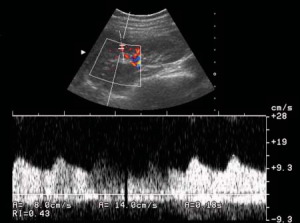
Peak systolic blood flow velocity is normal. Ultrasound examination of blood vessels. Vascular examination of the upper extremities
Physical Basics ultrasound and options ultrasonic methods Research in cardiology is described in detail in numerous manuals, to which we refer the inquisitive reader.
Currently in Angiology greatest distribution received following methods Ultrasound:
- Doppler ultrasound, which allows you to measure the speed of blood flow;
- Ultrasound angiography (B-scan), which provides visualization of the internal lumen of the vessel, measurement of its diameter and assessment of the condition vascular wall;
- duplex scanning, combining both of the above methods;
- spectral analysis and color mapping of the Doppler signal, allowing one to study the nature and speed of blood flow in the heart and blood vessels.
Rice. 3.21. Age-related changes dopple transonic beam. A sarogram of the peripheral artery should be performed.
It should be noted that Doppler ultrasound (D-ultrasound) of blood vessels is not a method of direct visualization of atherosclerotic lesions of the arteries, but by changes in blood flow speed it allows one to judge the severity vascular pathology.
IN modern diagnostics For diseases of the heart and blood vessels, four options for D-ultrasound are used. 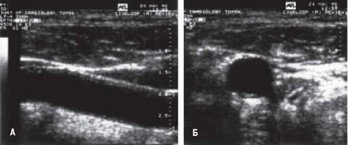
Doppler examination for fetal anemia
Because there is variation in results between laboratories, each institution must determine its "critical titer" - the level at which there is a significant risk of developing hydrographs. Intra-articular transfusions continue until 35 weeks of pregnancy. Ideally, embryonic intervention should occur before hydrogel onset. As a result, noninvasive methods that predict severe anemia before the onset of hydrogels have been requested. Over the years, several vessels have been evaluated to better predict severe anemia.
growth and blood flow patterns.
Spectral analysis of Doppler signals showed differences in arterial blood flow depending on age, even in healthy people (Fig. 3.21).
It is known that when studying the speed of blood flow through vessels using ultrasound, the Doppler effect is manifested better, the higher the elasticity of the vessel wall, effective pressure and resistance. This is expressed as a velocity profile (Fig. 3.21) with a steep acceleration rise (a). The decrease in movement speed (b) is less rapid with incisura (c), dicrotic tooth (d), post-systolic reflux (e). The elastic resistance of the artery causes the appearance of a positive wave (f). Thus, sufficient elasticity of the arterial walls allows the left ventricle to eject blood into the arterial bed, even if the arterial capillary resistance is increased. The ability of arteries to contract elastically ensures the maintenance of blood flow during diastole. Due to atherosclerosis, the elasticity of the arterial wall decreases, which leads first of all to a decrease in the secondary positive wave (f), then there is a reduction in reflux (e), rounding of the apex and expansion of the base of the main Doppler complex.
In accordance with known physical laws, the vessel wall has greater acoustic resistance compared to surrounding tissues; therefore, it gives a brighter reflection of the ultrasound signal than nearby tissues. soft fabrics. The lumen of the vessel has less  neck acoustic resistance than the wall, so the difference in this indicator of these structures will be large enough to sharply contrast their image. Thus, the contours of the vessels and their lumen are normally identified quite clearly, while the walls of the arteries are visualized on the screen of the ultrasound device as bright structures, and the lumen corresponds to Fig. 3.23. An example of a duplex scan of a vessel appears dark in a large artery (common carotid artery) (Figure 3.22). healthy person. Explanation in the text.
neck acoustic resistance than the wall, so the difference in this indicator of these structures will be large enough to sharply contrast their image. Thus, the contours of the vessels and their lumen are normally identified quite clearly, while the walls of the arteries are visualized on the screen of the ultrasound device as bright structures, and the lumen corresponds to Fig. 3.23. An example of a duplex scan of a vessel appears dark in a large artery (common carotid artery) (Figure 3.22). healthy person. Explanation in the text.
Increased blood velocity with fetal anemia has been reported in the carotid arteries, descending aorta, and umbilical vein. Intracardiac and venous studies Dopplers do not accurately predict anemia 9. Fetal aploma 16 and splenic artery 17 have also been evaluated with variable success. The use of angular independent measures or measures that require angle correction are not sensitive enough to detect changes in velocity associated with anemia 1.
The middle cerebral artery became suitable choice when assessing the fetus for anemia. However, the method for obtaining peak systolic velocity at mean cerebral artery has crucial to receive reliable results. The apex of the fruit is depicted on the axial plane, which includes the septum septum and thalami. The transducer is then moved to the base of the skull until the circle of Willis is visualized. The vessel's chest angle should be close to zero, and the Doppler gate should be located at the center of the vessel directly above its demarcation from the circle of Willis 18.
With vascular pathology, differences in acoustic resistance between the lumen of the vessel, its walls and surrounding tissues decrease, which leads to a decrease in contrast differences between them.
In modern ultrasound diagnostics, devices are used that operate in real-time B-mode, which means that it is possible to obtain images and control the movement of organs in accordance with the natural time course. The undoubted advantages of these devices, which distinguish them favorably from other devices, are: high resolution, the ability to obtain images in any plane and at any scanning angle of the vessel of interest, indispensability when studying moving objects, in particular pulsating vessels.
It should be taken into account that when an ultrasonic wave propagates in different environments energy is lost, and the degree of its absorption depends on the frequency of the ultrasound signal. The higher the frequency, the higher the degree of absorption. Therefore, in ultrasound scanning to locate deep-lying vessels (thoracic, abdominal cavity, retroperitoneal space) use sensors with a frequency of 2.25-3.5 MHz. For echolocation of superficial vessels (limbs, neck), ultrasound sensors with a frequency of 510 MHz are required.
An undoubted progress has been the ability to simultaneously perform D-ultrasound of blood flow in a vessel (duplex scanning, ultrasound angiography) simultaneously with B-scanning. By placing a mark from where the implementation will be carried out 
Rice. 3.24. Ultrasound scanning coronary arteries. A - echogram; Ao
Examination of neck vessels
The fetus should not be active or breathing during the examination. Before this gestational age, the reticuloendothelial system is too immature to successfully destroy sufficient quantity antibody-coated red blood cells to cause significant anemia 24.
The physiological mechanism of this finding has not yet been elucidated. Fetal liver length in normal and isoimmunized pregnancy. Ultrasonographic measurements of fetal spleen in red blood cells - alloimmunized pregnancy. Mean central cerebral artery systolic velocity for diagnosing fetal anemia: the untold story. Venous, arterial and intrauterine bleeding of blood in isoimmunization of erythrocytes. Effect of intravascular fetal transplantation transfusion on fetal intracellular Doppler waveforms. Acute fetal hemodynamic changes after intrauterine transfusion for the treatment of heavy red blood cell alloimmunization. Intrauterine fetal transfusion hemolytic disease. Benefits and risks of caged fetal transfusion after 32 weeks' gestation. Fetal transfusion for alloimmunization of fetal red blood cells during pregnancy. Pulsed Doppler flow velocity signals before and after intrauterine intravascular transfusion for severe fetal erythroblastosis. Pulsed Doppler flow velocity signals in the prediction of fetal hematocrit in highly isoimmunized pregnancies. Diagnosis of fetal anemia using Doppler ultrasound in pregnancy complicated by maternal blood group immunization. Accurate prediction of fetal hemoglobin using Doppler ultrasonography. Noninvasive tests for predicting fetal anemia in pregnancy caused by Kell alloimmunization. Doppler sonography for predicting fetal anemia caused by massive maternal hemorrhage. The value of the average systolic velocity of the middle cerebral artery in the diagnosis of fetal anemia after the intrauterine death of one monochorionic twin. Non-invasive diagnosis by Doppler ultrasonography of fetal anemia due to parvovirus infection. Prediction of fetal anemia in Rh disease by measuring peak mean systolic velocity cerebral artery. Correction of fetal anemia at middle cerebral artery peak systolic velocity. Correlation between middle cerebral artery peak systolic velocity and fetal hemoglobin after 2 previous intrauterine transfusions. Effects of fetal behavioral states on middle cerebral artery peak systolic velocity. Longitudinal measurement of fetal middle cerebral artery peak systolic velocity to monitor pregnancies complicated by red cell alloimmunization: a prospective multicenter intent-to-treat study. Conventional management of maternal red cell alloimmunization compared with management by Doppler estimation of middle cerebral artery systolic velocity.
- Collaborative group for Doppler assessment of blood velocity in anemic fetuses.
- Fetal blood flow velocity of the middle cerebral artery in an anemic fetus.
- Sonographic evaluation of fruit algae fruit.
- Re-evaluating the usefulness of fetal fetal vein diameter in the management of isoimmunization.
- aorta; RVOT - right ventricular outflow tract; LA - left atrium; LCA
- left coronary artery; RCA - right coronary artery. The diagram shows the location of the orifices of the coronary arteries in the projection of the aortic valve leaflets.
The reflected signal can be registered at any depth of the ultrasound beam under image control in B-mode; you can select any part of the vessel in which registration of blood flow velocity is necessary (Fig. 3.23).
Modern ultrasound devices have the ability to combine B-scanning, D-ultrasound and color flow mapping modes, which makes it possible to determine the nature and severity of blood flow disorders depending on the severity of organic changes in the vascular wall. In other words, such devices help to simultaneously evaluate the morphological substrate and functional manifestations of vascular pathology.
Ultrasound of the coronary arteries has not been used in the diagnosis of coronary artery disease widespread. Meanwhile, numerous data have been published on the possibility of visualizing the mouths of the coronary arteries (most often the mouth common trunk LCA) using two-dimensional echocardiography.
It has been shown that the optimal location of the left artery is the apical location of the sensor, in which it is possible to visualize the artery over its maximum extent and often identify the proximal part of the circumflex branch. An obstacle to observing the artery from this approach is severe obesity.
The parasternal ultrasound window is attractive because it allows you to examine the artery with high magnification, since from here it is closest to the sensor (Fig. 3.24). In patients with pulmonary emphysema, the LCA is not detected from this approach due to a decrease in the acoustic window. In these cases, the subcostal approach is preferable.
In healthy individuals, the thickness of the LCA walls is 1-2 mm, the lumen width is 3-6 mm. The internal contour of the arterial wall is smooth. With a visual comparative assessment, the density of the artery wall approaches the density of the adjacent left segment of the aorta and is significantly inferior to the density of the anterior and posterior segments.
U patients with ischemic heart disease An increase in the density of the left artery walls due to atherosclerotic lesions was revealed.
There is evidence in the literature about the possibility of using transesophageal ultrasound to visualize the coronary arteries and study coronary blood flow by Dopplerography and color mapping.
Despite promising preliminary data, according to reputable researchers, the limitations of coronary artery ultrasound are: false positive results and the ability to detect only significant lesions of the coronary arteries - stenoses of at least 50%. In addition, questions specifically
In addition, measurements of intimal medial thickness are associated with increased risk stroke. These trials include diverse populations in Europe and North America to help clinicians gain evidence to support the best clinical practice for asymptomatic carotid artery disease.
Carotid ultrasonography is a two-stage or duplex procedure. The image is usually viewed in shades of gray, which is a scale of brightness. Sometimes color flow information is superimposed on a grayscale image. A probing cursor is placed in the artery and a signal representing the speed of blood flow is generated. The signal has peaks and valleys that correspond to systolic and diastolic blood flow.
- Image processing is carried out using the brightness mode method.
- By convention, the color of the pulsating artery is red.
- This is called color Doppler imaging.
- This allows the speed of blood flow to be measured.
- The signal is visual and auditory.
- Peaks and low tides create a spectrum.
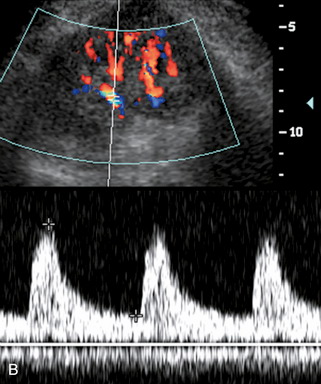
B
A
1
2
3
Rice. 3.25. An example of duplex scanning of the carotid artery at the bifurcation level in a healthy person. A - longitudinal B-scan; B - Dopplerograms of blood flow in the common (1), external (2) and internal (3) carotid arteries.
Pulse echo method - used to image the ship. The original signal is generated in a computer, transmitted through a transducer to the patient's neck, and then bounced off various tissue boundaries. The direction of the pulse and the time elapsed before the signal returns determine the position of the tissue border. Changes in plaque echogenicity, measured by computer-assisted quantitative ultrasound index, may be a marker of plaque instability as well as an indicator of plaque remodeling, thereby providing a means for monitoring anti-atherosclerosis drugs such as statins. An object that picks up very little of the impulse, such as fluid in a cyst, is hypoechoic. An object that picks up most of the signal, such as a heavily calcified plaque, is hyperechoic.
- The sensor detects a return signal.
- The echogenicity of an object in an image determines its brightness.
The effectiveness and sensitivity of ultrasound methods in detecting coronary stenoses cannot be considered completely resolved.
The development of ultrasound technology and catheter technology has led to the emergence of intravascular ultrasound imaging, which allows for qualitative (subjective) assessment biological structures in the area of interest, quantitatively analyze the acoustic parameters (amplitude, frequency, scattering angle of the reflected signal, acoustic density and tissue heterogeneity) characterizing the object being studied: the vascular wall, atheromatous and thrombotic deposits.
In patients with coronary artery disease, intracoronary ultrasound makes it possible to qualitatively and quantitatively determine the severity of stenosis, the morphological structure of the arterial wall and atherosclerotic plaque, as well as assess functional properties (elasticity, rigidity) coronary artery.
However, at present this method seems to be classified as extravagant, and is unlikely to become available to anyone in the coming years. wide application at the clinic.
Ultrasound of the brachiocephalic arteries is now of primary importance in the diagnosis of cerebrovascular pathology caused by atherosclerosis.
Velocity changes in spectral analysis reflect changes in hemodynamics. . Doppler phenomenon. Used to estimate the speed of blood as it passes through the tube. As with pulse echo technology, a pulse is emitted from the transducer at a specific frequency. When the pulse enters the moving blood, it returns back to the probe; however, its frequency varies.
- The change in frequency is known as Doppler shift.
- This shift correlates with changes in blood flow velocity.
- This is called angle dependence.
dT 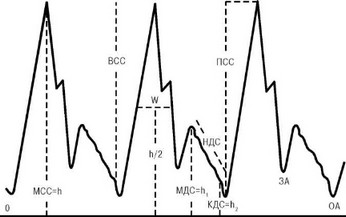
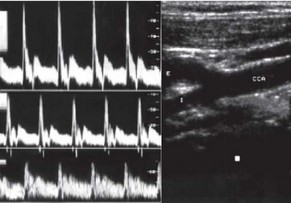
Rice. 3.26. Basic elements of a Dopplerogram of the common carotid artery. Explanation in the text.
ro-sclerosis, thrombosis and embolism, nonspecific aortoarteritis, congenital vascular anomalies. It is believed that with the help of ultrasound it is possible to determine the localization and extent of the lesion with approximately the same accuracy as with arteriography.
The study is carried out with the patient lying on his back with his head tilted back, for which a cushion can be placed under the shoulder blades.
The sensor is installed in the area of the jugular notch and deflected posteriorly. The scanning line runs in the frontal plane. At the same time, the aortic arch with the main branches extending from it is visible on the ultrasound monitor screen: the left common carotid and subclavian arteries. To study the vessels of the neck, the ultrasound sensor is placed alternately on both lateral surfaces in the area of the sternocleidomastoid muscles. The scanning line approximately coincides with the sagittal plane. The common carotid arteries and their bifurcations are usually visible here.
On the echolocator screen, the common carotid artery (CAA) can be traced along its entire length with light, smooth, clearly visible walls. Pulsation synchronous with heart contractions is clearly visible. In addition to the main trunk of the OCA, they are well differentiated
external and internal carotid arteries (ICA), in which characteristic spectra of arterial blood flow are recorded during D-ultrasound (Fig. 3.25).
The peculiarity of blood flow through the brachiocephalic arteries in healthy people is that in none of the phases cardiac cycle it does not reach zero, therefore the following elements are distinguished on the CCA Dopplerogram (Fig. 3.26):
Like light, radiation and audible sound, ultrasound is a wave. The medium is a channel through which the wave passes. Examples of media are air, water and fabric. Frequency is measured in cycles per second, called hertz. A cycle represents one revolution of the wavelength.
Examination of the vessels of the lower extremities
Therefore it is measured in megahertz. Therefore it is measured in kilohertz. The term spatial pulse duration is sometimes used. He equal to the number cycles per pulse multiplied by the wavelength. When ultrasound passes through tissue, some of the signal is lost through scattering, reflection and absorption.
- MSS - maximum systolic velocity (h);
- VSS - increase in systolic velocity;
- MDS - maximum diastolic velocity (hj);
- EDP - end diastolic velocity (h2);
- VAT - diastolic velocity slope;
- PSS - increase in systolic velocity;
- FOR - closure of the aorta;
- OA - opening of the aorta;
- dT is the time from the opening of the aorta to the maximum PVR;
- SA - systolic acceleration (SA = PSS: dT);
- CRI - circular resistance index (CRI/MCR);
- W is the width of the curve at half the MCC level.
In the spectral analysis of a Dopplerogram to determine stenosis of the carotid arteries, three main signs are distinguished: a change in the peak systolic frequency, the magnitude of the spectral expansion of the Doppler signal, and the shape of the spectrogram envelope.
With the introduction of B-scanning methods and duplex study it became possible to document the evolution of athero-

Rice. 3.27. Scheme for determining the degree of artery stenosis according to ultrasound B-scan data. Explanation in the text.
sclerotic plaque from the moment of its appearance until the development of stenosis or occlusion of the artery.
In one of our studies, 2300 ultrasound angiographies of the carotid arteries were performed in screening mode in patients with various cardiovascular diseases, but in the absence of clear clinical manifestations chronic cerebrovascular insufficiency (CVI). Among all those examined, the most common (84%) pathology was ischemic heart disease.
A separate group consisted of 54 patients with atherosclerotic lesions of the brachiocephalic arteries and clinical signs of CCVD II-IV degrees. For patients in this group, in addition to ultrasound of the carotid arteries, ascending cerebral angiography and carotid endarterectomy surgery were performed, followed by macro- and microscopic analysis of biopsy surgical material (Professor I.V. Sukhodolo).
The echo chambers SSD-280 (Aloka, Japan), Ultramark-9 HDI (ATL, USA) and a high-frequency (7.5 MHz) linear probe were used in the work. Two-dimensional scanning of the carotid arteries was performed in longitudinal and transverse projections from the anterolateral surface of the neck at maximum abduction of the holo-
Qualitative assessment of the Doppler spectrum
Therefore, the higher the machine frequency, the greater the attenuation, and the less can be displayed at a greater distance from the probe. On the other hand, higher frequencies mean shorter wavelengths and better resolutions. Therefore, there is a trade-off in frequency regulation.
Blood flow may be laminar, disturbed, turbulent, or plugged. When there is no stenosis, the blood flow is laminar. Blood flow is even, with the fastest flow in the middle and slowest at the edges of the vessel. When present small degree stenosis, blood flow becomes impaired and loses laminar quality. Even in normal conditions such flow can be observed around the carotid flask. With even greater stenosis, the flow may become turbulent.
You. To quantify the amplitude, frequency, and intensity of the reflected signal from the gated object, the histometric analysis program built into the device was used.
In patients with coronary artery disease, atherosclerotic lesions of the carotid arteries were detected in every fourth case. Most often (83.3%) plaques were localized in the upper third and bifurcation of the CCA. Asymmetrical lesions were observed four times less frequently than bilateral and “multi-story” lesions. Moreover, the latter type of lesion in patients with chronic CVN was established in 85.2%. In 8 patients with coronary artery disease, asymptomatic unilateral stenosis of the ICA of more than 75% of the vessel lumen was detected. It should also be noted here that in patients with CCVN syndrome it was not possible to trace the parallelism between the degree of stenosis carotid arteries and the severity of the neurological deficit. This confirms the literature data that in 15-20% of cases, even complete unilateral occlusion of the ICA can be asymptomatic.
When comparing the frequency of detection of carotid stenoses using ultrasound and radiocontrast angiography correlation analysis showed high agreement (r=0.789; рlt;0.01) with the results of both methods. However, in our opinion, the use of biaxial ultrasound makes it possible to more accurately determine the degree of arterial stenosis. This is due to the fact that when measuring the diameter of a vessel in one longitudinal projection, the true value of stenosis is distorted, especially with eccentric plaques, while the transverse ultrasound
scanning makes it possible to determine the cross-sectional area of the artery and the degree of its stenosis (Fig. 3.27).
During the study of carotid stenoses, our attention was drawn to the heterogeneity of signal reflection intensity, which could reflect the peculiarities of the morphological structure of atheromatous deposits. Initially, among all ultrasound findings, two types of plaques were identified
Quantitative Doppler sonographic parameters of arterial blood flow
The Reynolds number determines the level at which turbulent flow occurs. This is known as Poiseuille's law. Thus, during normal hemodynamics, when the length of the vessel increases or the viscosity of the fluid increases, resistance occurs. As the radius of the vessel increases, the resistance decreases significantly.
In a stenotic vessel, the volume flow remains constant. The continuity rule states that the volumetric flow remains constant regardless of the degree of constriction. Therefore, when the diameter of the vessel decreases, the blood velocity increases to maintain volumetric flow.
- dense (“hard”) and loose (“soft”).
The second category of plaques differed significantly
significant (30-40 dB) intensity of the reflected signal, the histometric analysis of which exceeded the level of signal intensity from the vascular wall. These plaques were classified as dense or homogeneous.
Histometric decomposition of the reflected ultrasound wave makes it possible to evaluate the consistency of the plaque by the maximum amplitude of the echo signal intensity, and its structure (homogeneity, heterogeneity) by the frequency of occurrence of the maximum level in the entire spectrum of the signal (Fig. 3.28).
B-scan histometric analysis comparison atherosclerotic plaques and the results of a histomorphological study of surgical material obtained after carotid endarterectomy (54 patients), made it possible to identify well-defined echomorphostructural criteria for the classification of atherosclerosis. Based on the massiveness of the inclusion of coarse calcific and fibrous conglomerates in the plaque, the presence of caseous necrosis and swelling, which were reflected in ultrasound data, all plaques were divided into 3 types:
- Type 1 - “soft”, loose plaques with low acoustic density and echo signal amplitude in the range from 8 to 18 dB (Fig. 3.28.a);
- Type 2 - heterogeneous plaques with a wide range of amplitude characteristics of the echo signal intensity (Fig. 3.28.b);
- Type 3 - dense, homogeneous plaques with a high frequency of histogram amplitudes in the echo signal intensity band from 19 to 35-40 dB Fig. 3.28.c);
Our observations of the localization of atherosclerotic plaques are not without curiosity. different types in the carotid basin (Fig. 3.29). Thus, type 1 plaques in 90% of cases were located in the lower and middle thirds of the CCA, in a number of cases circumferentially narrowing the lumen of the vessel for up to 2 cm. Plaques heterogeneous structure(type 2) were more common (83%) in the upper third and in the region of the bifurcation of the CCA. Atheromatous deposits of the 3rd (homogeneous) structural type in 94% of cases were localized in the bifurcation area and at the ostia of the ICA; Such plaques in 34% of cases had a concentric shape with fragments protruding into the lumen of the vessel, in 8% they had an irregular shell-like shape, most likely due to ulceration of the surface of the plaque. Among all patients with detected atherosclerosis of the carotid arteries, 12% had a combination of plaques of different structural types in one vessel and “multi-level” damage to the CCA and ICA.
It is important to note that, although we did not find a direct relationship between the degree of stenosis of the carotid arteries and the severity of clinical manifestations of chronic venous insufficiency, we found a connection between the structural types of atherosclerotic vascular lesions and the characteristics clinical symptoms. Thus, in 173 patients with ICA stenosis less than 75% at 3rd (dense, homogeneous) structural type plaques, neurological deficit was observed only in 5% of cases, while the presence of loose and heterogeneous plaques in 64% of patients was accompanied neurological disorders of varying severity (candidate of medical sciences
M.P. Plotnikov).
Taking into account the above, when assessing atherosclerotic lesions of the carotid arteries using B-angioscanning, it seems appropriate to us to determine not only the degree of vascular stenosis, but also the intensity of the echo signal, which characterizes the structural features of atheromatous overlays, which, in turn, has been confirmed almost complete coincidence of ultrasound results with histomorphological examination data.
As mentioned above, currently duplex scanning of the carotid arteries (see Fig. 3.22) is the main method for diagnosing carotid arteries
rotid stenoses. Standardized duplex ultrasound is the basis of multicenter international studies, such as the “Asymptomatic Carotid Stenosis and Risk of Stroke” (ACSRS) and the “Asymptomatic Carotid Surgery Trial” (ACST), in which we participated. According to some researchers, duplex ultrasound is superior in diagnostic value to angiography even in the preoperative examination of patients with carotid atherosclerosis. Here is what Professor P.R.F. Bell from Great Britain writes: “In our practice, angiography is not performed unless there is a need for it.” special indications, we rely solely on the nature of the lesion as determined by duplex scanning. Angiography is prescribed if there is a proximal or distal break in the image during duplex scanning, and it is not performed on all patients. We had no problems complying of this rule in more than 300 cases of carotid endarterectomies.”
Duplex scanning allows you to clearly visualize the atherosclerotic plaque and determine characteristic changes blood flow in the area of stenosis (Fig. 3.30).
In case of ICA stenosis, the following most important changes are revealed on Dopplerograms:
- section of artery with increased speed blood flow in the area of narrowing of the lumen of the vessel by an atherosclerotic plaque (Fig. 3.30.b);
- a section of an artery with turbulent blood flow, expressed in a typical superposition of Doppler high-frequency signals (associated with an increase in flow velocity) and low-frequency signals (due to vibration of the vessel walls) (Fig. 3.30.c);
- decrease in blood flow velocity in the ICA by 30% or more compared to the contralateral artery;
- decrease in the diastolic component of blood flow velocity in the CCA compared to the contralateral artery.

Rice. 3.31. Ultrasound classification of atherosclerotic plaques in the carotid arteries. A - schematic representation of the echomorphostructure of plaques; B - ultrasound image of plaques (indicated by arrows). Other explanations are in the text.
In modern foreign literature, to unite such atherosclerotic lesions of the carotid arteries, such a concept as “embologenic potential of a plaque with an unstable morphological structure” has been defined.
Modern ultrasound devices of the 4th-5th generation are equipped special programs computer image processing, which makes it possible to accurately measure the acoustic parameters of the echo signal, which in turn makes it possible to analyze in detail the structural characteristics of the object being studied, in particular - morphological features atherosclerotic plaques.
Based on the ultrasound results, it was proposed various classifications carotid atherosclerotic plaques. For example, they are divided into homogeneous and heterogeneous; soft, dense and calcified plaques are also distinguished. The classification described in 1993 and which has found its application in the international multicenter study according to the ACSRS protocol. In this  classification, 5 echo types of atherosclerotic plaques of carotid localization are identified (Fig. 3.31).
classification, 5 echo types of atherosclerotic plaques of carotid localization are identified (Fig. 3.31).
Type I: homogeneous echo-negative (soft) plaques with (or without) echo-positive (dense) cap;
Type II: predominantly echo-negative plaques with more than 50% echo-positive components;
Type III: predominantly echo-positive plaques with more than 50% echo-negative inclusions;
Type IV: homogeneous echopositive (dense) plaques;
Type V: plaques that cannot be classified because extensive calcification creates an intense acoustic shadow.
Clinical comparison revealed that echo-positive, dense fibrous plaques with a thick fibrous cap are more often
Table 3.1.
Correlation of the ankle-brachial index (ABI) with the severity of clinical manifestations arterial insufficiency lower limbs.
LBI value, conventional units. Clinical sign
1.2±0.1 normal
0.6±0.2 intermittent claudication
0.3±0.1 ischemic pain at rest
- 1 ±0.1 impending tissue necrosis

occur in asymptomatic patients and are considered as plaques with a stable morphostructure. Echo-negative plaques, soft, with rich lipid deposits or with hemorrhages, were much more often found in patients with symptoms of chronic CVN, and were associated with a high incidence of cerebral strokes.
This classification is considered more reliable in dynamic observation for patients with carotid stenoses in comparison with an objective neurological examination, since the proposed gradations of atherosclerotic plaques make it possible to better identify carotid lesions with high risk ischemic stroke.
In conclusion, it remains to briefly mention that today the only real means of eliminating stenosis and preventing stroke remains the operation of carotid endarterectomy, one of the aspects of which is the problem of restenosis. It has been shown that within two years after surgery, restenosis is usually associated with hyperplasia of the endothelium and intimal smooth muscle cells, and in more late dates- with a newly formed atherosclerotic plaque. In connection with
IN
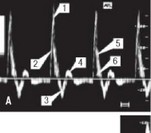
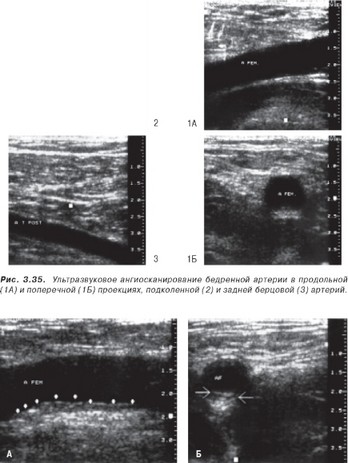
Rice. 3.33. An example of an ultrasound spectrogram of the femoral (A), popliteal (B) and posterior tibial (C) arteries of a healthy person.
- - systolic peak; spectrogram waves of direct (2), reverse (3) and reflected (4) blood flow; 5 - frequency band of the spectrogram envelope; 6 - systolic “window”.
Therefore, it is quite obvious that in the long term postoperative observation For such patients, the method of choice is high-quality duplex ultrasound of the carotid arteries.
Ultrasound of the abdominal aorta and main arteries of the lower extremities makes it possible to determine the level of segmental occlusion, the severity of stenotic vascular lesions and the severity of regional circulatory disorders in patients with OANK.
In angiosurgical practice, the most common is Doppler ultrasound (flowmetry), which makes it possible to evaluate pulse blood flow, systolic pressure (Fig. 3.32) and blood flow velocity in the arteries. With OAANC it is important diagnostic indicator is the regional level systolic pressure in different segments of the limbs compared with the value of blood pressure in the brachial artery.
The study is performed at horizontal position sick. A sphygmomanometer cuff 18 cm wide is applied to the area of the limb being examined (thigh, lower leg); The ultrasound sensor is installed in the projection of the artery at an angle of 45° towards the blood flow; the appearance of the first signal when air is released from the cuff indicates the value of systolic blood pressure in this segment. The pressure in the brachial arteries is measured in the same way, after which the regional systolic pressure index is calculated as the ratio of the pressure in the leg segment to the pressure in the brachial artery. In healthy people, this index usually exceeds 1.0.
In patients with OAANK with degree II ischemia, the pressure index on the thigh ranges from 0.9 to
- 8. The ankle-brachial index (ABI) decreases to approximately 0.7. For ischemia III degree LBI is reduced to 0.5. For ischemia
- the degree of LBI drops to 0.3 and below. In other words, with an occlusive lesion Fig. 3.34. arteries of the lower extremities, decreased LBI
abdominal-HoiA of the aorta (AO) Graphic registration of D-ultrasound allows-
healthy person in
longitudinal (A) and
transverse (B)
projections.
Rice. 3.36. Ultrasound image atherosclerotic plaque (indicated by arrows) in the femoral artery during longitudinal (A) and transverse (B) scanning. 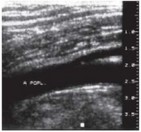
It is not possible to evaluate the qualitative and quantitative characteristics of blood flow in the vessels of the extremities (Fig. 3.21, 3.33). Qualitative characteristics includes an assessment of the spectrogram envelope and the value of spectral expansion. Normally, there are 3 waves of the spectrogram: direct, reverse and reflected blood flow; a narrow frequency band is located along the spectrogram envelope; a “window” is formed under the systolic peak (Fig. 3.33). ![]() With occlusion of the aortoiliac segment, the spectrogram of the femoral artery shows a violation of the shape of the envelope, the disappearance of reverse and reflected blood flow, an increase in the time of rise of the curve and a decrease in the peak systolic frequency. The same changes are observed in the blood flow through the popliteal artery in patients with occlusion of the femoral segment.
With occlusion of the aortoiliac segment, the spectrogram of the femoral artery shows a violation of the shape of the envelope, the disappearance of reverse and reflected blood flow, an increase in the time of rise of the curve and a decrease in the peak systolic frequency. The same changes are observed in the blood flow through the popliteal artery in patients with occlusion of the femoral segment.
With stenosis of the iliac and femoral arteries, spectrograms from distal vessels show blunting of the apex, disappearance of the wave of reverse blood flow, and a decrease in peak systolic frequency
The B-scan method makes it possible to visually assess atherosclerotic lesions of the abdominal aorta and its main branches.
According to the literature, the use of ultrasound angioscanning makes it possible to obtain an image of the aorta in all healthy individuals. Scanning in the longitudinal plane, as well as in the transverse one, gives results. 3.37. ultrasound of the common femoral (A), the ability to study the aorta on the mak-
popliteal (B) and posterior tibial simal length. At
(B) the arteries of a healthy person in this mode, the aorta has the appearance of a tubular
duplex scanning.
structure gradually tapering distally. Normally, the walls of the aorta have a smooth, even contour, their thickness does not exceed 3 mm. The wall of the aorta is much thicker than the wall located next to the inferior vena cava. In both scanning planes, the aortic lumen (2.0-2.4 cm in diameter) is homogeneous, does not contain any inclusions or reflected signals, and has dark color(Fig. 3.34). Distinctive feature of the aorta is a pulsation clearly visible during B-scanning throughout the entire length of the aorta, coinciding with heart contractions.
With a transverse scan in the area of the aortic bifurcation on both sides of the spine, two small, 1.11.2 cm in diameter, round pulsating formations can be distinguished - the common iliac arteries.
The iliac arteries, both on the right and on the left, can be traced for 6-8 cm in the distal direction from the aortic bifurcation. They have the appearance of tubular structures with even, smooth contours of the internal 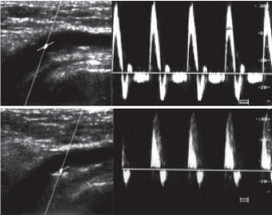
1
2
A
B
Rice. 3.38. Duplex scanning of non-stenotic atherosclerosis of the femoral artery.
- - the mark is installed in the central part of the vessel lumen. The amplitude and configuration of the blood flow spectrogram (A) does not differ from the norm (see Fig. 3.33.A).
- - the mark is installed above the plaque. The Dopplerogram (B) shows a decrease in the velocity and turbulent nature of the blood flow: a decrease in the systolic peak, an expansion of the frequency spectrum, the disappearance of the “window” and waves of reflected blood flow.
on the surface of the walls and clearly visible pulsation. Overall diameter iliac arteries equal to 1.1±0.1 cm, and the external iliac
- 0.9±0.1 cm.
The walls of peripheral arteries affected by atherosclerosis have uneven contours(Fig. 3.36). Their reflectivity is different: the maximum echo signal is given by calcified plaques, other parts of the wall have a lower reflection intensity, but it is always higher than that of the walls of an unaffected vessel.
In places of arterial stenosis, as a rule, areas of wall calcification, which are characterized by a higher echo density, are clearly visible. However, unlike complete occlusion, the lumen of the vessel is always preserved.
With stenosis, the phenomenon of disappearance of pulsation of the artery walls is observed. Local stenoses cause a hard-to-see disappearance of pulsation in a small area of the artery. In the case of extended stenosis, a decrease in pulsation is clearly noticeable when approaching the area of stenosis
To study the abdominal aorta, celiac, mesenteric and renal arteries, we use a 2.5-5 MHz convex sensor.
Click on pictures to enlarge.
 |
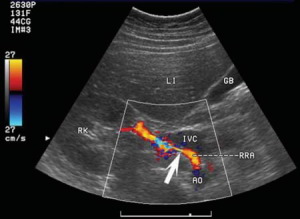
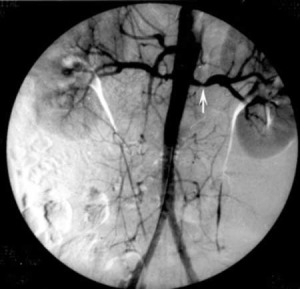
|
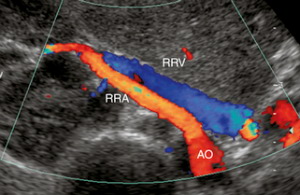
| Photo. The renal arteries arise from the abdominal aorta just below the superior mesenteric artery- at the level of the II lumbar vertebra. The renal vein is located anterior to the renal artery; at the hilum of the kidney both vessels are located anterior to renal pelvis. The right renal artery is the only large vessel, which passes behind the inferior vena cava. The left renal vein passes through the “tweezers” between the aorta and the superior mesenteric artery. A ring-shaped left renal vein is often found, when one branch is located in front and the other behind the aorta. | |
First, let's evaluate the size of the kidney, the thickness of the parenchyma, and the condition of the pyelocaliceal complex. Next, we will trace the aorta from the celiac trunk to the bifurcation in the gray scale and color flow modes. In the presence of atherosclerotic plaques in the aorta, stenosis of the orifices is likely renal artery, especially in the elderly or sick diabetes mellitus. If possible, locate the renal arteries on a cross-section of the aorta when scanning through the anterior abdominal wall by moving the transducer from the superior mesenteric artery along the aorta. The right renal artery is easier to find than the left. Let us trace its course from the aorta to the hilum of the kidney, where it is divided into segmental branches. The left renal artery is better visible in the lateral position. Inspect carefully abdominal aorta and kidneys to identify additional branches of the renal arteries from lower sections aorta or iliac arteries.
 |
 |
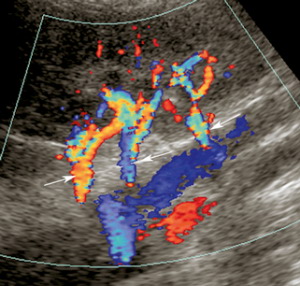 |
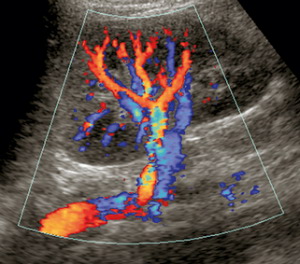
| Photo. A - With CDK, it is clear that the right renal artery (RRA) departs from the aorta (AO) and goes to the hilum of the kidney; Anterior to the right renal artery is the right renal vein (RRV). The acoustic window is the liver parenchyma. B — When performing a central dorsal maneuver in a position on the right side, the acoustic window serves as left kidney— it is clearly visible how the left renal artery and vein at the hilum of the kidney are divided into segmental and interlobar vessels. B - Several accessory renal arteries (arrows) go to the left kidney. | ||
 |
 |
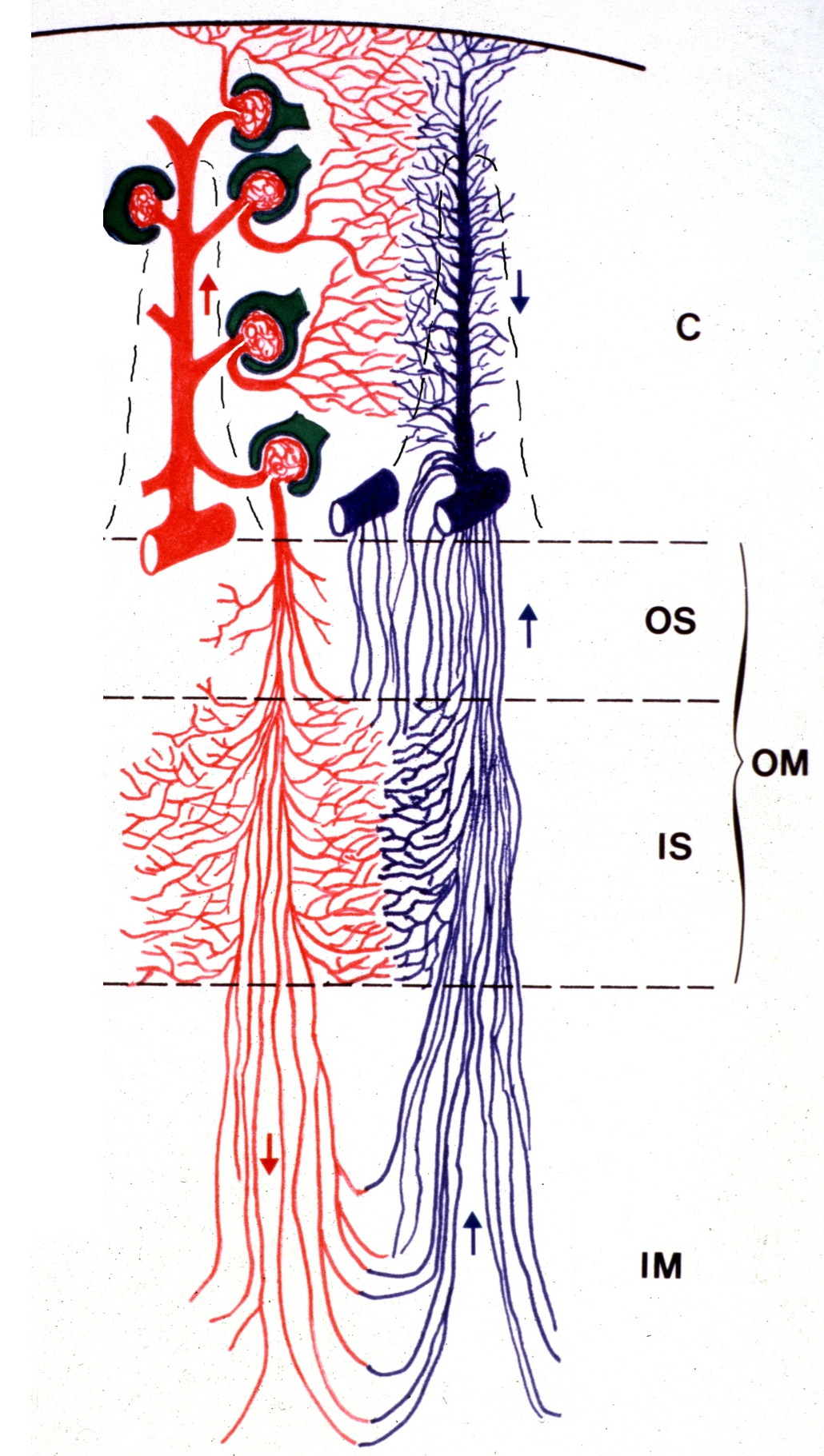 |
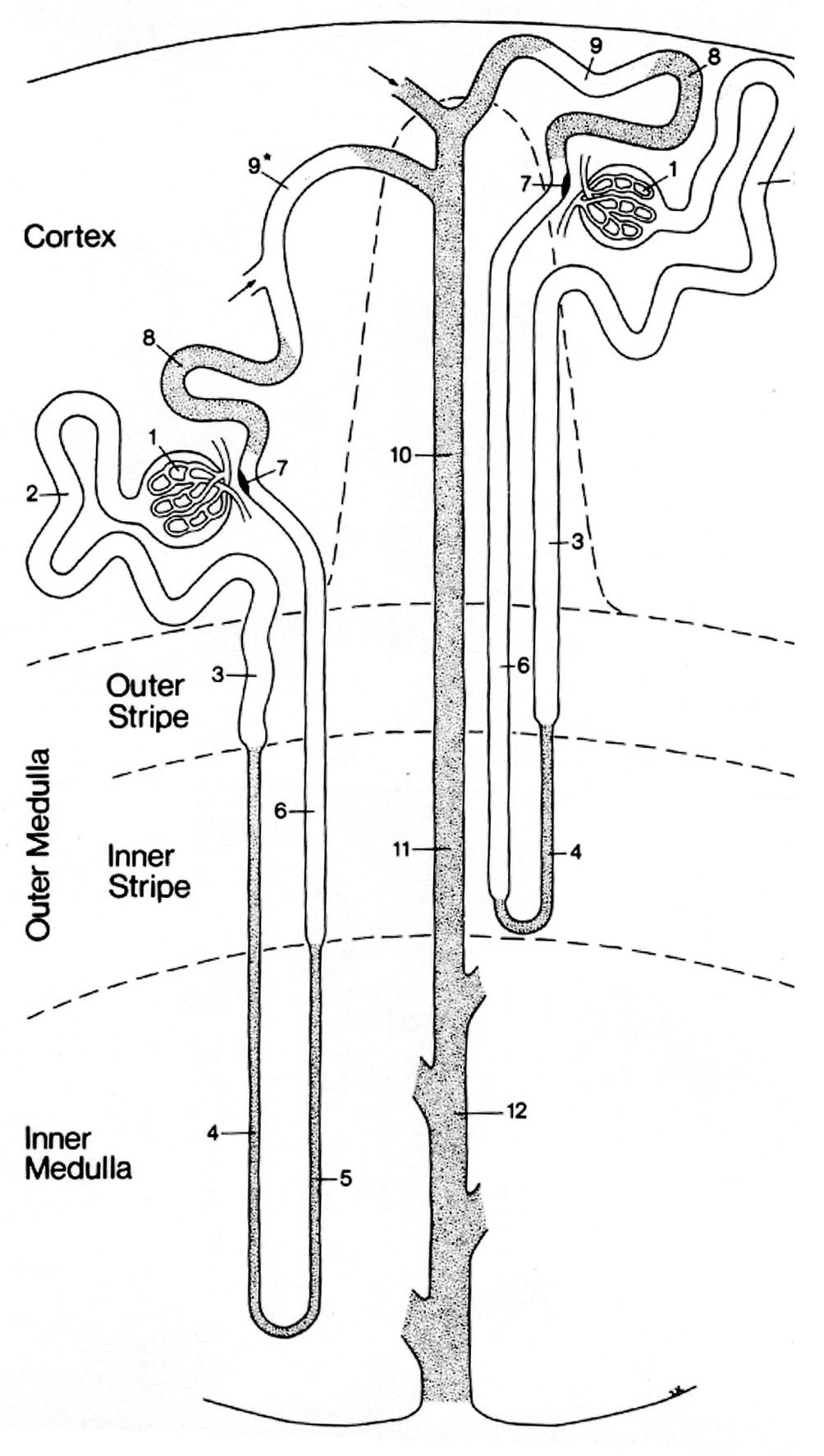
| Photo. A - At the hilum of the kidney, the main renal artery is divided into five segmental ones: posterior, apical, superior, middle and inferior. The segmental arteries pass through the sinus and divide into interlobar arteries, which are located between the pyramids in the renal parenchyma. The interlobar arteries continue into the arcuate (aa. arcuatae) → interlobular (aa. interlobular) → afferent arterioles of the glomeruli (vas afferens) → capillary glomeruli (glomeruli). Blood from the glomerulus flows into the efferent arteries, from which direct venules (venulae rectae) and interlobular veins (venae interlobulares) are formed. Interlobular veins and straight venules form arc veins (vv. arcuatae). Then the blood enters the interlobar (vv. interlobares) → segmental (vv. segmentares) → renal veins (v. renales) → inferior vena cava. | ||
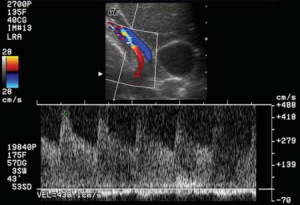
The renal artery at its exit from the aorta, in the proximal, middle and distal segments, as well as the apical, middle and inferior segmental arteries should be assessed. We conduct a spectral analysis of the Doppler curve at at least seven points on both sides. ABOUT pay attention to high-velocity flow and turbulence, as these may be associated with stenosis.
Important!!! The angle between the scanning plane and the vessel should be from 30° to 60°.
We evaluate peak systolic (PSV) and end-diastolic (EDV) blood flow velocities, as well as acceleration time (Ao AT). Peak systolic(PSV) and end diastolic (EDV) velocities are determined at the top of the highest systolic peak and at the end of diastole, respectively. Acceleration time(Ao AT) is determined from the beginning of the systolic movement to the highest systolic peak. Systolic acceleration(Ao Accel) is determined by dividing the peak systolic change in blood flow velocity by the acceleration time. Resistance index(RI) = (peak systolic flow velocity - end-diastole flow velocity) / peak systolic flow velocity.
The normal spectrum of renal arteries and renal parenchymal vessels has a pronounced systolic peak with antegrade diastolic flow throughout the cardiac cycle. Normally in adults, the peak systolic velocity (PSV) in the renal artery is 100-180 cm/s, end-diastolic velocity(EDV) - 25-50 cm/s; RI on the main renal artery in the area of the renal hilum should be less than 0.7, and on the interlobar arteries 0.34-0.74, the difference in RI of the right and left kidney does not exceed 0.05.
 |
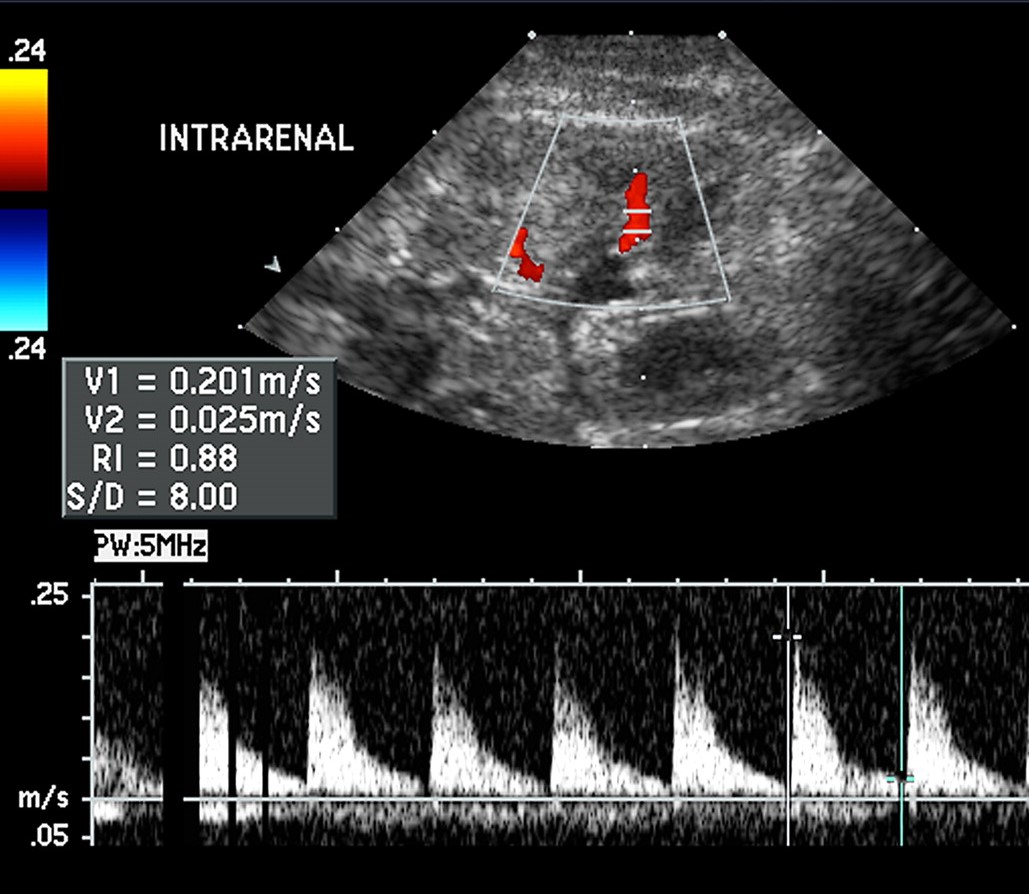 |
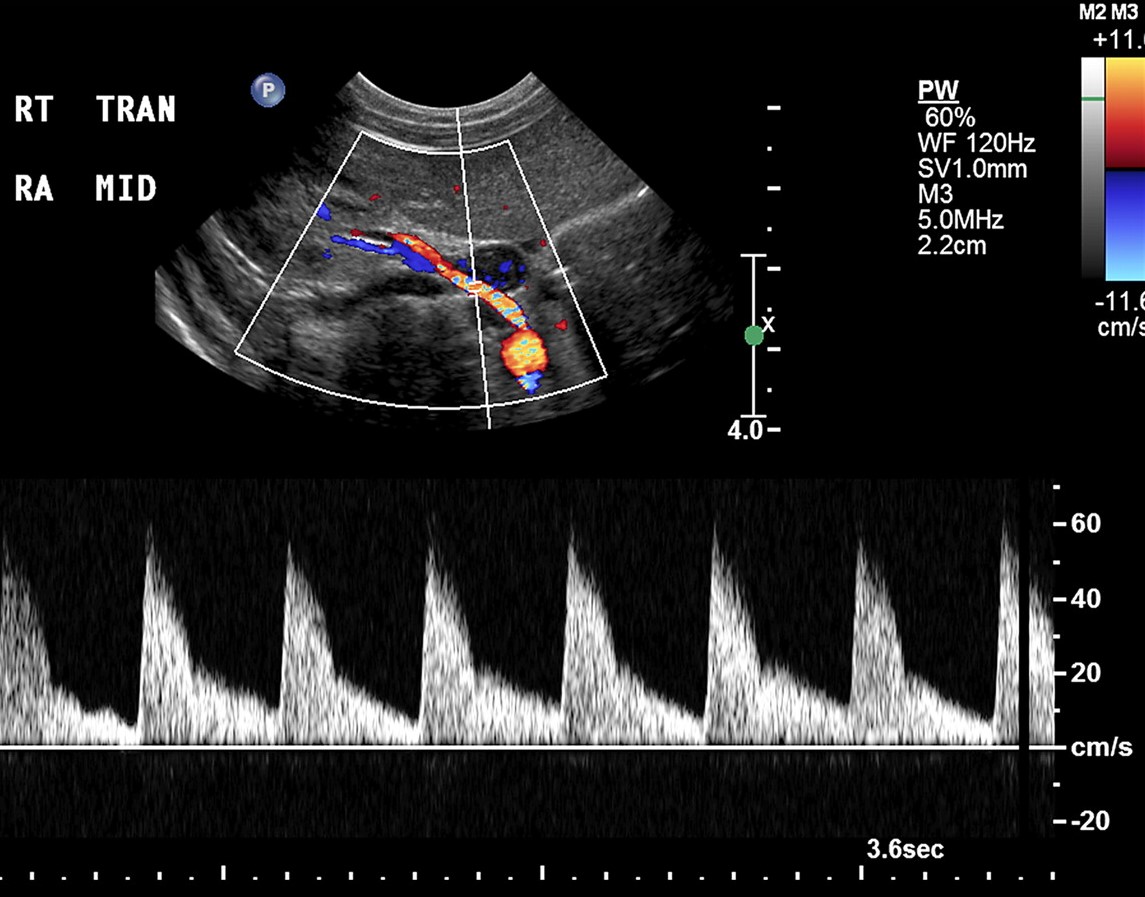
| Photo. A, The spectrum from the midportion of the right renal artery in a 2-day-old girl shows a pronounced systolic peak with antegrade flow throughout diastole. B, The spectrum from the intrarenal artery in a preterm 26-day-old girl shows a relatively high resistance (RI 0.88), which is considered normal for preterm neonates. | |
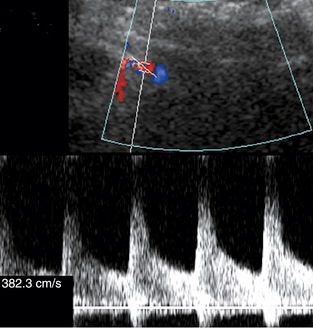
Hemodynamically significant renal artery stenosis is usually determined when the diameter decreases by 50-60%. Criteria for diagnosing hemodynamically significant renal artery stenosis:
- Peak systolic velocity in the renal artery is 180-200 cm/sec or more;
- The ratio of peak systole in the renal artery to peak systole in the aorta at the level of the renal artery (RAR) exceeds 3.3;
Important!!! Young patients without stenosis may have high (above 180 cm/sec) systolic peak values of the aorta and its branches. Elderly patients with severe heart failure and poor cardiac output may have a low peak systolic even in the region of stenosis. The ratio of peak systole in the renal artery to peak systole in the aorta at the level of the renal artery makes it possible to level out these features.
- With renal artery stenosis, blood flow in the distal sections (intrarenal vessels) is attenuated—the “tardus-parvus” effect. Tardus means slowly or late, and parvus small or little. Tardus indicates that systolic acceleration is slow and the time to reach peak systolic velocity increases. Parvus indicates that the systolic peak is low in height, which means the flow rate is slow. An acceleration index of less than 300 cm/sec 2 or an acceleration time of more than 0.07 seconds is considered abnormal and indicates renal artery stenosis in 60% of cases. Some authors use an acceleration of 0.10 or 0.12 seconds as a cutoff for significant stenoses, which improves specificity.
- The ratio of the peak systolic velocity of the renal and interlobar arteries (RIR) should not exceed 5.
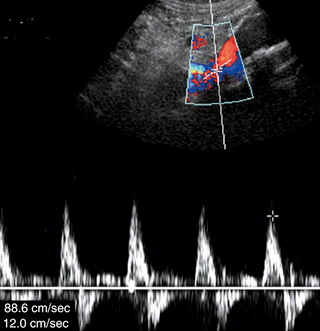
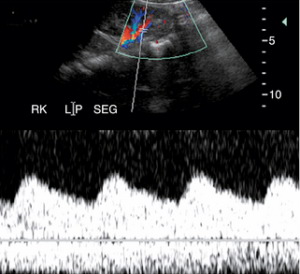
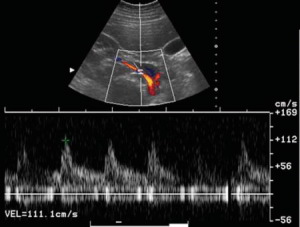
| Photo. Stenosis of the right renal artery on Doppler ultrasound. A - Increased peak systolic velocity of the renal artery - 382.3 cm/sec. B — Peak systolic velocity of the aorta at the level of the renal arteries — 88.6 cm/sec. The renal-aortic ratio is 4.3, indicating significant renal artery stenosis. B - There is signal damping on the intrarenal segmental arteries - a tardus-parvus curve is characteristic. Note the rounded contour of the early systolic peak and the long systolic acceleration time. | ||
 |
 |
 |
Important!!! Renal artery stenosis can be suspected by indirect signs- attenuation of the Doppler signal in segmental or interlobar arteries. Assessment of intrarenal blood flow is easy, accurate and quick way detection of renal stenosis.
But this method cannot be used alone. The shape of the Doppler curves of the intrarenal arteries depends on the elasticity of the vessels, the resistance of the microvasculature, as well as on the incoming blood flow. In patients with changes in small vessels kidneys, for example, with diabetic nephropathy, the phenomenon of signal attenuation in the intrarenal vessels even with high level renal artery stenosis can be destroyed. Conversely, attenuated intrarenal waves can be seen in the absence of significant renal artery stenosis in patients with aortic stenosis or aortic occlusion.
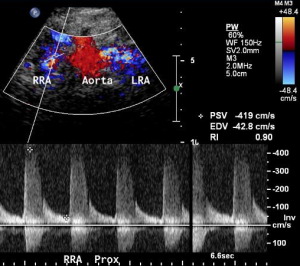
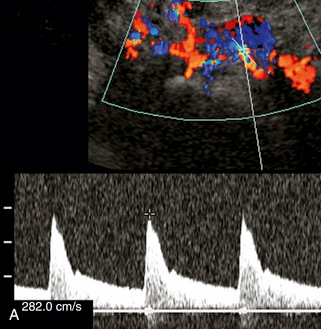
| Photo. A - Left renal artery stenosis: peak systolic velocity - 419 cm/sec, end-diastolic velocity - 42.8 cm/sec, resistance index - 0.9. B - Peak systolic velocity in the left renal artery is 282 cm/sec, indicating stenosis. Note (Panel B) that the Doppler of the intrarenal vessels appears normal. The stenosis was confirmed by magnetic resonance angiography. | ||
 |
 |
 |
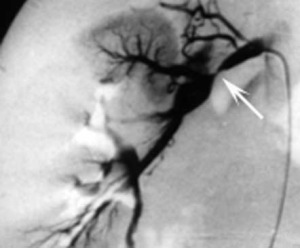
| Photo. Severe stenosis of the right renal artery in young man: A - The angiogram shows pronounced stenosis in the middle segment of the right main renal artery (thick arrow) and the accessory artery (thin arrows). B - Peak systolic velocity at the renal artery is only 111 cm/sec - spectral Doppler does not see stenosis. B - Color Doppler shows narrowing of the right renal artery (arrow). AO—aorta; G.B. gallbladder; IVC—inferior vena cava; LI—liver; RK - right kidney; RRA—right renal artery. | ||
 |
 |
 |
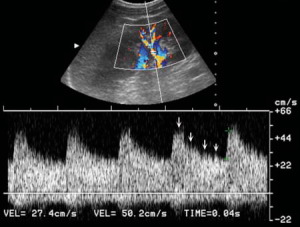
| Photo. Severe stenosis of the middle segment of the right renal artery in elderly woman. A - Peak systolic velocity (PSV) at the renal artery 438 cm/sec, renal-aortic ratio 5.1 (438/86). B — Spectral analysis of the interlobar artery shows changes typical for stenosis: low PSV - 14 cm/sec; systolic acceleration time 0.18 seconds, IR 0.43, renal/interlobar artery ratio (RIR) 438/14=31.3. B — Angiography confirmed stenosis in the middle segment of the right renal artery. | ||
 |
 |
 |
| Photo. Spectral Dopplerography of the kidneys in an elderly man revealed changes at the level of the intrarenal arteries: A - Spectral analysis of the segmental artery shows a turbulent and chaotic nature of the blood flow - signal bursts along the contour (arrows), but the time of systolic acceleration is not changed - 0.04 seconds. B - On the interlobar artery, the blood flow is laminar - a smooth contour, but the systolic acceleration time is increased - 0.13 seconds. C - Angiography shows severe stenosis of the middle segment of the left renal artery. | ||
 |
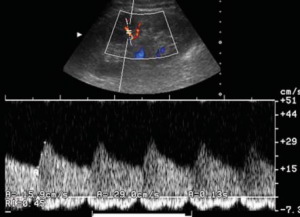 |
 |

