgy Fedorovich Lang in 1939.
The blood system includes peripheral blood, hematopoietic organs, hematopoietic organs and blood depots.
Main functions of blood:
1) Transport - carries out the transfer of oxygen, energy and plastic material to cells, as well as the removal of metabolic products from them (carbon dioxide, etc.).
2) Protective - characterized by manifestations of cellular and humoral immunity.
3) Thermoregulatory - blood is a universal heat exchanger.
4) Regulatory - transports regulatory substances: hormones and other biologically active compounds.
5) Maintaining homeostasis - ensures the constancy of the internal environment of the body.
As you know, the volume of circulating blood is 6-8% of a person’s body weight (on average 4-6 liters). Blood consists of a liquid part - plasma, and formed elements: erythrocytes, leukocytes, platelets.
Blood plasma consists of 90-92% water, and 8-10% is dry residue, most of which is represented by proteins. The mineral composition of the blood is mainly determined by sodium, potassium, calcium and phosphate ions.
A decrease in blood plasma volume (wounds, trauma, dehydration, etc.) leads to the development of hypovolemia, the extreme degree of which is called hypovolemic shock. These conditions require immediate medical correction, because may lead to the death of the victim.
In some situations (hormonal disorders, various diets, use of medications, etc.) there may be
the ionic composition of the plasma changes significantly. Such conditions are called hypo- or hypernatremia, hypo- or hyperkalemia, etc.
Erythrocytes are red blood cells. They are nuclear-free cells. They have the shape of a biconcave disk. Normally, red blood cells have a size of 6-8 microns (normocyte), and their number, varying depending on gender and body weight, is 4.0-5.0x 1012/L. Red blood cells perform several important functions, the main one of which is respiratory. It lies in the ability of red blood cells to transport oxygen to cells, which is determined by the presence of hemoglobin in the structure of red blood cells.
Hemoglobin is a blood pigment belonging to the class of chromoproteins (i.e. colored proteins). Consists of 4 hemes (4 pyrrole rings in complex with 2 iron atoms) and globin (Fig. 1).
Note that the direct transport of oxygen is carried out by the iron atom located in the structure of hemoglobin, therefore the respiratory capacity of the blood directly depends on the content of the latter in the body. The normal iron content in the body is 2-5 g, two thirds of which is part of hemoglobin. Iron enters the body with food (meat, buckwheat, apples, etc. are rich in it). Absorption of alimentary iron occurs in the small intestine, and it is absorbed only in ionized
form, most actively in the divalent state (Fe2+).
Therefore, for normal absorption of iron, hydrochloric acid is necessary in the stomach (transfers iron from a molecular to an ionized state), as well as ascorbic acid (reduces Fe3* to Fe2’). Looking ahead, we note that it is for this reason that many iron preparations for enteral use contain ascorbic acid.
In the small intestine, divalent iron binds to the parietal transport protein apoferritin, forming a transport complex - ferritin, in the form of which the intestinal barrier passes (Fig. 2). Once in the blood plasma, already in the trivalent state, iron combines with another carrier - P-globulin (transferrin), and the form of this complex enters the tissues. In the bone marrow it is used to build hemoglobin, which is then included in the synthesis of red blood cells.
When there is a lack of iron in the body (due to low intake from food, malabsorption, blood loss, etc.), so-called hypochromic (iron deficiency) anemia develops. It is called hypochromic due to the weakening of the coloring intensity of erythrocytes caused by a lack of chromophore - Fe atoms. This disease also requires drug therapy, because Against this background, the oxygen capacity of the blood decreases, and as a result, the cells suffer from hypoxia.
It should be noted that cyanocobalmin (vitamin B2) plays an important role in the process of formation of normal red blood cells (Fig. 3). Cyanocobalmin (like all vitamins) is not synthesized in the body, but comes from food. In the stomach it forms a complex with a specific protein transcorrin, which is often called intrinsic Castle factor. This protein is strictly specific for cyanocobalamin, is produced in the parietal cells of the fundus of the stomach and performs a single, but very important function - it ensures normal absorption of cyanocobalamin (the latter is also called external Castle factor for this reason). In the blood, cyanocobalamin, turning into the enzyme cobamide, promotes the formation of folinic acid from folic acid, which is used for the synthesis of purine and pyrimidine bases necessary for the synthesis of nucleic acids (DNA) (Fig. 4).
The resulting DNA stimulates cell division of rapidly regenerating tissues (red blood cell precursors and gastrointestinal tract cells), which leads to the formation of normal red blood cells (normocytes).
When there is a deficiency of cyanocobalamin in the body, hyperchromic anemia develops (pernicious anemia, Addison-Birmer anemia). Vitamin B2 deficiency occurs due to various reasons (autoimmune damage to the lining cells of the stomach, gastric resection, tapeworm infestations), the common consequence of which is a lack of intrinsic Castle factor, leading to impaired absorption of cyanocobalamin. As a result of developing vitamin deficiency, the synthesis of normal erythrocyte DNA is blocked (Fig. 4), which, in turn, causes a disruption in the division of erythrocyte precursor cells.
Folic acid
Cobamamide ~
Folinic acid
Purine and pyrimidine bases
Progenitor cell
 Normal red blood cell
Normal red blood cell
Rice. 4. The role of cyanocobalamin in the formation of red blood cells
As a result, instead of normocytes, megalocytes are formed (large, undifferentiated cells of large size - more than 10 microns). On the one hand, these cells are very rich in hemoglobin (therefore anemia is called hyperchromic), but due to their large size, megalocytes cannot penetrate into tissues from
vascular bed. A paradoxical situation arises - there is plenty of hemoglobin and oxygen in the blood, but the cells suffer from its severe deficiency. The bone marrow and tissues of the nervous system are especially sensitive to this.
Let us add that folic acid is important in the process of erythrocyte biosynthesis as a substrate for the subsequent chain of reactions (see Figure 4).
A distinctive morphological feature of leukocytes is the presence of a nucleus, which differs between types of leukocytes in size and degree of differentiation. There are several types of leukocytes:
1. Granulocytes - characterized by the presence of specific granularity in the cytoplasm. These include:
Basophils (mast cells) quantitatively make up 1% of the total number of leukocytes. They maintain blood flow in small vessels; promote the growth of new capillaries; ensure the migration of other leukocytes into tissues, increasing the permeability of the vascular wall; capable of phagocytosis (contribution to general phagocytosis is insignificant); participate in the formation of immediate allergic reactions, releasing the main allergy hormone, histamine, during degranulation.
Eosinophils (amount - 1-5%) are involved in allergic reactions, protect the body from helminth invasions, and participate in phagocytosis (the contribution is also insignificant).
Neutrophils (quantity - 45-75%), being microphages, carry out phagocytosis. On average, one neutrophil can phagocytose up to 20 bacteria or damaged body cells. However, this ability manifests itself only in a slightly alkaline environment, so neutrophils carry out phagocytosis only during the stage of acute inflammation, when the pH has not yet shifted to the acidic side. In addition, neutrophils secrete substances with bactericidal properties (lysozyme, cationic proteins, interferons) and substances that promote tissue regeneration (aminoglycans).
2. Agranulocytes do not have specific granularity in the cytoplasm.
Lymphocytes (quantity - 20-40%) are cells that provide specific immunity. There are T- and B-lymphocytes.
T-pymphocytes are thymus-dependent cells, since their differentiation occurs under the influence of this gland. They provide a cellular immune response. There are several types of T-lymphocytes: T-killers (destroy foreign cells); T-helpers (helper cells, stimulate the proliferation of B-lymphocytes); T-suppressors (suppress the immune response to certain antigenic influences); Immune memory T cells (store information about all antigens, circulating in the blood for more than 10 years).
B lymphocytes (quantity - 2-10%) provide the humoral immune response. They phagocytose bacterial cells, and do this in an acidic environment when the inflammatory process is chronic. In addition, they enhance tissue regeneration and provide antitumor protection.
When the number of leukocytes decreases, leukopenia develops, and when the number increases, leukocytosis develops.
Leukopenias can be primary, i.e. congenital, hereditary (neutropenia, Chediak-Higashi syndrome - monocytopenia in combination with a decrease in phagocytic activity), and secondary, i.e. acquired. Secondary leukopenias are more common. They can occur due to a violation of leukopoiesis (nutritional, toxic (benzene poisoning), medicinal (chloramphenicol), radiation, tumor processes), destruction of leukocytes (radiation), redistribution of leukocytes (shock, etc.), increased loss of leukocytes (burns, osteomyelitis ).
Leukemia can be physiological (during food intake) and pathological (adaptation to pathological conditions, tumors).
The described conditions, like other blood diseases, require drug correction (see below).
Platelets are non-nuclear blood cells that have a biconvex shape. The platelet size is 0.5-4 microns, i.e. These are the smallest blood cells. Normally, 1 mm3 of plasma contains 200-400 thousand platelets. The main function of platelets is to provide the vascular-platelet component of hemostasis (preventing and stopping bleeding when small and medium-sized vessels are damaged).
Vessel lumen
5. B Platelet aggregation, formation of a platelet plug upon injury
 Activation of fibrinolysis. removal of excess platelets
Activation of fibrinolysis. removal of excess platelets
5. G. Reendothelnzatsnya
Rice. 5. General mechanisms of vascular hemostasis
When vessels are damaged, processes are activated aimed at restoring the integrity of the vascular wall (Fig. 5). In the first few seconds, platelet aggregation occurs at the site of endothelial destruction, resulting in the formation of a blood clot that “seals” the hole, stopping the bleeding. Then platelet aggregation stops, and the excess part of the platelet plug, which protrudes into the lumen of the vessel and interferes with blood flow, is lysed by fibrinolysis enzymes (for details on fibrinolysis, see.
below). The final stage of the described cascade is the regeneration of tissue of the vascular wall (reendothelialization).
Thus, platelet aggregation is an important component of the physiology of the blood system. However, in some pathologies, the activity of this process goes beyond its allotted limits, as a result of which the rheological properties of the blood adversely change - it becomes more viscous, and blood clots form. All this can significantly disrupt hemodynamics, leading to embolism and death, therefore normalization of impaired platelet aggregation is an important component of the pharmacology of the blood system (see below).
Platelet aggregation is controlled by a number of biologically active substances, the main of which are thromboxane Ag and prostacyclin. belonging to the class of prostaglandins. Thromboxane A2 is the main physiological inducer of platelet aggregation. The mechanism of its action can be represented as follows (Fig. 6).
Thromboxane A2 stimulates specific thromboxane receptors located on the platelet membrane, which leads to activation of the enzyme phospholipase C, the primary messenger associated with the thromboxane receptor. Phospholipase C promotes the synthesis of secondary messengers: inositol-3-phosphate (IP()
280-
and diacylglycerol (DAG), which increase the intracellular concentration of Ca2* ions. Calcium is a key agent of platelet aggregation, because it activates glycoprotein receptors (another type of platelet membrane receptors), through which cell gluing occurs due to the activation of fibrin threads.
In turn, prostacyclin, stimulating the corresponding prostacyclin receptors, activates the enzyme adenylate cyclase, which promotes the accumulation of cAMP in the cell (synthesized from ATP). Cyclic adenosine monophosphate (cAMP) is a second messenger of cellular signal transmission that lowers the concentration of calcium ions inside platelets. As a consequence, a weakening of the activity of glycoprotein receptors and a decrease in platelet aggregation.
It is important to note that the synthesis of thromboxane A2 and prostacyclin has some peculiarities. On the one hand, both are formed from arachidonic acid according to the general scheme of prostaglandin synthesis. However, thromboxane A2 is formed directly in platelets, and this reaction at the last stage is catalyzed by the enzyme thromboxane synthetase (Fig. 7).
Membrane phospholipids
Phosphaiipisa A.
Arachidonic acid
Cyclooxygenase
Cyclic endoperoxyls (PGO2/H2)
In this case, prostacyclin is synthesized in the vascular endothelium under the influence of another enzyme - prostacyclin synthetase.
These differences form the basis for the action of some antiplatelet drugs (see below).
When large vessels are damaged, the integrity of the circulatory system is maintained by plasma (hemocoagulation) hemostasis. Its implementation is ensured by the blood coagulation system. The main provisions of the theory of blood coagulation were formulated in 1895 by A.A. Schmidt (University of Tartu, Estonia):
1. The process of blood coagulation is staged.
2. The next stage ends with the formation of an active enzyme, i.e. Blood clotting is an enzymatic process.
3. The product of the previous stage is an activator for the subsequent stage, i.e. Blood coagulation is a cascade process.
In the process of blood clotting, there are fundamentally 3 phases:
1. Formation of the prothrombinase complex.
2. Thrombin formation.
3. Fibrin formation.
The mechanisms of blood clotting are quite complex, so we will highlight only the main points necessary to understand the mechanisms of action of drugs.
In the intact human body, coagulation factors are in an inactive state. Let us recall that coagulation factors are usually designated by Roman numerals in the chronological order of their discovery. The most important in this section are: factor I (fibrinogen) - a macromolecular blood protein that normally has a sol structure, and when coagulation processes are initiated, it turns into a gel state - fibrin; factor II (prothrombin); factor III (thromboplastin) - phospholipid of cell membranes; factor IV (Ca2* ions) is a catalyst for all enzyme activation processes.
In the liver, under the influence of vitamin K, a number of coagulation factors are synthesized, the main one of which is prothrombin. It enters the blood, where, under the influence of prothrombin activators, formed during vascular damage, it is converted into thrombin (Fig. 8). The latter, in turn, stimulates the formation of fibrin from fibrinogen. Fibrin is a high-molecular protein compound with a gel-like quaternary structure that “seals” the damaged area of the vessel, restoring its integrity.
The blood coagulation system is balanced by the fibrinolysis system, designed to maintain the blood in a fluid state. The main agent of this system is the proteolytic enzyme fibrinolysin (plasmin), which has the ability to break down fibrin strands.
Blood coagulation system
Fibrinopsptids (fibrinolysis products)
Rice. 8. Blood coagulation and fibrinolysis system
Facilities,affecting the system
blood. Lecture outline:
1. Basic terms used in
analysis of the topic.
2. Classification of means affecting
blood system.
3. Characteristics of agents affecting
erythropoiesis
4. Characteristics of agents affecting
leukopoiesis
5. Scheme of thrombus formation
6. Characteristics of hemostatic agents
7. Characteristics of Antithrombotic
funds
8. Characteristics of agents affecting
fibrinolysis Basic terms
used in
topic. Anemia
Leukopenia
Hemostasis
Thrombosis
Fibrinolysis
Platelet aggregation
Consolidation
Erythropoiesis
Leukopoiesis Classification of funds
affecting the blood system. 1. Drugs affecting erythropoiesis.
A. Stimulating erythropoiesis
Iron preparations for oral use:
hemopher, ferrogradumet, tardiferon, Totema,
sorbifer.
Iron preparations for parenteral use:
ferkoven, Ferrum lek, ferbital.
Vitamin preparations:
Cyanocobalamin, folic acid, pyridoxine,
riboflavin, combination vitamin preparations.
B. Suppressing erythropoiesis.
Radioactive phosphorus. 2.Medicines affecting leukopoiesis.
A. Stimulating leukopoiesis
Methyluracil, leucogen, pentoxyl.
B. Suppressing leukopoiesis.
Dopan, myelosan, methotrexate, mercaptopurine. 3.Means that affect the function of hemostasis.
A. Increasing blood clotting
(hemostatics)
1.Coagulants:
Direct: thrombin, fibrin, hydrogen peroxide,
hemostatic sponge, statin, calcium chloride
Indirect: vitamin K, vikasol.
2. Antifibrinolytic (fibrinolysis inhibitors)
Aminocaproic acid, Ambien, Contrical, Gordox
3. Angioprotectors
Dicynone, ethamsylate, dobesylate, ascorbic acid,
rutin, Ascorutin.
4.Medicinal plant raw materials.
Nettle leaf, water pepper herb, shepherd's purse,
yarrow, viburnum bark. B. Antithrombotic (lowering
blood clotting)
1. Antiplatelet agents.
Aspirin, chimes, ticlopidine, xanthinol
nicotinate, pentoxifylline.
2. Anticoagulants.
Direct action: heparin, hirudin.
Indirect action: warfarin, Phenilin, syncumar,
neodicoumarin.
Outside the body: sodium citrate.
3.Fibrinolytic.
Direct acting: fibrinolysin
Indirect action: streptokinase. Facilities,
stimulating erythropoiesis. Anemia is a painful condition
characterized by a general disorder
blood and its qualitative change
composition.
Types of anemia:
Hypochromic
Hyperchromic. Hypochromic anemia-iron deficiency
anemia
Hypochromic anemia is characterized by
a sharp decrease in hemoglobin in
red blood cells.
Causes:
Extensive blood loss
Lack of iron in food
Gastrointestinal diseases associated with
low acidity. Prescribe iron supplements with ascorbic acid
acid or contains ascorbic acid
acid.
Side effects.
Formation of black plaque on teeth Prescribed after meals, without chewing. Solutions
- through a tube.
Darkening of stool, constipation
Dyspeptic disorders. Hyperchromic anemia is an increase
hemoglobin content, but sharply decreases
number of red blood cells, and new ones are formed
immature forms.
Hyperchromic anemia is divided into:
Pernicious
Macrocytic. Pernicious anemia – B12 deficiency
anemia and is characterized by a decrease
iron absorption.
Cyanocobalamin is prescribed intramuscularly every other day.
course 14-30 days.
- necessary for normal hematopoiesis and
maturation of red blood cells.
- enhances blood clotting function. Macrocytic anemia is
folate deficiency anemia.
Folic acid tablets are prescribed
1 x 3 times a day, course 20-30 days.
stimulates the function of red bone marrow,
increases the content of red blood cells in the blood,
participates in the synthesis of amino acids. Drugs that inhibit erythropoiesis.
Radioactive phosphorus.
Used in oncology for erythremia -
intensive proliferation of bone marrow, leading to
to a very large increase in content
red blood cells Facilities,
stimulating leukopoiesis. Indications for use:
Aleikia
Leukopenia
Agranulocytosis
Causes:
Poisoning with industrial poisons
Drug poisoning
Infectious diseases (malaria, syphilis,
typhoid fever)
Irradiation Methyluracil, leucogen, pentoxyl.
Mechanism:
Stimulate leukopoiesis,
accelerate regeneration processes,
immunostimulating effect.
Application:
orally for leukopenia, agranulocytosis, hepatitis,
pancreatitis.
Methyluracil is also prescribed externally in suppositories and
ointments for slow-healing wounds, burns, cracks
rectum. Facilities,
inhibiting leukopoiesis. Dopan, myelosan, methotrexate,
Mercaptopurine.
Used for leukemia and others
diseases associated with growth
hematopoietic tissues (lymph nodes,
bone marrow, spleen). Facilities,
increasing blood clotting.
Hemostatics. Blood coagulation system - hemostasis.
1. Cellular hemostasis: affects aggregation
platelets, improves microcirculation and
rheological properties of blood.
2.Plasma hemostasis: affects coagulation
blood (coagulation)
3.Fibrinolysis. General scheme of thrombosis.
1. Formation of active thromboplastin (an enzyme
formed when platelets break down)
2. The transition of prothrombin to thrombin under the influence
thromboplastin and calcium ions.
Thrombin is formed in the liver with the participation of vitamin K.
3. The transition of fibrinogen to fibrin under the influence
thrombin and calcium ions. Preparations for topical use
act at the level of cellular hemostasis,
promote local formation of blood clots in
capillaries, venules, arterioles.
Hemostatic sponge, viscose, statin,
hydrogen peroxide 3%,
Apply
with superficial bleeding from the skin, nose,
rectum. Direct coagulants.
These are natural factors.
Thrombin, fibrinogen, calcium salts.
Apply
for bleeding, the cause of which is a decrease in
fibrinogen.
Fibrinogen – intravenous drip. Indirect coagulants.
Vikasol (synthetic analogue of vitamin K)
Mechanism:
stimulate the formation of prothrombin and increase
blood clotting.
Application:
planned operations,
bleeding with a low prothrombin index
overdose of anticoagulants.
The effect occurs after 12 – 18 hours,
tablets are prescribed 1 x 3 times a day
IV, IM 1 ml 2 times a day. Antifibrinolytic agents (inhibitors
fibrinolysis).
Aminocaproic acid, Ambien,
kontrikal, gordoks.
Mechanism:
Inhibits the formation of fibrinolysin and
prevent the formation of blood clots.
Application:
Bleeding with increased fibrinolytic
activity
Peptic ulcer with bleeding
Cirrhosis of the liver
IV drip. Facilities,
reducing blood clotting
(Antithrombotic) General use.
Treatment and prevention of diseases
with ischemic heart disease
Cerebrovascular
diseases
Atherosclerotic lesions
peripheral vessels
Venous thrombosis. Antiplatelet agents (inhibitors of cellular hemostasis:
aspirin, chimes, pentoxifylline,
ticlopidine, plavix.
Pharmacodynamics
Reduce platelet aggregation, prevent
formation of blood clots, improve microcirculation
blood.
Applicable:
For compensatory therapy of infarction
Prevention and treatment of thrombosis
Cerebrovascular accident Anticoagulants.
Pharmacodynamics
Interferes with blood clotting processes,
prevent the formation of intravascular thrombi
and promote their resorption.
Main indications:
Thrombosis due to CVD
Myocardial infarction
Atherosclerosis
Vascular surgeries
Blood transfusion
For embolisms Direct acting anticoagulants.
Heparin, hirudin
Mechanism:
Reduces thrombin activity.
Pharmacodynamics:
Reduces blood clotting in the body and outside
Prevents the formation of blood clots
Reduces platelet aggregation
Side effect:
tendency to bleed and hemorrhage.
The antagonist is protamine sulfate. Anticoagulants of indirect action.
Warfarin, neodicoumarin, Phenilin,
sinkumar
Mechanism:
prevent the formation of prothrombin in the liver.
Application:
Treatment and prevention of thrombosis, thromboembolism,
thrombophlebitis
Myocardial infarction
Angina pectoris
Heart disease
Antagonist – vikasol Fibrinolytic agents.
Fibrinolysin is a natural blood factor.
Mechanism:
melts the surface layers of the blood clot.
Application:
in acute thrombosis in combination with
anticoagulants, for pulmonary thromboembolism,
myocardial infarction

