Vascular ischemia of the foot. Chronic ischemia of the lower extremities - treatment, diagnosis and symptoms
Every cell, tissue, organ human body need oxygen. This is exactly what is needed for normal height and development. All processes in the body take place with the participation of oxygen.
And if for one reason or another the body does not receive enough oxygen, the cells suffer from its deficiency, do not function at full capacity, or even die. The condition when cells lack oxygen is called ischemia. Any organs and parts of the body can suffer from ischemia human body, the lower extremities are no exception.
1 Why does ischemia occur?
Ischemia lower limbs in most cases (about 96%) occurs due to vascular atherosclerosis, and in particular branching abdominal aorta, iliac arteries or arteries that branch from them. Atherosclerosis is a condition when the body, due to excess accumulation cholesterol, triglycerides, plaques are deposited in the walls of blood vessels.
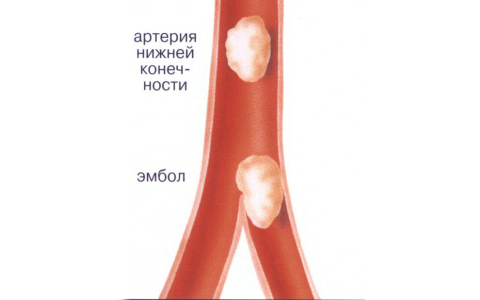
Because of these plaques, the lumen of the artery narrows and blood flow slows down or stops. Sometimes plaques can break off and migrate with the bloodstream, while they clog any lumen of the vessel. This condition is called embolism. Also, vascular ischemia of the legs often occurs in patients suffering from diabetes mellitus, inflammation of the vascular walls - endarteritis, increased coagulability blood when the risk of thrombosis is high.
There are also prerequisites for the occurrence of ischemia. A huge percentage of experienced smokers know firsthand about ischemia of the lower extremities. Smoking is the main provoking factor in the development of ischemia. These factors also include high blood pressure, increased level cholesterol and “bad” lipoproteins, overweight bodies.
2 What are the symptoms of lower limb ischemia?

The most remarkable and important symptom- pain in the leg muscles, most often the calf muscles, which occurs when walking. Patients may describe this condition as “pressing”, “squeezing”, “burning”, “fettering”. These pains go away when you stop walking and take a short rest. They intensify again when running, climbing stairs, or increasing the pace of walking. This symptom has its own name - “intermittent claudication.”
A limb affected by ischemia is characterized by dry skin, pallor, the temperature of such a limb is reduced and it is cold to the touch. Subjectively, patients complain of chilliness, coldness, a crawling sensation, numbness in the legs, and cessation of hair growth on the limbs. Half of men with leg ischemia suffer from impotence. If the condition worsens, the patient does not receive any treatment, cracks and trophic ulcers of the extremities may occur.
It is noteworthy that in people suffering from diabetes mellitus, ulcers are painless, which worsens the appeal of such patients to a doctor at the stage of their formation. Ulcers can become necrotic, black spots appear, first in the area of the toes, heels, then in the overlying areas, gangrene forms.
3 What is ischemia of the lower extremities?
![]()
Ischemia is classified into acute and chronic. Acute occurs against the background of relative well-being, spontaneously, abruptly. IN short terms symptoms develop and the patient’s well-being worsens. This is a condition that requires immediate medical attention. Acute ischemia often develops due to thrombosis or embolism of a vessel atherosclerotic plaque or a blood clot.
Emboli can be of cardiac origin, for example, if the patient has rhythm disturbances such as atrial fibrillation, or a vessel aneurysm, blood clots can occur due to injury to the vessel.
Chronic ischemia lower extremities - this is a condition that develops gradually, over a long period of time, with a progressive deterioration in the patient’s well-being; it is more common in male smokers and diabetics. Its cause, in most cases, is obliterating atherosclerosis.

In addition to acute and chronic, in the classification of ischemia it is important to take into account the severity. According to the severity of ischemia, it is classified into stages:
- Stage 1 - the patient complains of pain, a feeling of stiffness, burning in the leg muscles during heavy physical activity. These complaints occur when walking after covering a distance of more than 1 km;
- Stage 2a - complaints of pain arise already when walking from 250 to 1000 m;
- Stage 2b - walking distance without pain is 50-250m;
- Stage 3 - Pain occurs when walking less than 50m, bothers you at night, at rest;
- Stage 4 - in addition to severe, persistent, excruciating pain, ulcers, necrosis, blackening of the toes and heels occur, and gangrene develops.
According to the classification, starting from the third stage, ischemia is considered critical, in which blood flow in the artery is almost completely absent, and without restoration of blood flow, gangrene develops. Without proper surgical treatment, medication, unfortunately, is practically ineffective at this stage, a patient suffering from critical ischemia faces limb amputation within one year.
4 Smoking or walking?

Separately, I would like to touch upon the topic of smoking and ischemia of the lower extremities. When starting to smoke, few people think about the fact that after 15-20 years they risk being left without legs. Why is this happening? Nicotine increases vascular tone, which leads to vasoconstriction, in smoking people the blood thickens, which leads to an increased risk of thrombosis, blood pressure rises, these and other factors contribute to the occurrence of ischemia.
Some long-term smokers with severe ischemia of the lower extremities, when they learn that they risk smoking before amputation, quit their long-term bad habit in an instant. But the majority make a choice in favor of cigarettes and become disabled smokers. Every smoker should be warned about such consequences of smoking, and everyone chooses to smoke or walk.
5 Diagnosis of ischemia of the lower extremities

When examining a patient, the doctor pays attention to the color of the skin of the legs, its temperature, the presence or absence of pulsation in the arteries of the lower extremities, and determines the sensitivity of the skin starting from distant areas. It is also important to carefully collect complaints, medical history, identify predisposing factors for the development of the disease, and concomitant diseases.
Main methods instrumental diagnostics are:

In addition to diagnosing blood vessels directly, they also use laboratory methods: blood biochemistry (determine cholesterol levels, lipid spectrum, fibrinogen, blood glucose), ECG, EchoCG, fundus examination, ultrasound of the kidneys. Carry out diagnostics to identify concomitant pathology. In order to take into account all diseases, decide on treatment tactics.
6 Treatment of ischemia

If ischemia of the lower extremities is detected at the earliest stages, when there are no obvious clinical signs or symptoms of trophic disorders, drug treatment is possible. It includes the application medicines, blood thinners, drugs that lower cholesterol levels, normalize blood pressure, drugs aimed at improving blood flow, painkillers if necessary.
In each case, the attending physician prescribes treatment individually, taking into account concomitant pathology and individual tolerance patient. Effective in early stages physical exercise, selected and developed by a master of exercise therapy, physiotherapeutic treatment, hyperbaric oxygen therapy. But, if drug therapy does not bring results, and the degree of ischemia increases, it is indicated surgical treatment.
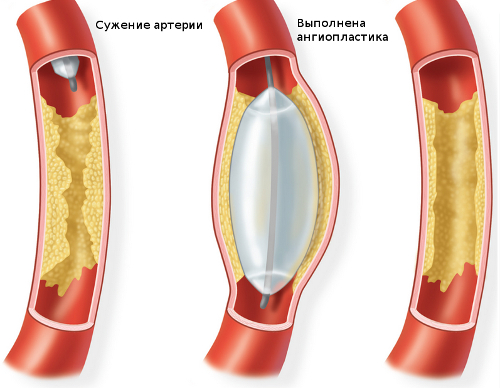
Apply following methods vascular operations:
- balloon angioplasty - expansion of the vessel with a special balloon, resulting in normalization of blood flow;
- installation of a stent in a vessel;
- endarterectomy - removal of plaque in a vessel;
- bypass surgery and prosthetics.
If gangrene of a limb has developed, these surgical treatment methods are ineffective, and only amputation of the limb can save the patient.
Mandatory at all stages of ischemia complete failure from smoking, stabilization of body weight, blood pressure, cholesterol levels. There is a need for rational balanced diet, prevention of physical inactivity.
It is important to monitor your health, remember the symptoms of limb ischemia, and, at the first alarm bells, contact your doctor.
Acute arterial occlusions — acute disorder blood circulation distal to the site of occlusion of the artery by an embolus or thrombus. The condition is considered urgent. Proximal and distal to the occlusion site, normal blood flow is disrupted, which leads to additional thrombus formation. The process can involve collaterals, and the thrombus may spread up to the venous system. The condition is considered reversible within 4-6 hours from its onset (in English literature this time period is called the “golden period”). After this time, deep ischemia leads to irreversible necrotic changes.
Code according to the international classification of diseases ICD-10:
- I74.2
- I74.3
- I74.9
Statistics. The frequency of hospitalizations is 5-10:10,000 population. Leading cause of death and limb loss in old age. The predominant age is over 60 years. The predominant gender is male.
Reasons
Etiology
. Arterial embolism is the obstruction of a vessel by an embolus that has migrated through the bloodstream. Emboli are classified depending on the primary source of the lesion. Source - left half heart... Parietal thrombus as a result of arrhythmia, heart attack, surgical trauma, stenosis mitral valve, endocarditis and cardiac weakness of any etiology... Vegetations on the valves... Foreign bodies... Tumors.. Source - aorta... Sclerotic plaques... Trauma followed by thrombosis... Aneurysm... Foreign bodies.. Source - pulmonary veins... Thrombosis... Trauma followed by thrombosis... Tumors.. Source - right heart: with defects of the interventricular and interatrial septum.. Source - veins great circle blood circulation: with defects of the interventricular and interatrial septa.
. Artery thrombosis. Virchow's pathogenetic triad: damage vascular wall, changes in blood composition, disturbances in blood flow (its laminar flow).. Damage to the vascular wall... Obliterating atherosclerosis... Arteritis: systemic allergic vasculitis(thromboangiitis obliterans, nonspecific aortoarteritis, periarteritis nodosa), infectious arteritis... Trauma... Iatrogenic vascular damage... Other (due to frostbite, exposure to electric current etc.) .. Blood diseases: polycythemia vera, leukemia.. Diseases of internal organs (atherosclerosis, hypertension, malignant tumors etc.) .. Blood flow disturbances... Extravasal compression... Aneurysm... Spasm... Acute failure blood circulation, collapse... Previous surgery on the arteries.
Classification of acute limb ischemia
. Stress ischemia: absence of signs of ischemia at rest and their appearance during exercise.
. Ischemia degree I. Sensitivity and movement in the affected limb are preserved.. Grade I ischemia is characterized by a feeling of numbness, coldness, and paresthesia.. With grade IB ischemia, pain appears in the distal parts of the limb.
. Ischemia degree II. Characteristic disorders of sensitivity, as well as active movements of the limb: from paresis (grade IIA) to plegia (IIB).
. Ischemia of the III degree is characterized by the beginning of necrobiotic phenomena, which is clinically expressed in the appearance of subfascial edema (IIIA), and later - muscle contracture: partial (IIIB) or total (IIIB).
Genetic aspects. A combination with hereditarily caused increased blood clotting and hyperlipidemia syndromes is possible.
Clinical manifestations
. Five main symptoms— in the English-language literature, the “five P” symptom complex. (If any of these signs are present, routine examination to identify occlusion is indicated. Occlusion of vessels located more proximally leads to more rapid progression of symptoms. Occlusion at the level of the aortic bifurcation can cause symptoms of damage on both sides.) .. Pain ( Pain) - localized distal to the site of occlusion, diffuse, gradually intensifies (sometimes disappears with spontaneous resolution of occlusion). Most often, this is the first sign of embolism. Does not improve with changes in the position of the limb. Pulselessness is mandatory for the diagnosis of embolism or thrombosis. Doctors often lack the skill to determine the pulse on a. dorsalis pedis, which leads to diagnostic errors. When determining the pulse, it is necessary to compare it on both limbs. Pale (Pallor) - the skin color is pale at first, then cyanosis occurs. The temperature of the limb should be checked sequentially from top to bottom. There may be signs of chronic ischemia (skin atrophy [dryness, wrinkling, peeling], lack of hair, thickening and brittleness of nails).. Paresthesia - numbness, tingling sensation, crawling "goosebumps" appear in the early stages of thrombosis. First, tactile sensitivity (the sensation of touch) disappears. In diabetes, tactile sensitivity may be initially reduced. The disappearance of pain and deep sensitivity indicates severe ischemia. Paralysis - motor function violated by late stages and indicates deep ischemia.
Most frequent localization embolism (along all main branches of the aorta) .. Femoral artery— 30% .. Iliac — 15% .. Popliteal — 10% .. Brachial — 10% .. Aortic bifurcation — 10% .. Mesenteric — 5% .. Renal — 5%.
. Determination of the level of occlusion in the arteries. Absence of pulse below and its intensification above the level of occlusion. Symptoms usually appear one joint below the level of occlusion.
. Differences in the clinical picture of embolism and thrombosis.. Embolism... Often preceded by heart disease: rheumatic mitral stenosis, MI, myxoma of the left atrium... Embolism is often provoked by a violation of the heart rhythm... In other cases, there are aneurysms of large arteries... The onset of the disease is sudden with severe pain... Above the level of embolism - increased pulsation of the artery.. Thrombosis. .. In the anamnesis - chronic diseases vessels (atherosclerosis of the arteries or endarteritis) ... Preceded by trophic disorders: hypotrichosis of the limbs with atherosclerosis, hyperkeratosis of the feet, deformation of the nail plates, etc. ... Symptoms appear gradually. More often, paresthesia occurs first, and then pain... Systolic murmur during auscultation above the site of blockage and above the arteries of the unaffected side... May be preceded by trauma or intervention on the vessels.
Diagnostics
Laboratory data. PTI rises. Bleeding time is reduced. Fibrinogen - content increases. IN postoperative period needs to be controlled... Daily diuresis.. OAM.. ACR.. Serum myoglobin.. Serum urea.. Serum electrolytes, primarily potassium.
Special studies. Doppler sonography: presence or absence of blood flow. Preoperative angiography. If the onset is acute, there is a source of emboli in the heart, and the patient has no previous history of intermittent claudication, then there is no need for preoperative angiography.
Differential diagnosis. Dissecting aneurysm of the abdominal aorta. Acute thrombophlebitis of the deep veins of the limb (white painful phlegmasia).
Treatment
TREATMENT
Stationary mode.
Treatment tactics depend on the degree of ischemia. Tension ischemia and grade IA - you can limit yourself to conservative treatment. If there is no effect within 24 hours in a patient with vascular embolism or within 7 days in a patient with thrombosis, organ-preserving therapy is required surgery. Ischemia IB-IIB degrees - emergency surgery aimed at restoring blood flow (thrombus - or embolectomy, reconstructive surgery bypass). Ischemia of IIIA-IIIB degrees - emergency thrombus - or embolectomy, bypass surgery, necessarily supplemented by fasciotomy. In some cases, the operation is accompanied by regional perfusion of the limb. Ischemia IIIB degree - primary amputation of the affected limb, because restoration of blood flow can lead to autointoxication and death of the patient.
Conservative therapy. If ineffective drug therapy One should not hesitate with surgical intervention, since passive tactics can lead to the death of the patient from increasing intoxication.
. Antithrombotic therapy. Heparin - first 100 IU/kg (5000-10,000 IU) IV or 20,000-30,000 IU (1000-1500 IU/h) IV drip, then 60,000-80,000 IU/ days (under the control of blood clotting time, PTT or INR). Fractional heparinization is continued for up to 10 days. 1-3 days before discontinuation of heparin, indirect anticoagulants are started. Contraindications: allergic reactions, hemorrhagic diathesis, trauma (for example, head injury), hematuria, hemoptysis, acutely developed aortic aneurysm.. Anticoagulants indirect action: ethyl biscoumacetate, phenindione. The effect of indirect anticoagulants is controlled by determining the PTI (kept at 50-40% as long as there is a risk of thrombosis). If there is bleeding, discontinue the drug, begin the administration of menadione sodium bisulfite, vitamin P, ascorbic acid, calcium chloride, transfusion of platelet mass, fresh frozen blood plasma.. Activators of fibrinolysis, for example xanthinol nicotinate.. Antiplatelet agents... Pentoxifylline... Acetylsalicylic acid(cannot be prescribed together with indirect anticoagulants) ... Dipyridamole.
Fibrinolytic agents (fibrinolysin, streptokinase, streptodecase, alteplase [tissue plasminogen activator]). Contraindicated in patients with intracardiac thrombi due to the risk of developing repeated embolisms, as well as in recent MI, aneurysms, dissecting aortic aneurysm, stroke, trauma, severe arterial hypertension, after recent operations.
. To improve blood circulation in an ischemic limb.. alprostadil is quite effective - it has a vasodilating, aniagregant effect, improves microcirculation.. antispasmodics (papaverine hydrochloride, drotaverine) are much less effective.. physiotherapeutic procedures (diadynamic currents, magnetic therapy, regional barotherapy) if the patient’s condition is satisfactory .
. To improve tissue metabolism in the ischemic zone - protease inhibitors (aprotinin), antioxidants.
. To ensure high diuresis (preferably 100 ml/h) - infusion therapy.
Surgical treatment. Indirect embolus and thrombectomy. The Fogarty balloon catheter is most often used. Endarterectomy and bypass surgery - if the Fogarty method is not applicable.
Postoperative management- anticoagulant therapy to prevent recurrent embolism and rethrombosis.
Complications. Acidosis, myoglobinuria, hyperkalemia. Relapse of occlusion. Persistent occlusion due to the inability to eliminate a thrombus or embolus. Reperfusion syndrome is a syndrome that occurs when blood flow is restored in an ischemic limb; its manifestations are similar to positional injury and partly to the syndrome prolonged compression.. Predisposing factors: combined arterial damage, deep and prolonged ischemia, arterial hypotension.. Observed in both the upper and lower extremities.. Clinical signs... Severe pain at rest... Hypoesthesia of the areas of innervation of the affected nerves... Paralysis of the muscles of the affected limb distal to the former occlusion... Painful tense swelling... Intoxication (vomiting, severe headache, impaired consciousness) ... Oliguria.. Early consequences unrecognized reperfusion syndrome: sepsis, myoglobinuria and renal failure, shock, multiple organ failure syndrome.. Late consequences unrecognized reperfusion syndrome: ischemic contractures, infections, causalgia, gangrene.
Course and prognosis . 90% favorable outcomes at timely treatment. Late start treatment or lack thereof causes death or loss of limb. Hospital mortality is 20-30% depending on causative factors.
ICD-10. I74 Embolism and thrombosis of arteries. I74.2 Embolism and thrombosis of arteries upper limbs. I74.3 Embolism and thrombosis of the arteries of the lower extremities. I74.9 Embolism and thrombosis of unspecified arteries.
Vascular diseases of the upper extremities leading to ischemia are less common compared to diseases of the lower extremities [Spiridonov A.A., 1989; Sultanov D.D., 1996; Bergau J.J., 1972], and this is primarily due to anatomical features: the upper limbs, compared to the lower ones, are characterized by the presence of well-developed collaterals and less muscle mass. However, ischemia of the upper extremities often leads to consequences no less pronounced than ischemia of the lower extremities, and often ends in amputation, especially when distal forms defeats. At the same time, the percentage of amputations remains quite high and, according to J.H.Rapp (1986) and J.L.Mills (1987), reaches 20%.
Chronic arterial insufficiency of the upper extremities, according to some authors, accounts for 0.5% of all cases of ischemia of the extremities and 0.9% of surgical interventions on the arteries.
The first descriptions of ischemia of the upper extremities date back to the beginning of the 19th century, when Maurice Raynaud first identified in 1846 independent disease"state of transitory
symmetrical digital ischemia due to impaired reactivity of small digital vessels." However, long before the first publication by M. Raynaud, there were already unsystematized reports in the literature about similar changes in the fingers.
The first report of damage to the branches of the aortic arch in a patient with syphilis belongs to Davis (1839). Savory (1856) presented a description of a young woman in whom the arteries of both upper limbs and the left side of the neck were obliterated; in all likelihood, these changes are characteristic of nonspecific aortoarteritis. In 1875, Broadbent published a report of the absence of a pulse in the radial artery.
Almost simultaneously, the first steps were taken in uncovering the origin of hand ischemia thanks to the development and more active learning pathological anatomy.
The first report of narrowing of large arteries emanating from the aortic arch belongs to the pathologist Yelloly (1823). In 1843, Tiedemenn’s fundamental work “On the narrowing and closure of arteries” was published, and in 1852, Rokitansky’s essay “On Some major diseases
arteries", in which for the first time a description of changes in the walls of arteries is given and an assumption is made about possible reasons various obliterating diseases.
Diseases of the upper extremities naturally led to the need to perform angiography of the hand. Haschek and Lindenthal were the first to perform postmortem angiography of an amputated upper limb in 1896. Berberich and Kirsch (1923) were the first to report successful in vivo angiography.
Chronic ischemia upper extremities is a consequence of any systemic disease, but may also be a manifestation of atherosclerotic lesions or neurovascular syndromes.
The most common systemic diseases leading to arm ischemia are Raynaud's disease or syndrome, thrombangiitis obliterans (Buerger's disease), nonspecific aortoarteritis, atherosclerosis, and more rare - scleroderma, periarteritis nodosa.
The etiology of primary vasculitis is unknown, but there are a number of theories about the occurrence of a particular systemic disease, and each of these theories has the right to exist. Systemic diseases, as a rule, develop after infections, intoxications, administration of vaccines, possibly hypothermia; a viral etiology of the disease cannot be ruled out. For example, with periarteritis nodosa, high titer HBs antigen is often detected in the blood of patients. Periarteritis nodosa characterized by damage to both arteries and veins, the walls of which undergo fibrinoid necrosis and inflammatory changes involving all three layers. In recent years, fixation of the HBs antigen in combination with immunoglobulins and complement has been discovered in the wall of affected vessels.
(SSD) progressive fibrosis is observed blood vessels, skin of the hands and upper body, as well as involvement in fibrosis of skeletal muscles and internal organs. An important link in the pathogenesis of the disease is a violation of microcirculation with proliferation and destruction of the endothelium, thickening of the wall and narrowing of the lumen of microvasculature vessels, vasospasm, aggregation of formed elements, stasis and deformation of the capillary network. These changes lead to necrosis of the soft tissues of the fingertips.
In neurovascular syndromes there is chronic injury neurovascular bundle from the outside. In this case, isolated damage to the subclavian artery is possible.
In patients with nonspecific aortoarteritis, ischemia of the upper limb can develop when the subclavian artery is involved in the inflammatory process. According to various authors(A.V. Pokrovsky, A.A. Spiridonov), in 80% of cases the second or third segment of the artery is affected, in 10-22% of cases - more proximal segments of the subclavian artery (B.V. Petrovsky, J. Oberg).
On early stage There is a thickening of the vessel wall, leading to its unevenness, but without narrowing the lumen of the vessel. As arteritis progresses, segmental stenoses and occlusions are formed, the development of which leads to limb ischemia.
Atherosclerosis affects large main arteries: in cases with ischemia of the upper limb, this is the subclavian artery and, as a rule, its first segment. Ischemia of the upper extremities with proximal atherosclerotic lesions of the branches of the aortic arch is observed in 30% of patients, and 1/10 of them are critical [Beloyartsev D.F., 1999]. According to I.A. Belichenko (1966), ischemia
of the upper limb with this form of lesion is 42%. An atherosclerotic plaque narrows or occludes the lumen of the artery, and in most cases there is a stealing of the blood supply to the brain through the vertebral artery, which sometimes compensates for ischemia of the arm.
According to various authors, the frequency of inflammatory changes in the arteries of the upper extremities with thromboangiitis obliterans ranges from 50 to 80%, and in 75% of cases the arteries of both the lower and upper extremities are affected.
Etiology and pathogenesis thromboangiitis obliterans (OT) have not been fully elucidated. There are many theories about the occurrence of thromboangiitis obliterans, such as genetic predisposition, allergic and autoimmune theories and many others. Each of these theories has a right to exist.
One of the main causes of OT is rightfully considered to be the autoimmune theory. In this case, damage to the vascular wall by altered endothelial cells is observed, which in turn leads to activation of T- and B-lymphocytes, the formation of circulating immune complexes, and biologically active amines.
Some authors consider genetic predisposition in the etiopathogenesis of OT. The genes of the HLA system are mainly associated with the regulation of the immune response, however, the implementation of the disease is not always possible without provoking factors external environment. Allergy to tobacco components is considered one of the main factors initiating this disease. There is a definite connection with smoking or chewing tobacco, and, according to many authors, all patients with OT are
heavy smokers. It is not yet clear, however, whether the effect of tobacco is vasoactive or immunological. IN lately Data have emerged on the effect of hashish and cocaine on the development of OT involving the upper extremities. The recent trend towards an increase in the prevalence of OT among women is associated with an increase in the number of smokers among them, and the manifestation of clinical signs in them is often combined with damage to the hands.
Among the possible etiological causes, the participation of fungal and rickettsial infections is discussed - Rickettsia mooseri, Rickettsia burnetii.
Pathogenesis of ischemia of the upper extremities with systemic diseases comes down to inflammatory changes in the walls of the arteries, and with thromboangiitis obliterans - also in the veins (25-40%).
Damage to the arteries of the upper extremities with thromboangiitis obliterans is characterized by inflammatory changes in arteries of predominantly medium and small diameter. The most commonly observed distal form of the lesion involves the arteries of the forearm, palmar arches and digital arteries [Sultanov D.D., 1996; Machleder H.I., 1988; Fronek A., 1990]. They reveal mucoid swelling of the adventitia and intima, which leads to impaired blood supply and the appearance of ischemia. But damage to the proximal parts of the arteries of the upper extremities is also possible with this disease. In the literature there are isolated reports of isolated stenosis of the subclavian and axillary arteries.
Thromboangiitis obliterans is more common in young and middle-aged men ( middle age does not exceed 30 years), and recently there has been a tendency to increase
increasing incidence among women, and often the disease ends in amputation of the affected limb.
The appearance of ischemia of the upper extremities is usually preceded by ischemia of the lower extremities or migratory thrombophlebitis, although primary lesions hands Clinical manifestations of upper limb ischemia in OT begin with numbness or pain when working in the tips of the fingers or hand. 44% of patients with OT experience Raynaud's phenomenon.
Clinical signs of ischemia of the upper extremities are varied: from numbness and paresthesia to ulcerative-necrotic changes. There are several classifications of chronic ischemia of the upper extremities. A.V. Pokrovsky (1978) distinguishes 4 degrees of chronic ischemia of the upper extremities:
I degree - numbness, paresthesia;
II degree - pain when moving;
III degree- rest pain;
IV degree - trophic disorders.
IN International classification ischemia of the upper extremities, the last two degrees are combined into the concept of critical ischemia.
The severity of limb ischemia depends on the level of vascular damage, as well as on the degree of development of collaterals. The higher the level of occlusion, the more severe ischemia. An exception to this rule may be diseases affecting the distal parts of the limb (hand, fingers with OT, systemic scleroderma, periarteritis nodosa).
Migrating thrombophlebitis is one of the pathognomonic signs of OT and, according to various authors, occurs in 25-45% of patients. In 1/3 of cases, migratory thrombophlebitis is combined with pathological
gia of the arteries of the upper extremities. The initial clinical signs of upper extremity ischemia in OT are characterized by numbness or pain when working in the fingers or hand. As the disease progresses, as a rule, trophic changes appear, accompanied by necrosis of the distal phalanges, especially near the nail bed and under the nails, and intense pain. Pain mainly occurs in the distal form of the lesion and is caused by the involvement of nerve endings in inflammation. Often trophic disorders appear after minor injuries. Around the ulcers and necrosis, hyperemia and swelling of the fingers are noted, and a secondary infection is often associated. According to J. Nielubowicz (1980), 15% of patients first admitted to surgical hospitals undergo amputation on the upper extremities, but performing them during the active period of the disease is fraught with prolonged non-healing of the wound, which often leads to re-amputation for more high level. In this regard, before any surgical procedures, it is necessary to identify the activity of inflammation and prescribe anti-inflammatory therapy, including pulse therapy with cytostatics and hormonal drugs.
Diagnosis of ischemia of the upper extremities during OT. Assessment of the degree of ischemia of the upper extremities is largely determined by the clinical picture. Sometimes making the correct diagnosis depends on the results of a comprehensive analysis of the medical history and physical examination (palpation and auscultation of the arteries).
A physical examination must include external examination, palpation and auscultation of both upper extremities with blood pressure measurement on both sides. The pressure gradient across the arms should not exceed 15 mm Hg. V.K.Bumeister (1955), examined 500 healthy people, revealed
37% had the same blood pressure in both arms, a difference of 5 mm Hg. - in 42%, a difference of 10 mm Hg. - in 14% and 15 mmHg. - in 7% of those examined.
Ripple is determined at four points of the limb - in the axillary fossa, elbow bend and in the distal parts of the forearm, where the radial and ulnar arteries are located closest to the surface. It is also mandatory to determine the pulse on the radial artery during a test with the arm abducted posteriorly. A positive test is characteristic of neurovascular syndromes.
Mandatory in a clinical study is auscultation of the supra- and subclavian areas, while it has been experimentally proven and clinically confirmed that noise occurs when a vessel narrows by 60% of its cross-sectional area. The absence of noise does not exclude arterial occlusion.
By palpation of the supraclavicular and subclavian areas, pathological formations can be identified that may be the cause of compression of the subclavian artery.
Instrumental diagnostic methods. The similarity of clinical signs of disease of the arteries of the upper extremities often causes diagnostic errors and requires the use of a complex of instrumental methods, including duplex scanning, capillaroscopy, laser flowmetry, plethysmography, angiography, as well as laboratory research methods.
A significant role in assessing the degree of limb ischemia is played by determining the transcutaneous oxygen tension of the hand (TcPO 2). Normal values of TcP0 2 are over 50-55 mm Hg, TcP0 2 is within 40-45 mm Hg. is considered compensated, and the decrease in TcP0 2 of the hand is below 25 mm Hg. characteristic of critical ischemia.
Recently, an ever-increasing role in the diagnosis of lesions
arteries of not only the lower, but also the upper extremities are assigned to duplex scanning (DS), and data have appeared on the study of the distal parts of the arteries of the extremities, including DS of the arteries of the forearm, hand, fingers and even the nail bed during OT [Kuntsevich G.I., 2002], at the same time diagnostic criterion Thickening of arterial walls during OT was an increase in the value of the intima-media complex (IMC) of more than 0.5 mm, of the palmar arch and digital arteries - more than 0.4 and 0.3 mm, respectively, in combination with an increase in the echogenicity of the vessel wall. Prolonged thickening of the vascular wall with registration of a main-altered type of blood flow indicates the presence of hemodynamically significant stenosis.
The wide-field capillaroscopy method plays a role in the diagnosis of OT important role, especially in critical ischemia of the upper extremities, when strengthening of the subpapillary plexus and disruption of the course of capillaries are observed [Kalinin A.A., 2002] along with a decrease in their diameter and number.
More if necessary accurate diagnosis angiography is performed. Preference is given to selective angiography of the upper limb using the Seldinger technique. During arteriography of the upper limb, it is difficult to visualize the palmar and digital arteries due to possible spasm of the arteries upon injection contrast agent. This condition must be differentiated from arterial occlusion both large and small arteries. Therefore, before introducing a contrast agent, an antispasmodic (for example, papaverine) is injected into the arterial bed.
Laboratory diagnostics gives an idea of the activity of the inflammatory process in the body. Indicators of true OT activity are data humoral immunity- circulating immune complexes, immunoglobulins
we are M and G. In more than 60% of patients, the content of C-reactive protein in the blood increases. Its increase is also observed in active period inflammation. Accelerated ESR and leukocytosis are not always possible. The activity of the inflammatory process is a direct indication for anti-inflammatory therapy.
Differential diagnosis. Differential diagnosis of ischemia of the upper extremities during OT should be carried out with systemic vasculitis (systemic scleroderma, periarteritis nodosa), Raynaud's disease and syndrome, with ischemia of the upper extremities associated with occlusion of the subclavian artery in atherosclerosis and nonspecific aortoarteritis, as well as with ischemia of the arm in neurovascular diseases. syndromes.
In systemic scleroderma (SSc), progressive fibrosis of the blood vessels, skin of the hands and upper body is observed, as well as involvement of skeletal muscles and internal organs in fibrosis. An important link in the pathogenesis of the disease is a violation of microcirculation with proliferation and destruction of the endothelium, thickening of the wall and narrowing of the lumen of microvasculature vessels, vasospasm, aggregation of formed elements, stasis, and deformation of the capillary network. These changes lead to necrosis of the soft tissues of the fingertips. For scleroderma skin changes on the fingers are often similar to changes in other diseases. Raynaud's phenomenon is observed in 85% of patients with diffuse SSc. Most important feature scleroderma is atrophy of the skin and subcutaneous tissue, especially the fingers (so-called sclerodactyly), face and upper half torso, and to a lesser extent - lower extremities. The disease usually begins in the 3rd-4th decade of life. At the same time, of course
They become pale (“dead”) and then cyanotic. Sclerodactyly leads to ulceration of the fingertips and osteolysis of the nail phalanges. Simultaneously with external changes in scleroderma, the internal organs(pulmonary fibrosis, esophageal atrophy, gastric atony, possible pericarditis).
With Raynaud's disease, spasm of blood vessels in the fingers is observed in response to cold or emotional stimuli. As a rule, the localization of vascular attacks is symmetrical, with possible gangrene on the skin of the fingertips. Raynaud's disease is often accompanied by increased sweating in the distal parts of the affected limb.
It is extremely rare that spasm of large-diameter arteries (subclavian arteries) may occur when taking medications containing ergot. In modern practice, ergot is used to treat migraines or uterine bleeding.
Periarteritis nodosa is characterized by damage to both arteries and veins, the walls of which undergo fibrinoid necrosis and inflammatory changes involving all three layers. IN recent years Fixation of the HBs antigen in combination with immunoglobulins and complement was detected in the wall of the affected vessels.
Hand ischemia in neurovascular syndromes usually manifests itself as Raynaud's syndrome. An important diagnostic criterion for compression of the neurovascular bundle is a test with the arm abducted posteriorly. In this case, the disappearance of pulsation in the radial artery is observed.
A large group of patients have so-called occupational vascular diseases, which can lead to ischemia of the upper extremities. Arterial and venous injuries can occur both in everyday life and with excessive physical stress on the upper limbs. So, for example, long
exposure to vibration on the hand (pneumatic impact tools, saws, etc.) can lead to white finger syndrome due to vasospasm. If in initial period In patients, sensitivity disturbances and paresthesia are observed; in later stages, signs of Raynaud's syndrome predominate, and due to repeated vasospasm of the fingertips, these changes are similar to changes in scleroderma. In this case, resorption is observed bone structures in the distal phalanges or their secondary hypervascularization.
Exposure of tissue to high electrical voltage (over 1000 V) results in widespread tissue damage, but tissue necrosis or arterial thrombosis can occur anywhere between the point of entry and exit of the current.
In athletes, arm ischemia can be observed after an injury or as a result of performing a sharp and strong abduction of the arm - the so-called butterfly strike (swimmers, baseball players, etc.).
Treatment. In all patients, treatment begins with conservative measures, taking into account etiopathogenetic factors and parallel determination of inflammatory activity, as well as complete cessation of smoking.
Drug treatment It is advisable to prescribe depending on the degree of chronic ischemia. In case of I degree ischemia of the upper extremities, preference is given to drugs that improve microcirculation (trental, agapurin, prodectin), vasodilators (mydocalm, bupa-tol), myolytics (no-shpa, papaverine), B vitamins (B 1, B 6, B 12 ). It is possible to use physiotherapeutic procedures - hydrogen sulfide, radon, narzan baths, physical therapy. In case of II degree of ischemia of the upper extremities, conservative therapy. In addition to the above treatment measures, it is advisable to
but add intravenous infusions of rheopolyglucin solution - 400 ml with trental solution 10 ml daily for 10-15 days. In case of critical degree of ischemia of the upper extremities, in addition to standard antiplatelet therapy, the activity of inflammation is always determined.
An increase in humoral immunity (CIC, immunoglobulins M and G), C-reactive protein indicates the activity of inflammation, which requires the use of anti-inflammatory pulse therapy (cytostatics and hormonal drugs).
Anticoagulation therapy (aspirin - 10 mg/day, direct and indirect anticoagulants) is carried out depending on changes in coagulogram parameters.
Relief of critical ischemia is possible by prescribing intravenous infusions of prostaglandin E1 (vasaprostan) at a dose of 60 mcg/day for 20-30 days in combination with pulse therapy, depending on laboratory parameters. For trophic ulcers it is advisable to use local treatment, giving preference aqueous solution iodine (iodopyrone). There are reports of the effectiveness of Argosulfan cream.
Vasospastic conditions are most often treated with blockers calcium channels- nifedipine, but this does not apply to smokers and those who are sensitive to cold. Conservative treatment methods include intra-arterial administration of reserpine, infusion of prostaglandins, and plasmapheresis.
If conservative treatment is ineffective and there is a threat of loss of the upper limb, surgical interventions are performed. Indications for surgery for chronic arterial obstruction include dysfunction of the limb, pain of movement and rest, trophic disorders and acute ischemia.
Angiography and duplex scanning data are determined
dividing in the tactics of surgical treatment.
For proximal lesions subclavian arteries More often, it is not arm ischemia that is observed, but steal syndrome, so all operations are aimed primarily at eliminating cerebral ischemia, and arm ischemia is of a secondary nature. These operations can be divided into intra- and extrathoracic (see Chapter 5).
For non-prolonged occlusions brachial artery or arteries of the forearm, it is possible to perform standard bypass operations. As a shunt, preference is given to an autologous vein if it does not show signs of inflammation. Otherwise, synthetic prostheses are used.
Unfortunately, the long-term results of using standard bypass operations for OT leave much to be desired. This is primarily due to the poor condition of the outflow tract and relapses of the inflammatory process, which leads to stenosis in the anastomosis area. Of no small importance in improving the results of surgical treatment is preoperative and, if necessary, postoperative immunosuppressive therapy.
Surgical treatment of lesions of the arteries of the forearm and hand remains controversial, because the absence or poor distal flow limits the use of standard reconstructive operations.
If in the 50s of the last century, with distal forms of damage to the arteries of the upper extremities, conservative and palliative surgical methods came to the fore, then at present, with distal forms of damage, in order to save the limb, it is possible to perform non-standard treatment methods - arterialization of the venous blood flow in the hand [Pokrovsky A.V., Dan V.N., 1989], transplantation of the greater omentum, osteotra-
Panation of the bones of the forearm. The latter method is effective only for stage II ischemia.
The technique of arterialization of the venous blood flow of the hand is reduced to the imposition of an arteriovenous fistula between the unchanged arterial section proximal to the site of occlusion and the superficial or deep venous system brushes
An important role in the treatment of upper limb ischemia is played by thoracic sympathectomy (more recently endoscopic). A positive reactive hyperemia test is an indication for thoracic sympathectomy, in which 2 or 3 upper thoracic ganglia are removed. According to some data, the effectiveness of sympathectomy in OT is quite high: its use reduces pain syndrome and reduces the rate of amputation [Betkovsky B.G., 1972; Alukhanyan O.A., 1998; Ishibashi H., 1995].
For systemic diseases, preference is given to conservative treatment methods, although in some cases periarterial or cervical sympathectomy is effective. R.Go-mis reports the effectiveness of periarterial sympathectomy for OT, Raynaud's syndrome and even periarteritis nodosa.
Diagnostic errors associated with underestimation of the manifestations of scleroderma often lead to incorrect treatment tactics. For example, in case of Raynaud's syndrome, which is a sign of scleroderma, and the presence of scalenus syndrome, scalenotomy is unacceptable due to the worsening of the scarring process in the area of the operation, which will inevitably lead to an increase in the severity of Raynaud's syndrome itself. Such patients require conservative treatment in specialized rheumatology departments.
The combination is required conservative methods treatment with surgical interventions. For example, with OT, first of all
it is necessary to eliminate the activity of inflammation using pulse therapy, and then carry out surgical intervention.
Forecast. At the right approach The prognosis for treatment of this category of patients is favorable. The main conditions for the effectiveness of treatment are timely prevention of inflammation and complete cessation of smoking.
Literature
Alukhanyan O.A. The first experience of using video-assisted thoracoscopic upper thoracic sympathectomies in the treatment of vascular disease/"/3rd International Congress of Nordic Countries and Regions. - 1998.
Baranov A.A., Shilkina N.P., Nasonov E.L. Hyperproduction of immunoglobulin E during obliterating diseases peripheral arteries//Wedge. med.-1991.-T.69,
No. 4.-P.45-48.
Beloyartsev D. F. Results of surgical treatment of proximal lesions of the branches of the aortic arch in atherosclerosis: Abstract of thesis. dis. ... Doctor of Medical Sciences - M., 1999. Kalinin A.A. Diagnosis and treatment of occlusive lesions of the arteries of the upper extremities in patients with thromboangiitis obliterans: Abstract of thesis. dis. Candidate of Medical Sciences - M., 2002. - 24 p.
Kuntsevich G.I., Shutikhina I.V., Ter-Khachatu-rova I.E., Kalinin A.A. Examination of the vessels of the nail bed using duplex scanning in a group of practically healthy individuals//Proceedings of the conference on ultrasound diagnostics dedicated to the 10th anniversary of the Department of Ultrasound Diagnostics of the Russian Medical Academy of Postgraduate Education of the Ministry of Health of the Russian Federation//Ultrasound Diagnostics.-2002.-No. 2.-P.286.
Petrovsky B.V., Belichenko I.A., Krylov V.S. Surgery of the branches of the aortic arch.-M.: Medicine, 1970.
Pokrovsky A.V., Dan V.N., Chupin A.V., Kalinin A.A. Combined treatment of critical ischemia of the upper extremities in patients with thromboangiitis obliterans // Proc. scientific Conf.-M., 2001. Sultanov D.D., Khodzhimuradov G.M., Rakhimov A.B. Surgical treatment of peripheral occlusion of arteries of the upper extremities // Thoracic and cardiovascular surgery. - 1996.-P.319.
Chupin A.V. Diagnosis and treatment of critical ischemia of the lower extremities in patients with thromboangiitis obliterans: Abstract of thesis. dis. ...Dr. med. nauk.-M., 1999. Yarygin N.E., Romanov V.A., Lileeva M.A. Clinical morphological features thromboangiitis obliterans//Actual-
important issues of diagnosis, treatment and medical examination of patients with rheumatic diseases: Sat. scientific tr. Yaroslavl State Medical Institute. - 1988.-P.111-114. Aerbajinai W. HLA class II DNA typing in Buerger's disease//Int.J.Cardiol. - 1997. - Vol.54. - Suppl. - S. 197. Ala-Kulju K, Virkkula L. Use of omental pedicle for treatment of Buerger's disease affecting the upper extremities//Vasa. - 1990. - Vol 19, N 4. - P.330 - 333.
Bergau J.J., Conn J., Trippel O.H. Senere ischemia of the hand//Ann.surg. - 1972 .- Vol.73. - P.301.
Bergquist D., Ericsson B.F., Konrad P., Bergentz S.S. Arterial surgery of the upper extremity//World J.Surg. - 1983. - Vol.7, N 6. -P.786-791.
Femandes Miranda C et al. Thromboangiitis obliterans (Buerger's disease). Study of 41 cases (commenty/Med.clin.Barc. - 1993.- Vol.25, N 9.-P.321-326.
Gordon R., Garret H. Atheromatous and aneurysmal disease of upper extremity arteries//Vas-cular Surgery/Ed.R.Rutherford. - Philadelphia, 1984. - P.688-692. Ishibashi H., Hayakawa N., Yamamoto H. et al. Nimura Thoracoscope sympathectomy for Buerger's desease: a report on the successful treatment of four patients. Department of Surgery, Tokai Hospital, Nagoya, Japan. SOURCE: Surg Today, 1995. - Vol.25(2). -P.180- 183. Izumi Y. et al. Results of arterial reconstruction in Buerger's disease//Nippon-Geca-Gakkai-Zasshi. - 1993. - Vol.94, No. 7. - P.751-754. Machleder H.L. Vaso-occlusive disorders of the upper extremity//Curr.problems in Durg. - 1988. - Vol.25(l). - P.l-67. Mills J.L., Friedman E.I., Porter J.M. Upper extremity ichemia caused by small artery dis-ease//Amer.J.Surg. - 1987. - Vol.206, N 4. -P.521-528.
Nielubowicz J., Rosnovski A., Pruszynski B. et al. Natural history of Buerger's disease//J.Cardio-vasc.Surg. - Vol.21. - P.529-540. | | | | | 24 | | | | | | | | | |
OAN is an urgent pathology that usually requires immediate surgical in rare cases, conservative treatment. Arterial insufficiency of the lower extremities may be caused for various reasons and in any case is accompanied by acute ischemic syndrome which poses a threat to human life.
Causes of arterial insufficiency
In the diagnosis of OAN, three main terms should be distinguished:
Embolism is a condition when occlusion of the lumen of an artery occurs with a fragment of a thrombus that is transported with the bloodstream (in this case the thrombus is called an embolus).
Acute thrombosis is a condition characterized by the development of a blood clot, which is formed as a result of pathology of the vascular wall and closes the lumen of the vessel.
Spasm is a condition characterized by compression of the lumen of the artery as a result of internal or external factors. As a rule, this state typical for arteries of muscular or mixed type.
Photos of diagnosing obstruction of the arteries of the lower extremities
In the majority clinical cases, etiological factor development of embolism is a cardiac pathology, which includes various types cardiopathy, myocardial infarction, heart changes as a result of rheumatic processes. We should not forget the fact that, regardless of the type of cardiac pathology, violations are of great importance in the occurrence of embolism heart rate. Unlike embolism, the main cause of thrombosis is atherosclerotic changes in the artery wall. The cause of the spasm, as mentioned above, is the impact external factor(trauma, shock, hypothermia). Less often - internal factor(inflammation of surrounding tissues).
Diagnosis of arterial insufficiency of the arteries of the extremities
In diagnosing the condition acute obstruction arteries there are 5 main symptoms:
- Pain in the limbs. As a rule, the first symptom noted by the patient himself.
- Sensory impairment. The patient notes a feeling of “pins and needles”, as if he had been sitting on his leg. In more difficult situations impaired sensitivity can be expressed before the state of anesthesia, when the patient does not feel his limb.
- Change skin. From slight pallor to pronounced cyanosis.
- Absence of pulsation of the artery below the level of the lesion. As a rule, this symptom is fundamental in diagnosing the development of OAN.
- Decreased temperature of the affected limb.
When interviewing the patient, you need to pay attention to the timing of the onset of the above symptoms and the nature of their course. A carefully collected anamnesis can help in making a diagnosis and further successful treatment ischemia of the lower extremities. Embolism is characterized by a sudden onset of the disease with rapid development pictures of arterial insufficiency. In the case of thrombosis, the development of the disease, as a rule, is less severe.
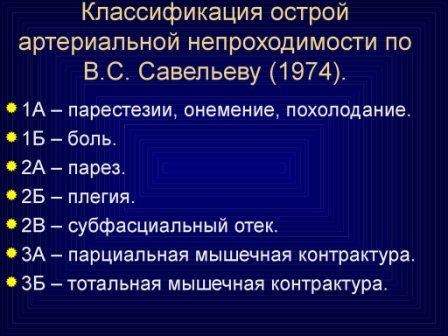 Classifications of obstruction of the lower extremities according to Savelyev
Classifications of obstruction of the lower extremities according to Savelyev In the diagnosis of acute thrombosis of the arteries of the lower extremities, when interviewing the patient, he may note that before, he experienced rapid leg fatigue, pain in calf muscles upon exertion, a feeling of numbness in the limbs. These symptoms are characteristic of chronic arterial insufficiency of the vessels of the lower extremities and indicate atherosclerotic damage to the arteries.
In addition to a physical examination and history taking, a significant role is played in making a diagnosis. instrumental methods diagnostics The main diagnostic method is Doppler ultrasound. It allows you to differential diagnosis causes of OAN, clarify the location of the lesion, assess the nature of the damage to the arterial wall, decide on tactics further treatment patient.
Useful article:
Another method for diagnosing vascular lesions is angiography. Difference this method is its “invasiveness”, the need to use radiopaque agents, and its use also requires certain preparation of the patient. Therefore the application ultrasound diagnostics in acute arterial insufficiency is more preferable.
Classification of acute ischemia of the lower extremities according to Savelyev
After diagnosis, an important task is to determine the degree of ischemia of the lower extremities. IN present moment the classification created by V.S. is used. Savelyev. Knowledge of the classification is vital when deciding on the tactics of surgical intervention in the treatment of acute arterial insufficiency of the lower extremities. Also knowing the degree of blood flow disturbance, the doctor has an idea of the urgency of the operation itself and the possibility of additional preoperative preparation.
 Rutherford classification for the diagnosis of acute arterial insufficiency of the lower extremities
Rutherford classification for the diagnosis of acute arterial insufficiency of the lower extremities So, there are 3 degrees of acute ischemia:
1 tbsp. – pain in the limb, numbness, coldness, feeling of paresthesia;
2a art. – active movement disorder;
2b art. – active movements absent;
2v art. – subfascial edema of the limb;
3a art. – partial muscle contracture;
3b art. – complete muscle contracture;
With the first two degrees of ischemia (1 and 2A), the doctor still has the opportunity to delay surgery for up to 24 hours, for the purpose of additional examination, or additional preparation of the patient for surgery. With a more severe degree of ischemia, surgical intervention comes to the fore and postponing the operation is possible only with a degree of ischemia of 2B (for 2 hours).
It is important to remember that the main treatment method for acute arterial insufficiency in the development of embolism or acute thrombosis is surgical repair main blood flow. The volume of the operation, the tactics of performing the intervention, and the method of anesthesia are determined by the surgeon individually for each patient. It is possible to use both open surgical treatment: embolectomy, thrombectomy from a typical approach, bypass surgery, and X-ray endovascular treatment, if the necessary instruments are available.
Conservative treatment of acute arterial insufficiency of the lower extremities is possible with timely initiation of anticoagulant, antiplatelet and antispasmodic therapy, the presence of good collateral blood flow. In this case, it is possible to “dissolve” (lysis) the thrombus, or compensate for blood flow due to collaterals.
At 1 tbsp. – 2nd stage of ischemia, restoration of blood flow is possible. In more severe forms, the only surgical treatment is amputation of the limb. Despite the technical possibility of restoring vascular patency, decay products induced by limb ischemia, when released into the main bloodstream, can provoke complications (for example, the development of acute renal failure), the consequences of which are much worse than the loss of the limb itself. Chances fatal outcome in this case they increase significantly.
 Photo of ischemia of the lower extremities during treatment
Photo of ischemia of the lower extremities during treatment Acute arterial insufficiency limbs is not as common a pathology as stroke or myocardial infarction. However, knowledge of symptoms and tactics treatment of this disease is important for both ordinary person, and for medical specialist, regardless of the latter's profile. life directly depends physical activity person.

