Reduced and increased cardiac ejection fraction. Cardiac output: norm and causes of deviation What is ejection fraction
The amount of blood ejected by the ventricle of the heart into the arteries per minute is an important indicator of the functional state of the cardiovascular system (CVS) and is called minute volume blood (IOC). It is the same for both ventricles and at rest is 4.5–5 liters.
An important characteristic of the pumping function of the heart is given by stroke volume , also called systolic volume or systolic ejection . Stroke volume- the amount of blood ejected by the ventricle of the heart into the arterial system in one systole. (If we divide the IOC by heart rate per minute we get systolic volume (CO) of blood flow.) With a heart contraction of 75 beats per minute, it is 65–70 ml; during work it increases to 125 ml. In athletes at rest it is 100 ml, during work it increases to 180 ml. The determination of MOC and CO is widely used in the clinic.
Ejection fraction (EF) – expressed as a percentage, the ratio of the stroke volume of the heart to the end-diastolic volume of the ventricle. EF at rest in a healthy person is 50-75%, and during physical activity it can reach 80%.
The volume of blood in the ventricular cavity that it occupies before its systole is end-diastolic volume (120–130 ml).
End-systolic volume (ECO) is the amount of blood remaining in the ventricle immediately after systole. At rest, it is less than 50% of the EDV, or 50-60 ml. Part of this blood volume is reserve volume.
The reserve volume is realized when CO increases under load. Normally, it is 15–20% of the end-diastolic value.
The volume of blood in the cavities of the heart remaining when the reserve volume is fully realized at maximum systole is residual volume. CO and IOC values are not constant. During muscular activity, IOC increases to 30–38 l due to increased heart rate and increased CO2.
A number of indicators are used to assess the contractility of the heart muscle. These include: ejection fraction, rate of blood expulsion during the rapid filling phase, rate of increase in pressure in the ventricle during the period of stress (measured by probing the ventricle)/
Blood expulsion rate changes using Doppler ultrasound of the heart.
Pressure rise rate in the cavities of the ventricles is considered one of the most reliable indicators of myocardial contractility. For the left ventricle, the normal value of this indicator is 2000-2500 mmHg/s.
A decrease in the ejection fraction below 50%, a decrease in the rate of blood expulsion, and the rate of pressure increase indicate a decrease in myocardial contractility and the possibility of developing insufficiency of the pumping function of the heart.
The IOC value divided by the body surface area in m2 is determined as cardiac index(l/min/m2).
SI = MOK/S (l/min×m 2)
It is an indicator of the pumping function of the heart. Normally, the cardiac index is 3–4 l/min×m2.
IOC, UOC and SI are united by a common concept cardiac output.
If the IOC and blood pressure in the aorta (or pulmonary artery) are known, the external work of the heart can be determined
P = IOC × BP
P - heart work per minute in kilograms (kg/m).
MOC - minute blood volume (l).
Blood pressure is pressure in meters of water column.
At physical rest, the external work of the heart is 70–110 J, and during work it increases to 800 J, for each ventricle separately.
Thus, the work of the heart is determined by 2 factors:
1. The amount of blood flowing to it.
2. Vascular resistance during the expulsion of blood into the arteries (aorta and pulmonary artery). When the heart cannot pump all the blood into the arteries at a given vascular resistance, heart failure occurs.
There are 3 types of heart failure:
1. Insufficiency from overload, when excessive demands are placed on the heart with normal contractility due to defects, hypertension.
2. Heart failure due to myocardial damage: infections, intoxications, vitamin deficiencies, impaired coronary circulation. At the same time, the contractile function of the heart decreases.
3. Mixed form of failure - with rheumatism, dystrophic changes in the myocardium, etc.
The entire complex of manifestations of cardiac activity is recorded using various physiological techniques - cardiographs: ECG, electrokymography, ballistocardiography, dynamocardiography, apical cardiography, ultrasound cardiography, etc.
The diagnostic method for the clinic is the electrical recording of the movement of the contour of the heart shadow on the screen of the X-ray machine. A photocell connected to an oscilloscope is applied to the screen at the edges of the heart contour. As the heart moves, the illumination of the photocell changes. This is recorded by an oscilloscope in the form of a curve of contraction and relaxation of the heart. This technique is called electrokymography.
Apical cardiogram recorded by any system that detects small local movements. The sensor is fixed in the 5th intercostal space above the site of the cardiac impulse. Characterizes all phases of the cardiac cycle. But it is not always possible to register all phases: the cardiac impulse is projected differently, and part of the force is applied to the ribs. The recording may differ from person to person and from one person to another, depending on the degree of development of the fat layer, etc.
The clinic also uses research methods based on the use of ultrasound - Ultrasound cardiography.
Ultrasonic vibrations at a frequency of 500 kHz and higher penetrate deeply through tissues being generated by ultrasound emitters applied to the surface of the chest. Ultrasound is reflected from tissues of various densities - from the outer and inner surface of the heart, from blood vessels, from valves. The time it takes for the reflected ultrasound to reach the capturing device is determined.
If the reflective surface moves, the return time of the ultrasonic vibrations changes. This method can be used to record changes in the configuration of heart structures during its activity in the form of curves recorded from the screen of a cathode ray tube. These techniques are called non-invasive.
Invasive techniques include:
Catheterization of the heart cavities. An elastic catheter probe is inserted into the central end of the opened brachial vein and pushed towards the heart (into its right half). A probe is inserted into the aorta or left ventricle through the brachial artery.
Ultrasound scanning- the ultrasound source is inserted into the heart using a catheter.
Angiography is a study of heart movements in a field of X-rays, etc.
Mechanical and sound manifestations of cardiac activity. Heart sounds, their genesis. Polycardiography. Comparison in time of periods and phases of the cardiac cycle of ECG and FCG and mechanical manifestations of cardiac activity.
Heart beat. During diastole, the heart takes the shape of an ellipsoid. During systole, it takes on the shape of a ball, its longitudinal diameter decreases, and its transverse diameter increases. During systole, the apex rises and presses against the anterior chest wall. A cardiac impulse occurs in the 5th intercostal space, which can be recorded ( apical cardiography). The expulsion of blood from the ventricles and its movement through the vessels, due to reactive recoil, causes vibrations of the entire body. Registration of these oscillations is called ballistocardiography. The work of the heart is also accompanied by sound phenomena.
Heart sounds. When listening to the heart, two tones are detected: the first is systolic, the second is diastolic.
Systolic the tone is low, drawn-out (0.12 s). Several overlapping components are involved in its genesis:
1. Mitral valve closure component.
2. Closure of the tricuspid valve.
3. Pulmonary tone of blood expulsion.
4. Aortic blood expulsion tone.
The characteristic of the first tone is determined by the tension of the leaflet valves, the tension of the tendon threads, papillary muscles, and the walls of the ventricular myocardium.
Components of blood expulsion occur when the walls of the great vessels are tense. The first sound is clearly audible in the 5th left intercostal space. In pathology, the genesis of the first tone involves:
1. Aortic valve opening component.
2. Opening of the pulmonary valve.
3. Tone of pulmonary artery distension.
4. Aortic stretch tone.
Strengthening of the first tone can occur with:
1. Hyperdynamics: physical activity, emotions.
When there is a violation of the time relationship between the systole of the atria and ventricles.
With poor filling of the left ventricle (especially with mitral stenosis, when the valves do not open completely). The third option of amplifying the first tone has significant diagnostic value.
Weakening of the first sound is possible with mitral valve insufficiency, when the valves do not close tightly, with myocardial damage, etc.
II tone - diastolic(high, short 0.08 s). Occurs when the closed semilunar valves are tense. On a sphygmogram its equivalent is incisura. The higher the pressure in the aorta and pulmonary artery, the higher the tone. It can be heard well in the 2nd intercostal space on the right and left of the sternum. It intensifies with sclerosis of the ascending aorta and pulmonary artery. The sound of the 1st and 2nd heart sounds most closely conveys the combination of sounds when pronouncing the phrase “LAB-DAB”.
To assess the performance of a continuously running human “engine,” many quantitative indicators are taken into account. Among them are cardiac output (CO) and cardiac ejection fraction (CEF).
The norm of these values and comparison with them of the values measured in a particular patient allow the doctor to obtain an objective idea of the functional reserves of the “pumping” function of the myocardium and the existing pathologies in his cardiovascular system.
The information, photos and videos in this article will help the average person understand the essence of these parameters, how they are measured, what affects the indicators of VS and FVS, and whether modern medicine can influence the body to normalize these values.
Cardiac output is the total volume of blood flowing from the heart into the great vessels over a certain period of time or the volumetric velocity of blood flow. Typically, the time unit is equal to 1 minute, so among doctors the term “Minute Volume of Blood Circulation” or its abbreviation “MOC” is more often used.
Factors influencing the value of cardiac output

Cardiac output depends on:
- age and anthropometric indicators;
- human condition – rest (preload), after physical activity, psycho-emotional background;
- the frequency of myocardial contractions and its qualitative characteristics - stroke or systolic blood volume (SVV) flowing from the left ventricle into the aorta, and from the right ventricle into the pulmonary artery, during their contraction;
- the value of “venous return” - the blood volume flowing into the right atrium from the superior and inferior vena cava, into which blood from the whole body collects;
- dimensions of the thickness of the muscle wall and the volume of the heart chambers (see in the figure above).
FYI. The BC parameter is also influenced by specific indicators of the pumping (contractile) ability of the cardiac apparatus and the current state of the general resistance to blood flow of the system of peripheral blood vessels of the general circulation.
Reference values and standard assessment parameters

Today it is quite easy to find out the exact indicators of cardiac hemodynamics. Most of them are calculated by a computer program during a non-invasive echocardiographic ultrasound examination.
The procedure can be done free of charge in a public clinic, performed in a private medical institution or laboratory, and even by calling a specialist with a portable device to your home. The price of the examination ranges from 700 to 6,500 rubles, and depends on the class of equipment.

There are other methods for determining VS and SWS - according to Fick, thermodilution, left ventriculography, Starr's formula. Their implementation is invasive, so they are used in cardiac surgery. A description of their essence will be understandable only to specialists, but for the average person we will clarify that they are intended to monitor the state of the cardiovascular system during operations, monitor the condition of a patient in intensive care, but some are sometimes performed to make an accurate diagnosis.
Whatever methods of measuring VS are used, its reference values in a healthy adult who is in physical rest and psycho-emotional balance are fixed in the range from 4 to 6 l/min, while in one contraction from the left ventricle into the aorta 60 to 100 are pushed ml of blood. Such indicators are considered optimal provided that the heart beats at a speed of 60-90 beats/min, the upper pressure was in the range from 105 to 155, and the lower pressure was from 55 to 95 mm Hg. Art.
Just a note. Unfortunately, echocardiography is not always enough to clarify a cardiac diagnosis. In addition to it, the doctor may prescribe CT tomography, PhonoCG, EPI, CT coronary angiography, and radionuclide diagnostics.
Cardiac output syndromes
A decrease in VS occurs due to a decrease in the speed and volume of “venous outflow”, as well as a violation of myocardial contractility.

The causes of low cardiac output syndrome include:
- Diseases or conditions caused by cardiac origin or complications after cardiac surgery:
- bradyarrhythmia, tachyarrhythmia;
- heart valve defects;
- end-stage congestive heart failure;
- metabolic disorders in the myocardium;
- occlusion of a shunt or main vessel;
- decreased blood volume;
- accumulation of air in the pleural cavity and compression of the lobes of the lungs;
- accumulation of fluid between the layers of the pericardium;
- oxygen starvation of the myocardium;
- a shift in the body’s acid-base balance towards increasing acidity (decreasing pH);
- sepsis;
- cardiogenic shock.
- Non-cardiac processes:
- massive blood loss;
- extensive burn;
- decreased nervous stimulation of the heart;
- sudden dilatation of veins;
- obstruction of large veins;
- anemia;
- carbon dioxide poisoning.
Just a note. Aging of the body, prolonged physical inactivity, fasting, and diets that lead to a decrease in skeletal muscle volume cause persistent low cardiac output syndrome.

High BC is an adequate reaction of the heart in response to physical or psycho-emotional stress. The heart of a marathon athlete is capable of working at its maximum limit - with an increase in venous return and cardiac output by 2.5 times, pumping up to 40 liters per minute.
If the BC indicator is elevated at rest, then this may be a consequence of:
- the initial stage of hypertrophy of the heart walls - “athlete’s heart”;
- thyrotoxicosis;
- arteriovenous fistulas;
- chronic mitral and aortic insufficiency with left ventricular overload;
- low hemoglobin;
- beriberi diseases (vitaminosis B1);
- Paget's pathology (deforming osteodystrophy).
FYI. The increased load on the cardiovascular system during pregnancy causes an increase in CV, which returns to normal after childbirth.
What is cardiac ejection fraction
Among the criteria characterizing cardiac hemodynamics one can also find more “complex” parameters. Among them, Cardiac Ejection Fraction (CEF), which is the percentage ratio of the stroke systolic volume of blood pushed out of the left ventricle during heart compression to the volume of blood accumulated in it by the end of the period of relaxation of the heart muscle (diastole).
This indicator is used to make a prognosis for any cardiovascular pathology.

Reference values
The normal left ventricular ejection fraction at rest is 47-75%, and during psycho-emotional and physical stress its value can reach 85%. In old age, the rate decreases slightly. In children, the reference values at rest are higher – 60-80%.
The value of FVS is determined during radionuclide angiography using the Simpson or Teicholz formulas. The survey form indicates which formula was applied, since discrepancies of up to 10% are possible.
Cardiologists pay attention to FVS in cases when it drops to 45% or below. Such values are a clinical symptom of contractile insufficiency and decreased performance of the heart muscle. Indicators below 35% indicate irreversible processes in the myocardium.
FYI. At the initial stage of any cardiac disease, the ejection rate of the heart fraction does not change due to adaptive processes - thickening of muscle tissue, restructuring of small-diameter vessels and alveoli, increasing strength and/or number of contractions. A change in the value of the FVS occurs when the compensations are exhausted.
Reasons for the decline
Low cardiac ejection fraction occurs due to:
- diseases, infectious and inflammatory processes and myocardial defects;
- heavy load on the heart due to pulmonary hypertension;
- pathologies of the coronary and pulmonary vessels;
- tumor formations and diseases of the thyroid, pancreas, and adrenal glands;
- diabetes mellitus, obesity;
- poisoning with alcohol, tobacco, drugs, .
Attention! Increasingly, cases of decreased myocardial contractility are being recorded in young and mature people who abuse energy drinks.
Symptoms

Despite the fact that low cardiac ejection fraction is a clinical symptom in itself, it has its own characteristic symptoms:
- increased breathing rate, possible attacks of suffocation;
- presyncope and fainting;
- “floaters” or “darkening” in the eyes;
- increase in heart rate to tachycardia levels;
- swelling of the lower extremities (feet, legs);
- numbness of hands and feet;
- gradual increase in liver size;
- pain syndrome (of varying nature and strength) in the area of the heart and abdomen.
Important! Often, people suffering from diseases that are accompanied by a low ejection fraction of the heart look like they are drunk. Their coordination of movement is impaired, their gait becomes unsteady, their tongue becomes slurred, and other speech defects arise.
How to increase cardiac ejection fraction
Treatment of low cardiac ejection fraction is aimed at stabilizing pathological processes, and occurs as part of standard therapy for the disease or condition that causes decreased myocardial performance and correction of left ventricular failure. In addition to hypertensive drugs, the following may be prescribed: antiplatelet agents, blood thinners, anticoagulants, statins, peripheral vasodilators, antiarrhythmic drugs, aldosterone and angiotensin 2 receptor antagonists.

If the cardiac ejection fraction falls below 35%, treatment measures are aimed at improving the quality of life. If necessary, resynchronization therapy (artificial blockade) is performed. In cases of fatal arrhythmias, a pacemaker or cardiovector defibrillator is installed.
And at the end of the article, watch a video with detailed instructions on how to perform an exercise from Chinese health gymnastics that is accessible to everyone, which will help improve the cardiovascular system at the energy level.
When a patient receives test results, he tries to figure out on his own what each value obtained means and how critical the deviation from the norm is. The cardiac output indicator is of important diagnostic value, the norm of which indicates a sufficient amount of blood ejected into the aorta, and a deviation indicates impending heart failure.
Cardiac ejection fraction assessment
When a patient comes to the clinic with complaints of pain in the chest, the doctor will prescribe a full diagnosis. A patient who is encountering this problem for the first time may not understand what all the terms mean, when certain parameters are increased or decreased, how they are calculated.
Cardiac ejection fraction is determined with the following patient complaints:
- heart pain;
- tachycardia;
- dyspnea;
- dizziness and fainting;
- increased fatigue;
- pain in the chest area;
- interruptions in heart function;
- swelling of the limbs.
A biochemical blood test and an electrocardiogram will be indicative for the doctor. If the data obtained is not enough, ultrasound, Holter monitoring of the electrocardiogram, and bicycle ergometry are performed.
The ejection fraction is determined by the following heart tests:
- isotope ventriculography;
- X-ray contrast ventriculography.
Ejection fraction is not a difficult indicator to analyze; even the simplest ultrasound machine shows the data. As a result, the doctor receives data showing how efficiently the heart works with each beat. During each contraction, a certain percentage of blood is ejected from the ventricle into the vessels. This volume is referred to as the ejection fraction. If 60 cm3 of 100 ml of blood in the ventricle enters, then cardiac output is 60%.
The work of the left ventricle is considered indicative, since from the left part of the heart muscle blood enters the systemic circulation. If malfunctions in the left ventricle are not detected in time, there is a risk of heart failure. A reduced cardiac output indicates the inability of the heart to contract at full strength, therefore the body is not provided with the necessary volume of blood. In this case, the heart is supported with medication.
How is ejection fraction calculated?
The following formula is used for calculation: stroke volume multiplied by heart rate. The result will show how much blood is pumped out by the heart in 1 minute. The average volume is 5.5 liters.
Formulas for calculating cardiac output have names.
- Teicholz formula. The calculation is performed automatically by a program into which data on the final systolic and diastolic volume of the left ventricle is entered. The size of the organ also matters.
- Simpson's formula. The main difference is the possibility of getting all sections into the cut of the circle. The study is more revealing; it requires modern equipment.
Data obtained using two different formulas may differ by 10%. The data is indicative for diagnosing any disease of the cardiovascular system.
Important nuances when measuring the percentage of cardiac output:
- the result is not affected by the gender of the person;
- the older the person, the lower the rate;
- a pathological condition is considered to be below 45%;
- a decrease in the indicator of less than 35% leads to irreversible consequences;
- a reduced rate may be an individual feature (but not lower than 45%);
- the indicator increases with hypertension;
- in the first few years of life, in children the emission rate exceeds the norm (60-80%).
Normal EF values
Normally, a greater amount of blood passes through, regardless of whether the heart is currently loaded or at rest. Determining the percentage of cardiac output allows for timely diagnosis of heart failure.

Normal cardiac ejection fraction values
The cardiac output rate is 55-70%, a reduced rate is read as 40-55%. If the rate drops below 40%, heart failure is diagnosed; a rate below 35% indicates possible irreversible life-threatening heart failure in the near future.
Exceeding the norm is rare, since the heart is physically unable to expel more blood volume into the aorta than required. The figure reaches 80% in trained people, in particular athletes, people leading a healthy, active lifestyle.
An increase in cardiac output may indicate myocardial hypertrophy. At this moment, the left ventricle tries to compensate for the initial stage of heart failure and pushes out blood with greater force.
Even if the body is not affected by external irritating factors, it is guaranteed that 50% of the blood will be expelled with each contraction. If a person is concerned about his health, then after the age of 40, it is recommended to undergo an annual physical examination with a cardiologist.
The correctness of the prescribed therapy also depends on determining the individual threshold. An insufficient amount of processed blood causes a deficiency of oxygen supply in all organs, including.
Causes of reduced cardiac ejection fraction
The following pathologies lead to a decrease in cardiac output:
- coronary heart disease;
- myocardial infarction;
- heart rhythm disturbances (arrhythmia, tachycardia);
- cardiomyopathy.
Each pathology of the heart muscle affects the functioning of the ventricle in its own way. During coronary heart disease, blood flow decreases; after a heart attack, the muscles become covered with scars that cannot contract. Rhythm disturbances lead to deterioration of conductivity, rapid wear and tear of the heart, and lead to an increase in muscle size.
At the first stage of any disease, the ejection fraction does not change much. The heart muscle adapts to new conditions, the muscle layer grows, and small blood vessels are rebuilt. Gradually, the capacity of the heart is exhausted, the muscle fibers are weakened, and the volume of absorbed blood decreases.
Other diseases that reduce cardiac output:
- angina pectoris;
- hypertension;
- aneurysm of the ventricular wall;
- infectious and inflammatory diseases (pericarditis, myocarditis,);
- myocardial dystrophy;
- cardiomyopathy;
- congenital pathologies, violation of the structure of the organ;
- vasculitis;
- vascular pathologies;
- hormonal imbalances in the body;
- diabetes mellitus;
- obesity;
- gland tumors;
- intoxication.
Symptoms of reduced ejection fraction
A low ejection fraction indicates serious cardiac pathologies. Having received a diagnosis, the patient needs to reconsider his lifestyle and eliminate excessive stress on the heart. Emotional disorders can cause the condition to worsen.
The patient complains of the following symptoms:
- increased fatigue, weakness;
- feeling of suffocation;
- breathing problems;
- difficulty breathing when lying down;
- visual disturbances;
- loss of consciousness;
- heart pain;
- increased heart rate;
- swelling of the lower extremities.
At more advanced stages and with the development of secondary diseases, the following symptoms occur:
- decreased sensitivity of the limbs;
- liver enlargement;
- lack of coordination;
- weight loss;
- nausea, vomiting, blood in;
- abdominal pain;
- accumulation of fluid in the lungs and abdominal cavity.
Even if there are no symptoms, this does not mean that the person does not have heart failure. Conversely, pronounced symptoms listed above will not always result in a reduced percentage of cardiac output.
Ultrasound - norms and interpretation

Ultrasound examination of the heart
An ultrasound examination provides several indicators by which the doctor judges the condition of the heart muscle, in particular the functioning of the left ventricle.
- Cardiac output, normal 55-60%;
- The size of the atrium of the right chamber, the norm is 2.7-4.5 cm;
- Aortic diameter, normal 2.1-4.1 cm;
- The size of the atrium of the left chamber, the norm is 1.9-4 cm;
- Stroke volume, norm 60-100 cm.
It is important to evaluate not each indicator separately, but the overall clinical picture. If there is a deviation from the norm up or down in only one indicator, additional research will be required to determine the cause.
When is treatment for reduced ejection fraction required?
Immediately after receiving the ultrasound results and determining a reduced percentage of cardiac output, the doctor will not be able to determine a treatment plan and prescribe medications. The cause of the pathology should be dealt with, and not with the symptoms of reduced ejection fraction.
Therapy is selected after a complete diagnosis, determination of the disease and its stage. In some cases this is drug therapy, sometimes surgical intervention.
How to increase reduced ejection fraction?
First of all, medications are prescribed to eliminate the root cause of the reduced ejection fraction. A mandatory part of treatment is taking drugs that increase myocardial contractility (cardiac glycosides). The doctor selects the dosage and duration of treatment based on test results; uncontrolled use can lead to glycoside deficiency.
Heart failure is treated not only with pills. The patient must control the drinking regime; the daily volume of fluid consumed should not exceed 2 liters. It is necessary to remove salt from the diet. Additionally, diuretics, beta-blockers, ACE inhibitors, and Digoxin are prescribed. Medicines that reduce the heart's need for oxygen will help alleviate the condition.
Modern surgical methods restore blood flow in case of coronary disease and eliminate severe heart defects. An artificial heart driver can be installed for arrhythmia. The operation is not performed if the percentage of cardiac output drops below 20%.
Prevention
Preventive measures are aimed at improving the condition of the cardiovascular system.
- Active lifestyle.
- Classes.
- Proper nutrition.
- Quitting bad habits.
- Outdoor recreation.
- Relief from stress.
What is cardiac ejection fraction:
Did you like it? Like and save on your page!
Today, due to poor ecology, many people have unstable health. This applies to all organs and systems in the human body. Therefore, modern medicine has expanded its methods for studying pathological processes. Many patients wonder what cardiac ejection fraction (EF) is. The answer is simple, this condition is the most accurate indicator that can determine the level of performance of the human cardiac system. More precisely, the strength of the muscle at the moment of impact of the organ.
The cardiac ejection fraction can be defined as the percentage of the amount of blood that passes through the vessels in the systolic state of the ventricles.
For example, at 100 ml, 65 ml of blood enters the vascular system, respectively, the cardiac output of the heart fraction is 65%. Any deviations in one direction or another are an indicator of the presence of a disease that requires immediate treatment.
In most cases, measurements are taken from the left ventricle because blood flows from it into the systemic circulation. When there is a decrease in the amount of distilled contents, this is usually a consequence.
Diagnostics such as left ventricular ejection fraction are prescribed to patients who have:
- Intense.
- Systematic failures in the functioning of the organ.
- Shortness of breath and...
- Frequent fainting and dizziness.
- Weakness and fatigue.
- Decreased performance.
In most cases, during the examination, an ultrasound () of the heart and a cardiogram are prescribed. These studies provide output levels in the left and right side of the heart. Such diagnostics are quite informative and accessible to all patients.
Reasons
In fact, the causes of low cardiac ejection fraction are malfunctions of the organ. Heart failure is considered a condition that occurs as a result of long-term disruption of the system. This pathology can be caused by inflammatory diseases, malfunctions of the immune system, genetic and metabolic predisposition, pregnancy and much more.
Often the cause of heart failure is the presence of organ ischemia, a previous heart attack, a combination of hypertension and coronary artery disease, and valvular malformations.
Most often, symptoms of a reduced ejection fraction of the heart manifest themselves in a malfunction of the organ. To clarify the diagnosis, you need to undergo a detailed examination and undergo a lot of tests.
If necessary, the doctor prescribes a number of pharmacological drugs that can cause increased heart function. This applies to patients of any age category from infants to elderly patients.

Treatment
The most popular methods of treating low cardiac ejection fraction are the use of medications. In cases where the main cause of this pathological process is heart failure, treatment is selected for the patient taking into account the age and characteristics of the body.
Dietary restrictions are almost always recommended, as well as a reduction in fluid intake. You need to drink no more than 2 liters per day, and then only clean, non-carbonated water. It is worth noting that for the entire period of treatment it is necessary to almost completely avoid eating salt. A number of ACE inhibitors, digoxin and beta-blockers are prescribed.
All of the above agents significantly reduce the volume of circulating blood masses, which accordingly reduces the level of functioning of the organ. A number of other drugs can reduce the body's need for oxygen, while at the same time making its functionality more effective and at the same time less expensive. In some advanced cases, surgical intervention is used to restore blood flow in all coronary vessels. A similar method is used when.
In cases of severe defects and pathological processes, only surgery in combination with drug therapy is used as treatment. If necessary, artificial valves are installed that can prevent many other heart failures, including fibrillation. Instrumental methods are used as a last resort, when drug therapy is unable to eliminate certain problems in the functioning of the cardiac system.
Norm
To determine the natural rate of cardiac ejection fraction, a special Simpson or Teicholz table is used. It is worth noting that only after a complete examination can the doctor establish an accurate diagnosis and accordingly prescribe the most adequate treatment.
The presence of any pathological processes in the cardiac system is due to a regular lack of oxygen () and nutrients. In such cases, the heart muscles need support.
As a rule, all data is calculated using special equipment that can detect the presence of deviations. Most modern specialists, when using ultrasound diagnostics, prefer the Simpson method, which gives the most accurate results. The Teicholz formula is used less frequently. The choice in favor of one or another diagnostic method is made by the attending physician based on the test results and the patient’s health condition. The ejection fraction of the heart must be normal at any age, otherwise failures can be considered a pathology.
The exact result of both methods is considered to be in the range of 50-60%. A slight difference between them is allowed, but not more than 10%. Ideally, the normal heart fraction in adults is exactly this percentage level. Both methods are considered highly informative. As a rule, according to the Simpson table, the outlier is 45%, and according to Teicholz - 55%. When the values decrease to 35-40%, this is evidence of an advanced degree of heart failure, which can be fatal.
Normally, the heart should push out at least 50% of the blood it pumps. When this level decreases, heart failure occurs; in most cases it is progressive, which affects the development of pathological processes in many internal organs and systems.
The normal ejection fraction in children varies from 55 to 70%. If its level is below 40-55%, then this already indicates a malfunction of the heart. To prevent such deviations, it is necessary to conduct a preventive examination by a cardiologist.
website - a medical portal about the heart and blood vessels. Here you will find information about the causes, clinical manifestations, diagnosis, traditional and folk methods of treating cardiac diseases in adults and children. And also about how to keep the heart healthy and blood vessels clean until old age.
Do not use the information posted on the site without first consulting your doctor!
The authors of the site are practicing medical specialists. Each article is a concentrate of their personal experience and knowledge, honed over years of study at the university, received from colleagues and in the process of postgraduate training. They not only share unique information in articles, but also conduct a virtual consultation - answer questions you ask in the comments, give recommendations, and help you understand the results of examinations and prescriptions.
All topics, even those that are very difficult to understand, are presented in simple, understandable language and are intended for readers without medical training. For your convenience, all topics are divided into sections.
Arrhythmia
According to the World Health Organization, arrhythmias, irregular heartbeats, affect more than 40% of people over 50 years of age. However, they are not the only ones. This insidious disease is detected even in children and often in the first or second year of life. Why is he cunning? And because it sometimes disguises pathologies of other vital organs as heart disease. Another unpleasant feature of arrhythmia is the secrecy of its course: until the disease goes too far, you may not be aware of it...
- how to detect arrhythmia at an early stage;
- which forms are the most dangerous and why;
- when is enough for the patient, and in what cases is surgery indispensable;
- how and how long do they live with arrhythmia;
- which attacks of arrhythmia require an immediate call to the ambulance, and for which it is enough to take a sedative pill.
And also everything about the symptoms, prevention, diagnosis and treatment of various types of arrhythmias.
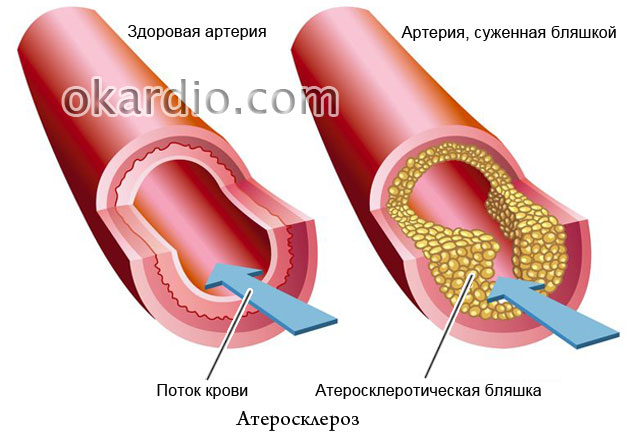
Atherosclerosis
It is written in all newspapers that the main role in the development of atherosclerosis is played by excess cholesterol in food, but why then in families where everyone eats the same, often only one person gets sick? Atherosclerosis has been known for more than a century, but much of its nature remains unsolved. Is this a reason to despair? Of course not! The site’s specialists tell you what successes modern medicine has achieved in the fight against this disease, how to prevent it and how to effectively treat it.
- why margarine is more harmful than butter for people with vascular damage;
- and why it is dangerous;
- why cholesterol-free diets don't help;
- what will patients with;
- how to avoid and maintain mental clarity into old age.
Heart disease
In addition to angina pectoris, hypertension, myocardial infarction and congenital heart defects, there are many other cardiac ailments that many have never heard of. Did you know, for example, that it is not only a planet, but also a diagnosis? Or that a tumor can grow in the heart muscle? The section of the same name talks about these and other heart diseases in adults and children.
- and how to provide emergency care to a patient in this condition;
- what to do and what to do so that the first does not turn into the second;
- why the heart of alcoholics increases in size;
- Why is mitral valve prolapse dangerous?
- What symptoms can you use to suspect that you and your child have heart disease?
- which cardiac diseases are more threatening to women and which ones to men.

Vascular diseases
Vessels permeate the entire human body, so the symptoms of their damage are very, very diverse. Many vascular diseases do not bother the patient much at first, but lead to serious complications, disability and even death. Can a person without medical education identify vascular pathology in himself? Of course, yes, if he knows their clinical manifestations, which this section will talk about.
In addition, here is the information:
- about medications and folk remedies for the treatment of blood vessels;
- about which doctor to contact if you suspect vascular problems;
- what vascular pathologies are deadly;
- what causes veins to swell;
- How to keep your veins and arteries healthy for life.
Varicose veins
Varicose veins (varicose veins) are a disease in which the lumens of some veins (legs, esophagus, rectum, etc.) become too wide, which leads to impaired blood flow in the affected organ or part of the body. In advanced cases, this disease is cured with great difficulty, but at the first stage it can be curbed. Read how to do this in the “Varicose veins” section.
 Click on photo to enlarge
Click on photo to enlarge You will also learn from it:
- what ointments exist for the treatment of varicose veins and which one is more effective;
- why doctors prohibit some patients with varicose veins of the lower extremities from running;
- and who it threatens;
- how to strengthen veins using folk remedies;
- how to avoid blood clots in affected veins.
Pressure
- such a common illness that many consider it... a normal condition. Hence the statistics: only 9% of people suffering from high blood pressure keep it under control. And 20% of hypertensive patients even consider themselves healthy, since their disease is asymptomatic. But the risk of getting a heart attack or stroke is no less! Although it is less dangerous than high, it also causes a lot of problems and threatens with serious complications.

In addition, you will learn:
- how to “deceive” heredity if both parents suffered from hypertension;
- how to help yourself and your loved ones during a hypertensive crisis;
- why blood pressure increases at a young age;
- how to keep your blood pressure under control without medications by eating herbs and certain foods.
Diagnostics
The section devoted to the diagnosis of heart and vascular diseases contains articles about the types of examinations that cardiac patients undergo. And also about indications and contraindications to them, interpretation of results, effectiveness and procedures.
You will also find answers to questions here:
- what types of diagnostic tests even healthy people should undergo;
- why is angiography prescribed for those who have suffered a myocardial infarction and stroke;

Stroke
Stroke (acute cerebrovascular accident) is consistently among the ten most dangerous diseases. People at greatest risk of developing it are people over 55 years of age, hypertensive patients, smokers and those who suffer from depression. It turns out that optimism and good nature reduce the risk of strokes by almost 2 times! But there are other factors that effectively help avoid it.
The section dedicated to strokes talks about the causes, types, symptoms and treatment of this insidious disease. And also about rehabilitation measures that help restore lost functions to those who have suffered from it.

In addition, here you will learn:
- about the differences in clinical manifestations of strokes in men and women;
- about what a pre-stroke condition is;
- about folk remedies for treating the consequences of strokes;
- about modern methods of rapid recovery after a stroke.
Heart attack
Myocardial infarction is considered to be a disease of older men. But the greatest danger it poses is not for them, but for people of working age and women over 75 years of age. It is in these groups that mortality rates are highest. However, no one should relax: today heart attacks overtake even the young, athletic and healthy. More precisely, underexamined.
In the “Heart Attack” section, experts talk about everything that is important to know for everyone who wants to avoid this disease. And those who have already suffered a myocardial infarction will find here many useful tips on treatment and rehabilitation.

- about what diseases a heart attack is sometimes disguised as;
- how to provide emergency care for acute pain in the heart area;
- about differences in the clinical picture and course of myocardial infarction in men and women;
- about an anti-heart attack diet and a heart-safe lifestyle;
- about why a person suffering from a heart attack must be taken to a doctor within 90 minutes.
Pulse abnormalities
When we talk about pulse abnormalities, we usually mean its frequency. However, the doctor evaluates not only the speed of the patient’s heartbeat, but also other indicators of the pulse wave: rhythm, filling, tension, shape... The Roman surgeon Galen once described as many as 27 of its characteristics!

Changes in individual pulse parameters reflect the state of not only the heart and blood vessels, but also other body systems, for example, the endocrine system. Want to know more about this? Read the materials in the section.
Here you will find answers to questions:
- why, if you complain of pulse irregularities, you may be referred for a thyroid examination;
- whether a slow heart rate (bradycardia) can cause cardiac arrest;
- what does it mean and why is it dangerous;
- how heart rate and the rate of fat burning when losing weight are interconnected.
Operations
Many heart and vascular diseases, which 20–30 years ago doomed people to lifelong disability, can now be successfully cured. Typically surgically. Modern cardiac surgery saves even those who until recently were given no chance to live. And most operations are now performed through tiny punctures, rather than incisions, as before. This not only gives a high cosmetic effect, but is also much easier to tolerate. It also reduces the postoperative rehabilitation time by several times.
In the “Operations” section you will find materials about surgical methods for treating varicose veins, vascular bypass surgery, installation of intravascular stents, heart valve replacement, and much more.
You will also learn:
- which technique does not leave scars;
- how operations on the heart and blood vessels affect the patient’s quality of life;
- what are the differences between operations and vessels;
- for what diseases is it performed and what is the duration of a healthy life after it;
- What is better for heart disease - to be treated with pills and injections or to undergo surgery.

Rest
“Rest” includes materials that do not correspond to the topics of other sections of the site. Here you can find information about rare cardiac diseases, myths, misconceptions and interesting facts regarding heart health, unclear symptoms and their significance, the achievements of modern cardiology and much more.
- about providing first aid to yourself and others in various emergency conditions;
- about the child;
- about acute bleeding and methods to stop it;
- o and eating habits;
- about folk methods of strengthening and healing the cardiovascular system.

Drugs
“Drugs” is perhaps the most important section of the site. After all, the most valuable information about a disease is how to treat it. We do not provide here magical recipes for curing serious illnesses with one tablet; we honestly and truthfully tell everything about the drugs as they are. What are they good for and what are they bad for, for whom are they indicated and contraindicated, how do they differ from analogues and how do they affect the body. These are not calls for self-medication, this is necessary so that you have good command of the “weapons” with which you have to fight the disease.

Here you will find:
- reviews and comparisons of drug groups;
- information about what can be taken without a doctor’s prescription and what should never be taken;
- a list of reasons for choosing one or another means;
- information about cheap analogues of expensive imported drugs;
- data on the side effects of heart drugs that manufacturers are silent about.
And many, many more important, useful and valuable things that will make you healthier, stronger and happier!
May your heart and blood vessels always be healthy!

