Congenital heart defects (CHD) in children: causes, symptoms, diagnosis and treatment. Patterns of changes in ultrasound examination parameters for congenital heart defects in the fetus depending on the characteristics of intracardiac hemodynamics antenatal
As you know, the heart is important organ in the human body, the well-being of the entire organism depends on its proper functioning. The heart consists of muscle (myocardium) and connective tissue(heart valves, walls large vessels). The activity of the heart is due to the rhythmic and consistent contraction of its constituent structures (atria and ventricles), as a result of which the blood flowing through the lungs is saturated with oxygen (the so-called pulmonary circulation) and distributes oxygen to all organs and tissues (systemic circulation).
As the fetal heart develops during pregnancy, it works differently from the heart of a newborn baby or an adult. In particular, the pulmonary circulation begins to function fully only during childbirth, when the newborn’s lungs open and at the moment of the first cry they fill with blood. Therefore, there are special holes and ducts in the fetal heart that allow blood to circulate in the developing body, bypassing the lungs ( ductus arteriosus connecting the aorta and pulmonary artery, oval window between the atria, ductus venosus between umbilical vein and inferior vena cava).
Sometimes under the influence unfavorable factors during the period intrauterine development Gross disturbances in the formation of the anatomical structures of the heart occur, which affects its activity and is not always compatible with the life of the child. Then, either by ultrasound of the fetus during pregnancy or in the first days after birth, the newborn is diagnosed congenital heart defect. What is it, what is the prognosis for life and what methods does it offer to preserve the life and health of such babies? modern medicine, we will try to find out in this article.
So these pathological conditions represent a large group of heart diseases, united by the following characteristics:
Occurs during intrauterine development;
- characterized by gross violations of the architectonics of the heart and large vessels (aorta, inferior and vena cava, pulmonary artery and veins);
- anatomical changes cause significant disturbances in hemodynamics (blood circulation throughout the body);
- caused by underdevelopment of anatomical structures or changes in them normal location in the heart.
The prevalence rate varies from 6 to 9 per 1000 live births. According to various authors, possible options There are between 50 and 100 congenital heart defects.
Schematic representation of some heart defects
Causes of congenital heart defects
Due to the fact that during intrauterine development there is an active formation of all organs human body, especially the heart, the fetus and the pregnant woman are vulnerable to the effects of various negative factors. Thus, the abnormal course of organogenesis can be influenced by increased background radiation, ionizing radiation, infectious diseases mothers, especially viral ones - rubella, measles, chickenpox, herpes; taking certain medications and toxic substances(drugs, alcohol) during pregnancy, especially in the first trimester (8-12 weeks - the period of the most intensive formation of all fetal organs). In 4–10% of cases, congenital defects are genetically determined, that is, inherited.
Symptoms of congenital heart defects
The clinical symptoms of defects depend on their type. There are defects of the “blue” and “white” types, as well as defects that create an obstacle to blood flow.
The main manifestation "blue" vices(transposition (change of location) main arteries, tetralogy of Fallot, atresia - fusion - of the tricuspid valve) is cyanosis - blue discoloration of the skin of the fingers, hands, feet, nasolabial triangle, ears, nose or, in extremely severe cases, the entire body. Also, manifestations of arterial hypoxemia (low oxygen levels) are shortness of breath, loss of consciousness with or without convulsions, tachycardia (rapid heartbeat), retardation in growth and development, frequent colds, neurological symptoms due to the lack of normal blood supply to the brain. As a rule, defects of this type manifest themselves already in the first hours and days of a newborn child’s life. Transposition of the great arteries (vena cava enters the left, not right atrium, and the aorta arises from the right, not the left, ventricle) is a severe defect incompatible with life, and the child, as a rule, dies immediately after birth. Also, defects incompatible with life include a three-chambered heart (two atria and one ventricle, or one atrium and two ventricles). The mortality rate of defects of this type is very high; if children with such defects survive in the first days of life, then without treatment they die by the end of the first or second year.
TO white type defects include defect interventricular septum, open Botallov (arterial) duct, defect interatrial septum. Clinically, these defects may begin to manifest themselves not in early childhood, but by 16–20 years. Symptoms of white type defects are as follows: pallor skin, developmental delay, frequent acute respiratory viral infections, signs of developing right ventricular failure - shortness of breath and tachycardia during exercise or at rest.
Defects with obstruction to blood flow: stenosis (narrowing of the lumen) of the aorta, coarctation (segmental narrowing) of the aorta, pulmonary artery stenosis are clinically manifested by shortness of breath, tachycardia, pain in the chest, decreased endurance, edema, developmental delays and poor circulation of the lower half of the body. With coarctation of the aorta, children survive to a maximum of 2 years of age.
Diagnosis of congenital heart defects
As a rule, it is possible to diagnose fetal malformations, including heart defects, even at the stage ultrasound examination pregnant woman. Then, depending on the type of defect, the woman may be recommended to either terminate the pregnancy (for defects incompatible with life, for multiple deformities, etc.), or continue the pregnancy with a more detailed examination of the pregnant woman and resolve the issue of surgical treatment of the child immediately or some time after birth. But sometimes due to some reasons (not visiting a pregnant woman antenatal clinic and ultrasound room, insufficient equipment of medical and obstetric stations with ultrasound equipment, etc.) developmental defects can be diagnosed only after childbirth.
Despite the fact that the symptoms of congenital defects are quite clear, in the process clinical examination In a newborn child, the diagnosis can only be assumed, since many symptoms are not strictly specific and may be due to other severe conditions of newborns ( respiratory distress syndrome, intracranial hemorrhages etc.). Also, not all defects can give a characteristic auscultatory picture (in the process of listening to the chest), and vice versa, noises, clicks or other auscultatory manifestations can occur with minor deviations from the norm in the structure of the heart (minor anomalies). Therefore, if a heart defect was not diagnosed by fetal ultrasound, all children with symptoms of circulatory disorders (diffuse or acrocyanosis, shortness of breath during feeding or at rest, loss of consciousness, convulsions) should undergo a cardiac ultrasound during their stay in the maternity hospital.
Echocardiography (ultrasound of the heart) is one of the most informative methods visualization of heart defects. An ECG may also be prescribed (it will show rhythm disturbances, hypertrophy of the atria and/or ventricles, if any), and a chest x-ray (it will show stagnation of blood in the lungs, if any, an increase in the shadow of the heart due to the expansion of its chambers). In particular difficult cases or before surgical treatment, ventriculography (introduction of a radiopaque substance into the cavity of the ventricles of the heart), angiography (introduction of contrast through the vessels in the heart cavity), and probing of the chambers of the heart with measurement of pressure in them may be prescribed.
Now let’s take a closer look at ultrasound diagnostics of common heart defects.
A. Congenital spankings heart with volume overload of blood vessels in the lungs (pulmonary circulation).
1. Atrial septal defect - with the help of one-dimensional echocardiography, signs of volume overload and dilatation (expansion) of the right ventricle are revealed, with two-dimensional echocardiography a break in the echo signal between the atria is visible, and with a Doppler study, the turbulent (with “vortices”) blood flow through the interatrial septum and the degree of pulmonary blood flow disorders.
2. Ventricular septal defect - when performing an ultrasound of the heart, a hole in the septum between the ventricles, dilatation of the left and right ventricles, turbulent blood flow from the left to the right ventricle are visualized, the severity of pulmonary hypertension is assessed, and the pressure difference in the ventricles is measured.

This is how a defect in the septum between the ventricles manifests itself during echocardiography with Doppler. On the left is a normal interventricular septum, on the right is its defect (VSD).
3. Patent ductus Botall - manifested on echocardiography by continuous blood flow through communication in the aorta and pulmonary artery, a change in blood flow at the mouth of the pulmonary trunk.
4. Coarctation of the aorta – a segmental area of narrowing of the aortic lumen is visible, accelerated blood flow below the segment.
5. Transposition of the great arteries - the incorrect departure of the vessels from the heart is visualized.
B. Heart defects with a decrease in blood volume in the pulmonary circulation.
1. Tetralogy of Fallot - with echocardiography, in addition to stenosis (narrowing) of the pulmonary artery and a septal defect between the ventricles, hypertrophy of the right ventricle and the origin of the aorta from the right ventricle are determined, and the degree of violation is also assessed intracardiac hemodynamics.
2. Pulmonary artery stenosis - narrowing of the lumen of the pulmonary artery is detected, and acceleration of blood flow at the mouth of the pulmonary artery and hypertrophy of the right ventricle.
3. Epstein's anomaly is a pathology of the development of the tricuspid heart valve, when the valve leaflets are attached not to the fibrous ring between the atrium and the ventricle on the right, but to the walls of the right ventricle, which causes a decrease in its volume. With ECHO-CG, valve pathology is determined, the degree of expansion of the heart cavities and disturbances in intracardiac blood flow are assessed.
4. Atresia of the tricuspid valve - with ECHO-CG there is no reflection of the echo signal from the tricuspid valve, hypertrophy of the right atrium and left ventricle is recorded.
B. Heart defects with a decrease in the volume of circulating blood in the systemic circulation (in the vessels of all vital organs).
1. Coarctation of the aorta (see above).
2. Isolated aortic stenosis - the degree of narrowing is assessed, accelerated blood flow through the aortic valve and deformed valve leaflets is visualized.
D. Heart defects without hemodynamic disturbances.
- Dextrocardia (mirror position of the heart on the right) is a fairly rare anomaly; hemodynamic disturbances are usually not recorded by ultrasound of the heart.
Treatment of congenital heart defects
Complete cure of the vast majority of heart defects is possible only with the help of their surgical correction. Cardiac surgery can be performed in the first hours or days of a newborn’s life, or in the first year of a child’s life. With a patent ductus arteriosus, expectant management is acceptable (in the absence of symptoms of life-threatening conditions), since this duct can close on its own in the first two years of life.
Operations can be performed either on open heart(with dissection of the chest wall), and the cardiovascular method (when access to the heart is carried out by introducing a probe into the vessels that reaches the cavities of the heart). Last method, for example, is used to correct defects between the atria or ventricles, to which an occluder is applied using a probe to close the holes.
But for some heart defects that are incompatible with life, for example, a three-chambered heart (one atrium and two ventricles, or two atria and one ventricle), surgical correction, unfortunately, is not possible.
In addition to cardiac surgery, the patient is prescribed drug therapy to improve contractile function heart and “unloading” of the pulmonary circulation. ACE inhibitors (enalapril, perindopril, lisinopril, ramipril, etc.), diuretics (furosemide, indapamide, etc.), B-blockers (carvedilol, bisoprolol, etc.) are used.
Lifestyle with congenital heart disease
The patient must comply the following recommendations regarding his lifestyle:
- rational balanced nutrition;
- following a restricted diet table salt and the volume of fluid consumed (to reduce volume overload of the heart and blood vessels);
- sufficient exposure to fresh air;
- exclusion of any sports activities and limitation of strong physical activity;
- sufficient sleep duration;
- regular observation by a cardiologist and cardiac surgeon with the necessary therapeutic and diagnostic measures;
- pregnancy for women with “blue” type defects is strictly contraindicated, but if surgical treatment, then the possibility of maintaining pregnancy is determined in each specific case individually with joint management of the pregnant woman by a cardiac surgeon, cardiologist and obstetrician-gynecologist in a specialized hospital. Delivery is usually carried out by caesarean section.
Prognosis for congenital heart defects
The life prognosis for most heart defects is unfavorable. As mentioned above, cardiac surgery treatment such babies need it in the first days and months after birth, otherwise they die within the first two years due to the progression of heart failure or complications ( bacterial endocarditis, fatal arrhythmias, increased risk thrombus formation and thromboembolic complications, frequent illnesses bronchopulmonary system(prolonged bronchitis, severe pneumonia). The exception is white type defects, in which, in the absence of surgical treatment for any reason, children are able to live up to 16–18 years.
After surgical correction, the prognosis for life is favorable, but still the child’s condition remains quite serious, so such children should be closely monitored by parents and doctors.
In conclusion, I would like to note that this diagnosis in a child is modern stage development of medicine is not a death sentence, since the capabilities of domestic and foreign pediatric cardiology make it possible to bear, give birth and raise a baby who is able to lead a full life, despite such a serious illness.
General practitioner Sazykina O.Yu.
One of the most commonly diagnosed developmental anomalies cardiovascular system in children it is considered a congenital heart defect. Such an anatomical disorder of the structure of the heart muscle, which occurs during the period of intrauterine development of the fetus, threatens with serious consequences for the health and life of the child. Timely medical intervention can help avoid a tragic outcome due to congenital heart disease in children.
The task of parents is to navigate the etiology of the disease and know about its main manifestations. In force physiological characteristics In newborns, some heart pathologies are difficult to diagnose immediately after the baby is born. Therefore, you need to carefully monitor the health of a growing child and respond to any changes.
Classification of congenital heart defects in children
Congenital heart disease provokes disruption of blood flow through the vessels or in the heart muscle.
The earlier a congenital heart defect is detected, the more favorable the prognosis and outcome of treatment of the disease.
Depending on external manifestations Pathologies distinguish the following types of congenital heart disease:
- "White" (or "pale") defects
Such defects are difficult to diagnose due to the lack obvious symptoms. A characteristic change is the pallor of the child’s skin. This may signal the arrival insufficient quantity arterial blood into tissue.
- "Blue" vices
 The main manifestation of this category of pathology is blue discoloration of the skin, especially noticeable in the area of the ears, lips and fingers. Such changes are caused by tissue hypoxia, provoked by the mixing of arterial and venous blood.
The main manifestation of this category of pathology is blue discoloration of the skin, especially noticeable in the area of the ears, lips and fingers. Such changes are caused by tissue hypoxia, provoked by the mixing of arterial and venous blood.
The group of “blue” defects includes transposition of the aorta and pulmonary artery, Ebstein’s anomaly (displaced place of attachment of the tricuspid valve leaflets to the cavity of the right ventricle), tetralogy of Fallot (the so-called “cyanotic disease”, a combined defect combining four pathologies - stenosis of the outflow tract of the right ventricle , dextraposition of the aorta, high and hypertrophy of the right ventricle).
Considering the nature of circulatory disorders, congenital heart defects in children are classified into the following types:
- Message with blood discharge from left to right (patent ductus arteriosus, ventricular or atrial septal defect).
- Message with blood discharge from right to left (tricuspid valve atresia).
- Heart defects without shunting (stenosis or coarctation of the aorta, pulmonary stenosis).
Depending on the complexity of the violation of the anatomy of the heart muscle, such congenital heart defects are distinguished into childhood:
- simple defects (single defects);
- complex (a combination of two pathological changes, for example, narrowing of the cardiac orifices and valvular insufficiency);
- combined defects (combinations of multiple anomalies difficult to treat).
Causes of pathology
Impaired differentiation of the heart and the appearance of congenital heart disease in the fetus are provoked by exposure to unfavorable factors environment on a woman during pregnancy.
The main reasons that can cause cardiac abnormalities in children during their intrauterine development include:
- genetic disorders (chromosome mutation);
- smoking, consumption of alcohol, narcotic and toxic substances by a woman during pregnancy;
- suffered during pregnancy infectious diseases(rubella and influenza virus, chickenpox, hepatitis, enterovirus, etc.);
- unfavorable environmental conditions (increased background radiation, high level air pollution, etc.);
- use of medications that are prohibited during pregnancy (including medications whose influence and side effects not sufficiently researched);
- hereditary factors;
- somatic pathologies of the mother (primarily diabetes mellitus).
These are the main factors that provoke the occurrence of heart disease in children during their prenatal development. But there are also risk groups - children, born of women over 35 years of age, as well as those suffering from endocrine dysfunctions or toxicosis of the first trimester.
Symptoms of congenital heart disease
Already in the first hours of life children's body may signal abnormalities in the development of the cardiovascular system. Arrhythmia, rapid heartbeat, difficulty breathing, loss of consciousness, weakness, bluish or pale skin indicate possible pathologies hearts.
But symptoms of congenital heart disease may appear much later. Parental concerns and immediate appeal for medical care should cause the following changes in the child’s health:
- blueness or unhealthy pallor of the skin in the area of the nasolabial triangle, feet, fingers, ears and face;
- difficulty feeding the child, poor appetite;
- delay in weight and height gain in the baby;
- swelling of the limbs;
- increased fatigue and drowsiness;
- fainting;
- increased sweating;
- shortness of breath (constant difficulty breathing or temporary attacks);
- changes in heart rate independent of emotional and physical stress;
- heart murmurs (determined by listening to a doctor);
- pain in the heart, chest.
In some cases, heart defects in children are asymptomatic. This makes it difficult to identify the disease in its early stages.
 Regular visits to the pediatrician will help prevent the worsening of the disease and the development of complications. During each routine examination, the doctor must listen to the sound of the child’s heart sounds, checking for the presence or absence of murmurs - nonspecific changes that are often functional in nature and do not pose a threat to life. Up to 50% of murmurs detected during a pediatric examination may be accompanied by “minor” defects that do not require surgical intervention. In this case, regular visits, monitoring and consultations with a pediatric cardiologist are recommended.
Regular visits to the pediatrician will help prevent the worsening of the disease and the development of complications. During each routine examination, the doctor must listen to the sound of the child’s heart sounds, checking for the presence or absence of murmurs - nonspecific changes that are often functional in nature and do not pose a threat to life. Up to 50% of murmurs detected during a pediatric examination may be accompanied by “minor” defects that do not require surgical intervention. In this case, regular visits, monitoring and consultations with a pediatric cardiologist are recommended.
If the doctor doubts the origin of such noises or observes pathological changes sound, the child must be sent for a cardiac examination. Pediatric cardiologist listens to the heart again and prescribes additional diagnostic studies in order to confirm or refute a preliminary diagnosis.
Manifestations of the disease in to varying degrees Difficulties do not only occur in newborn children. Vices can make themselves felt for the first time already in adolescence. If a child who outwardly looks absolutely healthy and active, shows signs of developmental delay, has blue or painful pale skin, shortness of breath and fatigue even from light exertion, then an examination by a pediatrician and consultation with a cardiologist is necessary.
Diagnostic methods
To study the condition of the heart muscle and valves, as well as to identify circulatory abnormalities, doctors use the following methods:
- Echocardiography is an ultrasound examination that allows one to obtain data on the pathologies of the heart and its internal hemodynamics.
- Electrocardiogram – diagnosis of heart rhythm disturbances.
- Phonocardiography is the display of heart sounds in the form of graphs, allowing you to study all the nuances that are not available when listening with the ear.
- with Doppler - a technique that allows the doctor to visually assess blood flow processes, the condition of the heart valves and coronary vessels by attaching special sensors to the patient's chest area.
- Cardiorhythmography is a study of the characteristics of the structure and functions of the cardiovascular system, its autonomic regulation.
- Cardiac catheterization - inserting a catheter into the right or left chambers of the heart to determine the pressure in the cavities. During this examination, ventriculography is also performed - X-ray examination chambers of the heart with the introduction of contrast agents.
Each of these methods is not used by a doctor in isolation - the results are compared to accurately diagnose the pathology various studies, allowing to establish the main hemodynamic disorders.
 Based on the data obtained, the cardiologist determines the anatomical variant of the anomaly, clarifies the phase of the course, and predicts probable complications heart defect in a child.
Based on the data obtained, the cardiologist determines the anatomical variant of the anomaly, clarifies the phase of the course, and predicts probable complications heart defect in a child.
If there were heart defects in the family of any of the future parents, the woman’s body during the period of bearing the child was subjected to at least one of hazardous factors or unborn child be at risk possible development congenital heart disease, then the pregnant woman should notify the obstetrician-gynecologist who is observing her about this.
The doctor, taking into account such information, should special attention look for signs of cardiac abnormalities in the fetus, apply all possible measures diagnosis of the disease in the prenatal period. Task expectant mother– undergo ultrasound and other examinations prescribed by the doctor in a timely manner.
The best results with accurate data on the state of the cardiovascular system gives the latest equipment for the diagnosis of childhood heart defects.
Treatment of congenital heart disease in children
Congenital heart abnormalities in childhood are treated in two ways:
- Surgical intervention.
- Therapeutic procedures.
![]() In most cases, the only possible chance to save a child’s life is the first radical method. The fetus is examined for the presence of pathologies of the cardiovascular system even before it is born, so most often the issue of prescribing an operation is decided during this period.
In most cases, the only possible chance to save a child’s life is the first radical method. The fetus is examined for the presence of pathologies of the cardiovascular system even before it is born, so most often the issue of prescribing an operation is decided during this period.
In this case, childbirth is carried out in specialized maternity wards operating at cardiac surgery hospitals. If the operation is not performed immediately after the birth of the child, surgical treatment is prescribed as soon as possible. short terms, preferably in the first year of life. Such measures are dictated by the need to protect the body from the development of possible life-threatening consequences of congenital heart disease - heart failure, etc.
Modern cardiac surgery involves open-heart surgery, as well as using catheterization techniques, supplemented by X-ray imaging and transesophageal echocardiography. Elimination of cardiac defects is effectively carried out using balloon plasty, endovascular treatment (methods of inserting walls and sealing instruments). In combination with surgical intervention, the patient is prescribed medicines, increasing the effectiveness of treatment.
Therapeutic procedures are auxiliary method combat the disease and are used when it is possible or necessary to reschedule the operation for a later late dates. Therapeutic treatment often recommended for “pale” defects, if the disease does not develop rapidly over months and years and does not threaten the child’s life.
During adolescence, acquired heart defects in children can develop - a combination of corrected defects and newly emerging anomalies. Therefore, a child who has undergone surgical correction of pathology may later need repeated surgery. Such operations are most often performed using a gentle, minimally invasive method in order to eliminate the burden on the psyche and body of the child as a whole, and also to avoid scars.
When treating complex heart defects, doctors do not limit themselves to corrective methods. In order to stabilize the child’s condition, eliminate the threat to life and maximize its duration for the patient, a number of step-by-step steps are required. surgical interventions ensuring adequate blood supply to the body and the lungs in particular.
Timely detection and treatment of congenital and heart diseases in children enables the majority of young patients to fully develop, lead active image life, support healthy condition body and not feel disadvantaged morally or physically.
Even after successful surgery and the most favorable medical prognosis, the main task of parents is to ensure that the child has regular visits and examinations by a pediatric cardiologist.
Congenital defects hearts rarely affect fetal development. This was first noted in the studies of B. Mac Mahon et al. . However, there are defects that are incompatible with life, and after birth the child immediately dies. Some congenital heart defects, even simple forms, in the early neonatal period are malignant, causing the development of circulatory decompensation and respiratory failure. The main reason This is due to the imperfection of compensatory mechanisms.
Diagnosis of the fetus is one of the most difficult tasks of perinatology. Many congenital heart defects, even complex ones, practically incompatible with life, do not manifest themselves antenatally due to the peculiarities of intracardiac hemodynamics and after birth become a disaster for the child’s life.
The antenatal period is characterized by circulatory features, such as high pressure in the right ventricle, low volume of blood flow in the pulmonary artery, parallelism of the ventricles of the heart, functioning ductus arteriosus and oval window, pumping blood as bypass anastomoses into the systemic circulation due to hard work right ventricle. These features of intracardiac hemodynamics of the fetus should certainly correct the nature of hemodynamic changes ultrasonic indicators hearts are normal and with heart defects in the fetus.
It is known that in patients with congenital heart defects, hemodynamic disturbances result from anatomical changes V to a large extent influence the data ultrasound scanning heart, such as the size of the heart cavities, the degree of myocardial hypertrophy, the function of the valve apparatus, contractility myocardium, direction of movement of the interventricular septum.
The method for assessing intracardiac hemodynamics is based on the well-known concepts of systolic, volumetric and mixed cardiac overload, proposed in 1952 by E. Cabrera and J. Monroy.
The division is based on the following principle.
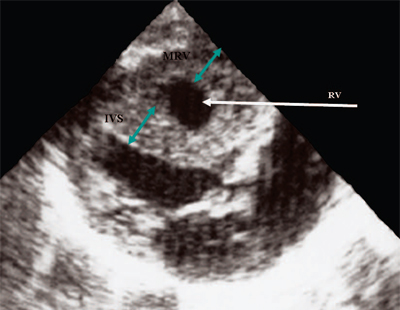
Resistance load occurs in a situation where the ejection of blood from the ventricles of the heart into the great vessels is hindered at the level of the semilunar valves (stenosis of the aorta and pulmonary artery), subvalvular space (idiopathic hypertrophic subaortic stenosis, subvalvular stenosis of the aorta or pulmonary artery), along the vascular bed (coarctation aorta) or with a significant increase in output resistance (Eisenmenger syndrome). As a result of the difficulty in ejecting blood, the tension in the myocardium of the corresponding ventricle sharply increases with a relatively stable blood volume, which serves as a manifestation of systolic overload of the heart. With systolic overload of the ventricles of the heart, regardless of the nosological form of the defect, the cavity of the ventricle, which bears the main resistance load, moderately increases in size. In response to resistance load, the echocardiogram reveals hypertrophy of the myocardium of the corresponding ventricle, and the greater the resistance to ejection, the more pronounced the degree of hypertrophy of the myocardium of the corresponding ventricle and the interventricular septum (Fig. 1).
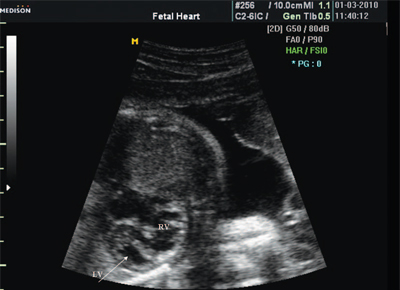
Rice. 1. Systolic overload of the right ventricle. Cross-section of the ventricles of the heart in pulmonary stenosis. The pressure gradient from the right ventricle to the pulmonary artery is 200 mm Hg. Severe hypertrophy of the interventricular septum and myocardium of the anterior wall of the right ventricle.
IVS - interventricular septum, MRV - right ventricular myocardium, RV - right ventricle.
Volume load occurs with additional blood flow into the ventricles and as a result of shunting of blood through the septal septa or ductus arteriosus (atrial and ventricular septal defects, patent ductus arteriosus), as well as as a result of reverse blood flow through the atrioventricular valves (valvular insufficiency).
Characteristic features of severe volume overload of the right ventricle are ventricular dilatation, in which the myocardial thickness does not exceed upper limit norms, enlargement of the right atrium, paradoxical nature of the movement of the interventricular septum and an increase in the amplitude of movement of the tricuspid valve (Fig. 2, 3).

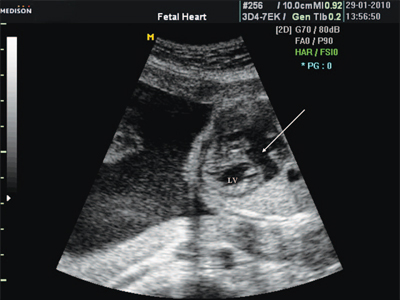
Rice. 2. Long axis of the heart. Volume overload of the right ventricle with atrial septal defect. The volume of blood discharge exceeds 200% of the MVR. There is marked dilatation of the right ventricle.
RV - right ventricle, AO - aorta, LA - left atrium, MV - mitral valve.

Rice. 3. Volume overload of the right ventricle with atrial septal defect. B- and M-scanning. The arrow shows the paradoxical nature of the movement of the interventricular septum.
For the left ventricle, a sign of volume overload is an increase in the cavity of the left atrium and ventricle, as well as excursions of the interventricular septum and myocardium back wall left ventricle (Fig. 4).
IVS - interventricular septum, MLV - myocardium of the left ventricle, LV and RV - left and right ventricles.
When a resistance and volume load is combined, a mixed overload occurs (for example, with a ventricular septal defect and an increase in pressure in the pulmonary artery for the right ventricle, systolic overload is combined with a volume load, for the left ventricle as a result of arteriovenous discharge of blood through the defect).
Over a long-term period (from 1980 to the present) of observations at the Federal State Institution Science Center obstetrics and perinatology named after. V.I. Kulakov Ministry of Health and Social Development of Russia, it was noted that in the antenatal period the principles of hemodynamic echocardiographic manifestations of congenital heart disease, which were previously developed and presented in modern literature, do not always work.
An analysis of more than 2000 observations of congenital heart defects in the fetus showed that in a number of observations there are only anatomical changes characteristic of a certain nosological form of the defect. With other congenital heart defects, changes in the echocardiogram are associated with the nature of the hemodynamic load on the heart and are similar to what is observed after birth. Finally, in a number of observations of congenital heart defects in the fetus secondary changes on an echocardiogram caused by hemodynamic disturbances differ from the hemodynamic manifestations of ultrasound indicators in children and adults. This made it possible to divide all congenital heart defects of the fetus into three groups depending on changes in the echocardiogram due to the characteristics of antenatal intracardiac hemodynamics.
The first group included heart defects that, while having clear anatomical manifestations of pathology, do not have hemodynamic manifestations of congenital heart disease during ultrasound examination. These include: atrial septal defect, ventricular septal defect, common ventricle, simple form of transposition great vessels and also in the presence of a ventricular septal defect, a common arterial trunk, double origin of vessels from the ventricles of the heart.
This should be analyzed using the example of atrial septal defect. The basis for intracardiac hemodynamic disorders in atrial septal defect is volume overload of the right heart. In ultrasound examinations in children and adults, this leads to:
- dilatation of the right ventricle (see Fig. 2, 3);
- enlargement of the right atrium;
- the paradoxical nature of the movement of the interventricular septum (see Fig. 2, 3).
Antenatally, with equal pressure values in the ventricles of the heart and in the atria, volume overload does not occur. In this regard, none of the echocardiographic hemodynamic signs used in children and adults are detected in the fetus. The echocardiographic manifestations of a defect antenatally include only a direct sign - a break in the ultrasound beam in the area of the defect. The size of the heart and the ratio of the sizes of the ventricles of the heart do not differ from the norm (Fig. 5).
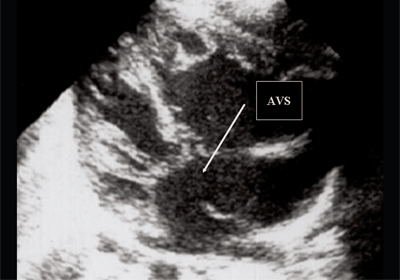
Rice. 5. Four-chamber section of the fetal heart. The arrow indicates the primary atrial septal defect (AVS).
This equally applies to the ventricular septal defect (Fig. 6), a simple form of transposition of the great vessels (Fig. 7, 8), transposition of the great vessels with a ventricular septal defect (Taussig-Bing syndrome) (Fig. 9), common ventricle ( Fig. 10), general truncus arteriosus(Fig. 10), double origin of vessels from one of the ventricles of the heart (Fig. 11).
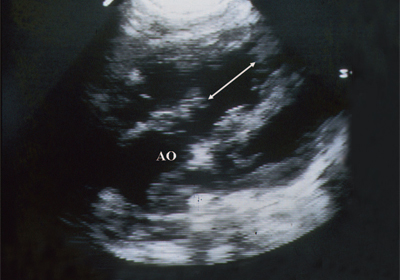
Rice. 6. Ventricular septal defect. Long axis of the heart. Arrows indicate a ventricular septal defect.
AO - aorta.
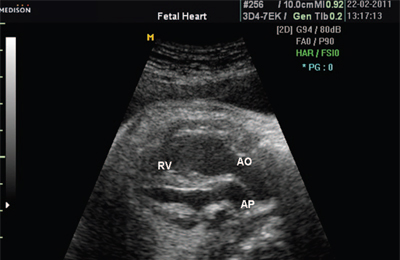
Rice. 7. Transposition of the great vessels.
AR - pulmonary artery, AO - aorta, RV - right ventricle.

Rice. 8. Transposition of the great vessels, arrows indicate the branches of the pulmonary artery.
AR - pulmonary artery, LV - left ventricle.
Rice. 9. Taussig-Bing syndrome. The pulmonary artery (marked with an arrow) is located above the ventricular septal defect.
AR - pulmonary artery, LV and RV - left and right ventricles.
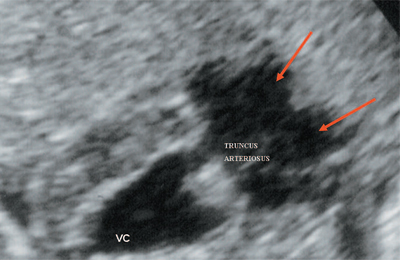
Rice. 10. Common ventricle with origin TRUNCUS ARTERIOSUS. The arrows show the division of TRUNCUS ARTERIOSUS into the aorta and the trunk of the pulmonary artery.
VC - common ventricle, TRUNCUS ARTERIOSUS - common arterial trunk.

Rice. 11. Double origin of the great vessels from the left ventricle. Long axis of the heart. The great vessels are inverted and arise from the left ventricle. The aorta is located “on top” of the ventricular septal defect (arrow).
LV and RV - left and right ventricle, AR - pulmonary artery, AO - aorta, VSD - ventricular septal defect.
Thus, the diagnosis of the above congenital heart defects is based on knowledge of the anatomical changes characteristic of a certain nosological form of the pathology.
The second group of congenital heart defects. Ultrasound examination records anatomical and hemodynamic changes characteristic of a certain nosological form of the defect. This group included: aortic stenosis, pulmonary artery stenosis, congenital mitral stenosis, transposition of the great vessels with narrowing of the pulmonary artery, obstruction of the outflow tract of one of the ventricles by a tumor, Ebstein's anomaly, hypoplastic syndrome of the right and left ventricles of the heart, fibroelastosis, premature closure of the oval window.
As an example, we can look at changes in echocardiographic parameters in valvular pulmonary artery stenosis. Hemodynamic disturbances in isolated pulmonary artery stenosis are caused by an obstruction in the path of blood ejection into the pulmonary artery. The severity of stenosis is determined by the difference systolic pressure in the right ventricle and pulmonary artery, i.e. pressure gradient.
Two-dimensional examination reveals thickening of the pulmonary valve leaflets, their excursion is reduced, and in systole they form a dome. These are anatomical manifestations of the defect. To these are added hemodynamic manifestations: pronounced hypertrophy of the myocardium of the anterior wall of the right ventricle and the interventricular septum, significantly exceeding the standards. The severity of right ventricular myocardial hypertrophy depends on the degree of pulmonary artery stenosis and, accordingly, on the magnitude of the pressure gradient. These data were obtained by comparing the results of ultrasound scanning and catheterization data of the heart cavities in children. It should be especially noted that with severe myocardial hypertrophy, the cavity of the right ventricle increases slightly. There is also an increase in the size of the right atrium.
In the fetus, similar changes were obtained, also depending on the degree of stenosis of the pulmonary artery. The cavity of the right ventricle, as seen in Fig. 12, not enlarged. At the same time, there is significant hypertrophy of the walls of the right ventricle. As in postnatal period an increase in the cavity of the right atrium was noted (Fig. 13). After birth, catheterization of the cardiac cavities in this observation revealed a pressure gradient at the outlet of the right ventricle equal to 200 mm Hg.
Rice. 12. Pulmonary artery stenosis. Hypertrophy of the right ventricular myocardium.
RV - right ventricle, IVS - interventricular septum, MRV - right ventricular myocardium.
Rice. 13. Severe pulmonary artery stenosis. Four-chamber cross-section of the heart. Significant enlargement of the right atrium cavity.
Such a relationship with disturbances of intracardiac hemodynamics in the fetus, of course, can be detected only in the case of a pronounced disturbance of the outflow of blood from the right ventricle into the pulmonary artery, since pulmonary blood flow in the antenatal period ranges from 12 to 20%. The remaining blood volume flows through the ductus arteriosus into the descending aorta. Therefore, slight stenosis of the pulmonary artery is not so informative in terms of hemodynamic ultrasound manifestations.
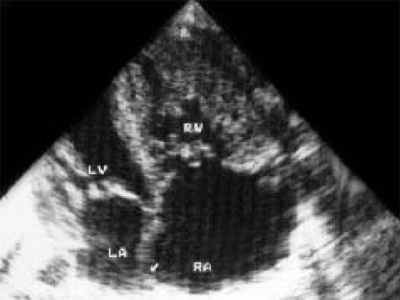
With Ebstein's anomaly, antenatal diagnosis, as in the postnatal period, is based on determining the location of the tricuspid valve in relation to the mitral valve and its displacement deep into the right ventricle. When researching, pay attention large sizes heart, mainly due to the right atrium (Fig. 14). Dopplercardiographic examination reveals tricuspid insufficiency.

Rice. 14. Ebstein's anomaly. Four-chamber cross-section of the heart. There is a displacement of the tricuspid valve towards the apex of the right ventricle.
LV and RV - left and right ventricle, RA - right atrium, TV - tricuspid valve, MV - mitral valve.
Minor aortic stenosis does not cause hemodynamic disturbances in the fetus. If there is a significant obstruction to the ejection of blood from the left ventricle, the pressure in it increases and the work of the left ventricle increases. With severe stenosis, the resistance to blood ejection increases significantly, the pressure in the left atrium also increases, and a left-to-right shunt of blood appears through the oval window, in contrast to the normal right-to-left shunt for the fetus. This causes symptoms of heart failure and may cause intrauterine retention development
Ultrasound examination reveals pronounced hypertrophy of the left ventricular myocardium (Fig. 15). The size of the left atrium increases. Mitral regurgitation may be recorded.
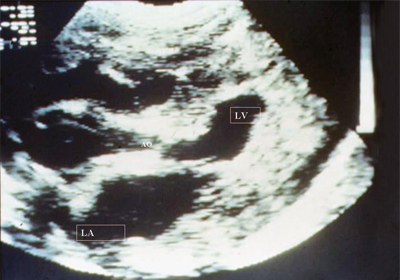
Rice. 15. Aortic stenosis. Long axis of the heart. There is a pronounced narrowing of the aortic opening, pronounced hypertrophy of the left ventricular myocardium, a decrease in its cavity and dilatation of the left atrium.
LV - left ventricle, LA - left atrium, AO - aorta.
With hypoplasia of the left side syndrome, circulatory disorders occur at early stages fetal development. Unlike normal fetal circulation, when blood from the vena cava partially passes through the oval window into the left chambers of the heart and into the systemic circulation, all the blood enters the right ventricle and pulmonary trunk. There is also a discharge of blood from the left atrium to the right through the oval window. Therefore, volume overload and dilatation of the right ventricle are observed antenatally (Fig. 16). The peculiarities of intracardiac hemodynamics also explain the fact that color flow mapping reveals retrograde or bidirectional blood flow through the foramen ovale and retrograde blood flow in the distal aorta.
Rice. 16. Left ventricular hypoplasia. The ratio of the sizes of the heart cavities is changed due to a compensatory increase in the size of the right ventricle.
LV and RV - left and right ventricle.
Premature closure of the oval window. With antenatal closure of the foramen ovale, right ventricular heart failure develops and the child is usually born dead. The left sections become hypoplastic, the myocardium of the left ventricle significantly hypertrophies (Fig. 17).

Rice. 17. Premature closure of the oval window valve. Moderate hypoplasia of the left ventricle and a significant enlargement of the left atrium are noted; the arrow indicates the mitral orifice.
LV - left ventricle, LA - left atrium, MV - mitral valve.
Finally, the third group of congenital heart defects, which differs in hemodynamic changes in the echocardiogram of the antenatal period from changes in the data ultrasound examination in the postnatal period. This group is small and will be discussed in detail. It included the following congenital heart defects: atrioventricular septal defect, tetralogy of Fallot, Steidel syndrome, coarctation of the aorta.
Atrioventricular septal defect. At full form of an atrioventricular septal defect, all four chambers communicate with each other. Hemodynamic disturbances are determined by the presence of messages at the atrial and ventricular levels and inadequate function of the atrioventricular valves. The load on all chambers of the heart is significantly increased.
Ultrasound diagnostics atrioventricular septal defect is based on the anatomical components of the defect (detection of a primary atrial septal defect; the presence of a high ventricular septal defect; in the complete form, the presence of a gap between the mitral and tricuspid valves). There are signs of an abnormality mitral valve, which are manifested by the approach of the anterior leaflet to the interventricular septum. This sign By analogy with angiography, it is called the “goose neck” symptom.
In addition to the anatomical components of the pathology, there are changes associated with hemodynamic changes:
- enlargement of the right atrium;
- reduction in the size of the left ventricle, associated with the presence of arteriovenous blood discharge, as well as often observed with atrioventricular septal defect moderate hypoplasia left ventricle.
What happens antenatally? Blood from the superior and inferior vena cava from the right atrium enters the left atrium through the oval window. Therefore, the enlargement of the right atrium, which manifests itself after birth, is not observed in the fetus. There is an enlargement of the left atrium cavity. This is the first difference in hemodynamic ultrasound signs in the atrioventricular canal in the fetus (Fig. 18).
Rice. 18. Atrioventricular septal defect (arrow).
LV - left ventricle.
The second difference in hemodynamic manifestations is increased or normal sizes left ventricle, in contrast to the reduced size observed after birth.
Tetralogy of Fallot. Hemodynamic changes in tetralogy of Fallot are determined by the degree of obstruction to the ejection of blood from the right ventricle into the pulmonary circulation and the presence of a ventricular septal defect. The amount of blood shunt is determined by the degree of obstruction to the ejection of blood from the right ventricle into the pulmonary artery and the resistance great circle blood circulation
Anatomical signs of pathology include dextroposition of the aorta and ventricular septal defect. Distinctive feature This pathology is considered to be an increase in the diameter of the aorta and infundibular narrowing of the pulmonary artery. A hemodynamic manifestation of the pathology should be considered hypertrophy of the right ventricular myocardium with a slight expansion of its cavity.
The fetus also clearly visualizes characteristic anatomical changes: a wide aorta located as a “rider aorta”, a ventricular septal defect. Unlike children and adults, infundibular pulmonary artery stenosis is not detected antenatally. The absence of subvalvular narrowing in the early neonatal period is also noted by pathologists. This corresponds to the opinion that this component of the pathology manifests itself in more mature age and increases with the patient's age.
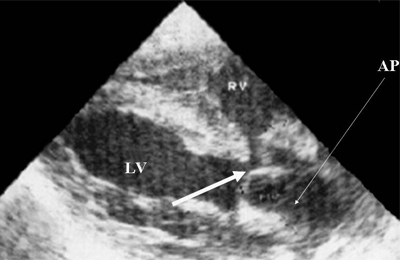
Antenatally, the right ventricle, due to the presence of pulmonary artery stenosis and ventricular septal defect, is less involved in the work of the heart than is normally observed, when the main load falls on the right parts of the heart. Therefore, the size of the right ventricle is reduced compared to the gestational age norm. At the same time, blood circulation is carried out due to increased load to the left ventricle. The latter, as a result of intense work, hypertrophies starting from the 22nd week of gestation. Thus, tetralogy of Fallot is characterized antenatally by left ventricular myocardial hypertrophy (Fig. 19).
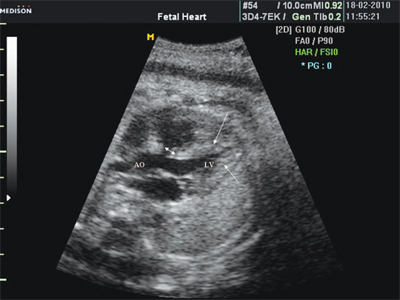
Rice. 19. Tetralogy of Fallot. The double arrow indicates a ventricular septal defect. Arrows indicate left ventricular myocardial hypertrophy.
LV - left ventricle, AO - aorta.
Coarctation of the aorta. The main diagnostic sign of aortic coarctation is visualization of the arch and descending aorta with the presence of its anatomical narrowing. Antenatally, this anatomical sign of pathology is observed only in 30% of cases, since coarctation often forms after birth and closure of the ductus arteriosus.
Hemodynamic signs of the defect in children and adults include:
- left ventricular myocardial hypertrophy;
- enlargement of the left atrium.
Antenatally, in the presence of coarctation of the aorta, the right ventricle, which is actively involved in the blood supply to the fetal organs, works against resistance to flow through the ductus arteriosus into the descending aorta. As a result, an increase in the cavity of the right ventricle and its hypertrophy are noted. (Fig. 20). The trunk of the pulmonary artery is also dilated. These ultrasound signs of pathology are present in 70% of cases.

Rice. 20. Coarctation of the aorta (a, b). Severe narrowing of the aorta typical place in three-dimensional image (b). When examining the long axis of the heart, pronounced hypertrophy of the right ventricular myocardium is noted.
MRV - right ventricular myocardium, IVS - interventricular septum.
An assessment of pathology using the index of the ratio of the size of the right ventricle to the size of the left ventricle and the ratio of the pulmonary artery diameter to the aortic diameter has been proposed. Normally, these indicators are 1.1 and 1.2, respectively.
With pronounced narrowing of the aorta (narrowing up to 25% of the normal value), signs of heart failure in the fetus are observed early, manifested by the presence of pericardial effusion, a significant decrease in the size of the left ventricle and a decrease in cardiac output.
Hypoplasia of the left ventricle with damage to the arches and aorta. Diagnosis of pathology antenatally, according to many authors, is not difficult; all signs that are important for diagnosis in newborns and adults should be used in antenatal examination.
To the classics ultrasonic signs left ventricular hypoplasia syndrome include:
- sharp narrowing of the ascending aortic arch;
- decrease in end-diastolic size of the left ventricle;
- narrowing of the aortic diameter;
- increase in end-diastolic size of the right ventricle;
- the ratio of the end-diastolic size of the left ventricle to the end-diastolic size of the right ventricle, equal to or less than 0.6;
- the presence of gross changes in the mitral valve.
The diagnostic task can be facilitated in the presence of ascites, hydropericardium in the fetus, or with concomitant extracardiac pathology.
Identifying all anatomical changes in left ventricular hypoplasia syndrome does not present significant difficulties. However, available observations have shown that in some cases the cavity of the left ventricle decreases slightly, while there is pronounced hypertrophy of the left ventricular myocardium. Comparison with data after birth, as well as with autopsy data, showed that such characteristic changes in left ventricular hypoplasia syndrome are observed in the most severe anatomical shape pathology - Steidel syndrome (atresia aortic valve in combination with hypoplasia ascending department aorta). The index of the ratio of the size of the left ventricle to the size of the right ventricle in diastole is within 0.6. With hypoplasia of the left ventricle without damage to the aortic arch, it does not exceed 0.15-0.2. With Steidel syndrome, if there is a small size of the left ventricle, pronounced hypertrophy of the left ventricular myocardium up to 0.7 cm is observed antenatally (Fig. 21), with left ventricular hypoplasia syndrome without damage to the aortic arch, the thickness of the myocardium does not exceed 2-3 mm.
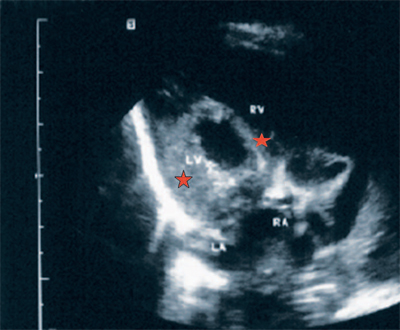
Rice. 21. Steidel's syndrome. Four-chamber cross-section of the heart. The cavity of the left ventricle is reduced. There is pronounced hypertrophy of the left ventricular myocardium and interventricular septum. The cavities of the right ventricle and right atrium are significantly increased in size.
LV and RV - left and right ventricle, LA and RA - left and right atrium.
Thus, during long-term observation of heart defects in the fetus, characteristic features hemodynamic manifestations of various nosological forms of pathology. All this with a clear manifestation of the anatomical components of heart defects can help in their antenatal diagnosis.
Literature
- Mac Mahon B., Mc Keown T., Record R.G. The incidence and life expectancy of children with congenital heart disease // Br. Heart J. 1953. V. 15. P. 121-129
- Cabrera E., Monroy J. Systilic and Diastolic lag- ing of the heart // Am. Heart J.1952. V. 43. N 5. P. 661.
- Zatikyan E.P. Features of intracardiac hemodynamics in patients with congenital heart defects during pregnancy. Diss. ... doc. honey. Sci. M., 1988.
- Burakovsky V.I., Bockeria L.A. Cardiovascular surgery. M.: Medicine, 1989.
- Zatikyan E.P. Hemodynamic patterns of echocardiogram changes in congenital heart defects // Cardiology. 1990. N 8. P. 47-50.
- Zatikyan E.P. Congenital and acquired heart defects in pregnant women. Functional and ultrasound diagnostics. M.: Triada-X, 2004.
- Allan L.D., Cook A.C., Huggon C. Fetal Echocardiography / Cambridge University Press, 2009.
- Kleinmann C.S., Donnerstein R.L., De Vore G.R. et al. Fetal echocardiography for evalution of in utero congestive heart failure: A technique for study of nonimmune fetal hydrops // N. Engl. J. Med. 1982. V. 306. P. 568.
- Sahn D.J. Sh ndrome in utero associated with hydrops fetalis // Am. Heart J. 1982. V.104, N 6. P. 1368-1372.
- Norberger L.K., Sanders S.P., Rein A.J. et al. Left heart obstructive lesions and left ventricular growth in the midtrimester fetus. A longitudinal study // Circulation. 1995. V. 92. N 6. P. 1531-1538.
- Medvedev M.V. Prenatal echography. Differential diagnosis and forecast. M.: Real Time, 2009
- Nanda N., Gramiak R. Clinical Echocardiography. S. Louis, 1975.
- Zatikyan E.P. Atrioventricular septum defect in the prenatal period // International Society The Fetus as a patient IX th International congress 1993. P. 41. Tokyo.
- Zatikyan E.P. Atrioventricular septal defect in prenatal period// Ultrasound diagnostics in obstetrics, gynecology and pediatrics. 1993. N 3. P. 40-45.
- Ohba T., Matsui K., Nakamura K. et al. Tetralogy of Fallot with absent pulmonary valve detected by fetal echocardiography // Int. Gynaecol. Obstet. 1990. V. 32. N 1. P. 71-74.
- Zatikyan E.P. Fetal cardiology. M.: Triada-X, 2009.
- Allan L.D., Chita S.K., Anderson R.H. et al. Coarctation of the aorta in prenatal life: and echocardiographic, anatomical and functional study // Br. Heart J. 1988. V. 59. P. 356.
- Zatikyan E.P. Echocardiographic assessment of the severity of anatomical and hemodynamic changes in hypoplastic left heart syndrome: dynamic observation from fetus to newborn // Ultrasound diagnostics. 2000. N 3. P. 29-36.
– a group of diseases united by the presence of anatomical defects of the heart, its valve apparatus or blood vessels that arose during prenatal period, leading to changes in intracardiac and systemic hemodynamics. Manifestations of congenital heart disease depend on its type; to the most characteristic symptoms include pallor or cyanosis of the skin, heart murmurs, lag in physical development, signs of respiratory and heart failure. If a congenital heart defect is suspected, an ECG, PCG, radiography, echocardiography, cardiac catheterization and aortography, cardiography, cardiac MRI, etc. are performed. Most often, for congenital heart defects, cardiac surgery is used - surgical correction of the identified anomaly.
Complications of congenital heart defects can include bacterial endocarditis, polycythemia, thrombosis peripheral vessels and thromboembolism of cerebral vessels, congestive pneumonia, syncope, dyspnea-cyanotic attacks, angina pectoris syndrome or myocardial infarction.
Diagnosis of congenital heart defects
Detection of congenital heart defects is carried out by comprehensive examination. When examining a child, the color of the skin is noted: the presence or absence of cyanosis, its nature (peripheral, generalized). Auscultation of the heart often reveals changes (weakening, strengthening or splitting) in heart sounds, the presence of murmurs, etc. Physical examination if a congenital heart defect is suspected is supplemented instrumental diagnostics- electrocardiography (ECG), phonocardiography (PCG), chest radiography, echocardiography (EchoCG).
ECG reveals hypertrophy various departments hearts, pathological deviation EOS, the presence of arrhythmias and conduction disorders, which in combination with data from other methods clinical examination allows us to judge the severity of congenital heart disease. With the help of 24-hour Holter ECG monitoring, hidden rhythm and conduction disturbances are detected. Through PCG, the nature, duration and localization of heart sounds and murmurs are assessed more carefully and in detail. Chest X-ray data complement previous methods by assessing the state of the pulmonary circulation, the location, shape and size of the heart, changes in other organs (lungs, pleura, spine). At conducting echocardiography anatomical defects of the septa and valves of the heart, the location of the great vessels are visualized, and the contractility of the myocardium is assessed.
In case of complex congenital heart defects, as well as concomitant pulmonary hypertension, for the purpose of accurate anatomical and hemodynamic diagnosis, there is a need to perform sounding of the cardiac cavities and angiocardiography.
Treatment of congenital heart defects
Most complex problem in pediatric cardiology is the surgical treatment of congenital heart defects in children of the first year of life. Most operations in early childhood are performed for cyanotic congenital heart defects. If the newborn has no signs of heart failure or moderate cyanosis, surgery may be postponed. Children with congenital heart defects are monitored by a cardiologist and a cardiac surgeon.
Specific treatment in each specific case depends on the type and severity of congenital heart disease. Operations for birth defects heart septum (VSD, ASD) may include plastic surgery or suturing of the septum, X-ray endovascular occlusion of the defect. In the presence of severe hypoxemia, for children with congenital heart defects, the first stage is palliative intervention, which involves applying various kinds intersystem anastomoses. This tactic improves blood oxygenation, reduces the risk of complications, and allows for radical correction in more favorable conditions. In case of aortic defects, resection or balloon dilatation of coarctation of the aorta, plastic surgery of aortic stenosis, etc. is performed. In case of PDA, its ligation is performed. Treatment of pulmonary artery stenosis consists of open or endovascular valvuloplasty, etc.
Anatomically complex congenital heart defects, in which radical surgery is not possible, they require hemodynamic correction, i.e., separation of arterial and venous blood flows without eliminating the anatomical defect. In these cases, Fontan, Senning, Mustard, etc. operations can be performed. Serious defects that cannot be treated surgical treatment require a heart transplant.
Conservative treatment of congenital heart defects may include symptomatic therapy dyspnea-cyanotic attacks, acute left ventricular failure (cardiac asthma, pulmonary edema), chronic heart failure, myocardial ischemia, arrhythmias.
Prognosis and prevention of congenital heart defects
In the structure of newborn mortality, congenital heart defects occupy first place. Without qualified cardiac surgical care, 50-75% of children die during the first year of life. During the compensation period (2-3 years), mortality decreases to 5%. Early detection and correction of congenital heart disease can significantly improve the prognosis.
Prevention of congenital heart defects requires careful planning of pregnancy, eliminating the impact of adverse factors on the fetus, conducting medical and genetic counseling and educational work among women at risk for having children with cardiac pathology, resolving the issue of prenatal diagnosis of the defect (ultrasound, chorionic villus biopsy, amniocentesis) and indications for termination of pregnancy. Management of pregnancy in women with congenital heart defects requires increased attention by an obstetrician-gynecologist and cardiologist.
Echocardiography (ultrasound of the heart) is a method of examining an organ, showing existing deterioration and abnormalities. Ultrasound is an absolutely harmless and simple procedure that can be used to detect diseases such as pulmonary hypertension, congenital defects in children, mitral valve defects, prolapse and other disorders.
The structure of the heart can be divided into four sections (chambers): the left and right atrium and the left and right ventricle. The interatrial septum separates both atria, the interventricular septum separates the ventricles. The purpose of these partitions is to prevent blood types from mixing. The tricuspid valve connects the right atrium and the right ventricle. They move blood from the veins to the lungs. The left atrium and left ventricle are connected by the mitral valve. With their help arterial blood spreads throughout the body, and they prevent blood from returning back to the heart.
The human heart is divided into four chambers: the left and right atrium and the left and right ventricle, separated from each other. This separation is necessary so that venous and arterial blood do not mix with each other
Why is the examination carried out?
Echocardiography (ultrasound of the heart) is considered a simple diagnostic procedure that helps detect certain diseases before their manifestations occur. Typically, echocardiography is prescribed for those suffering from shortness of breath, dizziness, lethargy, fainting, the occurrence of tachycardia attacks, disorders that interfere with cardiac activity, and pain in the organ.
If a heart murmur is detected, there are suspicions of diseases harmful to the cardiovascular system (for example, rheumatism) and lung diseases in chronic form, present hypertension, and electrocardiography indicates disturbances in cardiac activity, then an appointment for examination is mandatory. Also prescribed to children to confirm heart defects at birth.

Most the latest devices Ultrasound not only performs an ultrasound examination of the cardiovascular system, but can also do Doppler sonography, which involves tracing the movement of blood in the chambers of the heart. Helps to observe the functioning of the organ and identify deficiencies in the development of valves.
Norms of cardiac echocardiography
Echocardiography can reveal a number of abnormalities in the activity of the heart muscle. Only a specialist can conduct an analysis and make a conclusion. The following parameters are normal when performing echocardiography:
- aortic diameter - up to 3.7 cm;
- opening of the aortic valve leaflets - 1.5 cm or more;
- left atrium size - up to 4 cm;
- end diastolic size of the left ventricle - up to 5.5 cm;
- end systolic size of the left ventricle - up to 4.1 cm;
- thickness of the interventricular septum - up to 1.1 cm;
- thickness of the posterior wall of the left ventricle - up to 1.1 cm;
- ejection fraction - not less than 60%;
- shortening fraction - 30-40%;
- mitral valve opening area - 4 cm2;
- the size of the cavity of the right ventricle is up to 3 cm.
When performing echocardiography, the doctor studies the size of the chambers, wall thickness, contours and activity of the valves, and the activity of the myocardium (muscle layer). Deterioration of certain indicators indicates various violations cardiovascular system.
 Using an ultrasound of the heart (echocardiography), the doctor can see the structure of the organ, the thickness and functionality of the chamber walls, and track the location and size of the valves. All these data are highly informative when making a diagnosis.
Using an ultrasound of the heart (echocardiography), the doctor can see the structure of the organ, the thickness and functionality of the chamber walls, and track the location and size of the valves. All these data are highly informative when making a diagnosis. Pulmonary hypertension on ultrasound
Pulmonary hypertension– increasing increase in pressure in the pulmonary artery. There is a distinction between congenital and acquired hypertension. Echocardiography provides the maximum amount of information to determine arterial pressure to make a diagnosis of pulmonary hypertension. Indicators detected in the M-mode, such as inhibition of arterial valve opening, its closure during systole, and an increase in the duration of right ventricular ejection in relation to the total duration of ejection, indicate pulmonary hypertension.
Two-dimensional ultrasound may show right ventricular hypertrophy. If its wall is more than 10 mm, then the conclusion follows about excessive hypertrophy, which is observed in chronic pulmonary heart. The concept of normal (absence of hypertension) includes a value of less than 4 mm, while acute pulmonary hypertension gives 6-8 mm. wall thickness. 2D study in hypertension it also reveals flexibility of the interventricular septum. Pulmonary hypertension in severe form causes paradoxical systolic movement, which, combined with reduced pulmonary flow, leads to a deterioration in isometric relaxation of the left ventricle.
Additional symptoms of hypertension:
- discharge of blood from right to left along the open ductus arteriosus;
- discharge of blood from right to left along the oval window;
- pulmonary artery with a pressure greater than 40 mm. rt. Art., more than 50% of the total pressure.
Congenital heart defects studied in children
Congenital heart defects are disorders in the anatomy of an organ that are an intrauterine pathology. Often this pathology is caused by negative influences on the embryo in the womb. There are several varieties of this disease.
 Heart disease is an anomaly that develops in utero. Most often it is associated with a genetic predisposition or negative external influence for the fruit
Heart disease is an anomaly that develops in utero. Most often it is associated with a genetic predisposition or negative external influence for the fruit Patent ductus arteriosus- a channel that establishes a connection between the pulmonary artery and the aorta. During intrauterine development, it actively provides the fetus with oxygen without using the lungs for this purpose. Overgrows 2-8 weeks after birth. If this does not happen, it is considered a defect. Congenital pathology children may not have any symptoms, but sometimes the disease is detected in the form of stunted growth, darkening of the skin, and frequent pneumonia. When examining an ultrasound, you can notice an increase in the wall of the atrium and ventricle of the heart affected by the defect, and Dopplerography will show whether there is a discharge of blood from the aorta into the pulmonary artery, which is also an indicator of pathology.
Ventricular septal defect– pathology when the membrane has a congenital gap between the right and left ventricles. From the left ventricle with high pressure the blood moves to the right, where the pressure is low. The congenital defect is characterized by the following symptoms: developmental delays, frequent pneumonia. Upon examination, one can note a congenital enlargement of the cardiac cavity and an increase in the thickness of the walls. Dopplerography determines the discharge of blood from the left ventricle to the right.
Atrial septal defect– the wall located between the atria has a gap. Ultrasound diagnostics allows one to see thickened atria, and sometimes the congenital hole itself is visible.
Mitral valve defects in diagnosis
Mitral valve stenosis- a defect with a decrease in the gap located between the left atrium and the left ventricle. Manifestations of pathology: dizziness, difficulty breathing, rapid heartbeat, painful sensations in the chest. The disease causes thickening of the valve leaflets, the walls of the left atrium and the right ventricle.
Mitral valve prolapse- a defect with stretching of the gap in the space of the left atrium and left ventricle, as well as prolapse - this is a weak compression of the mitral valve leaflets at the time of systole. Mitral valve prolapse is congenital and differs in stages 1 and 2 of prolapse. Often, such prolapse is not considered a disease and does not require treatment. Endocarditis and rheumatism can cause prolapse. However, prolapse does not manifest itself for a long time. Signs of mitral prolapse: shortness of breath, lethargy, painful sensations from physical labor.
Echocardiography in a patient with mitral valve prolapse reveals an increase in the volume of the walls of the left ventricle and atrium, partial compression of the mitral valve leaflets in systole. The use of Doppler ultrasound allows you to determine the stage of prolapse.
Other heart diseases on ultrasound
Myocardial infarction– a disorder of blood supply, which leads to the extinction of the activity of one of its parts. Ultrasound of the patient's heart, suffered a heart attack myocardium, detects deterioration in compression of one of the organ sections.
Exudative pericarditis– accumulation of moisture in the pericardium (the lining of the organ). Pericarditis is manifested on ultrasound by the detection of moisture accumulated in the heart sac.
Myocarditis– types of diseases characterized by inflammatory process myocardium. Signs of abnormalities on echocardiography: enlargement of the organ chambers, decreased contractile function, decreased left ventricular ejection (less than 50%).
Infective endocarditis– penetration of infection causes inflammation of the endocardium. Tears and branches on valves - signs infective endocarditis in ultrasound diagnostics.

