Classification of congenital heart defects. Congenital heart disease in children and adults. Safe congenital heart defect: mitral valve prolapse
Congenital heart disease is a frightening diagnosis. For recent years The frequency of detection of various cardiac defects in fetuses, children and adolescents has increased significantly due to the active use of echocardiography (ultrasound of the heart). Let's look at the most common congenital anomalies cardiovascular system and find out what to expect from them.
Advisors: Dr. Gilles Delage, Gemas-Quebec, Saint-Laurent; Noni McDonald, Dalhousie University, Halifax. Variations that take into account the patient's situation may make a difference. Respiratory syncytial infection in children with congenital heart disease: a review. Epidemiology of respiratory syncytial viral infection in Washington, D.C., infection and disease by age, immunological status, race, and gender.
Textbook of children's infectious diseases. Improved outcome of respiratory syncytial infection in a high-priority hospitalized population of Canadian children. Pediatric Infection Research Network of Canada. The Pediatric Infection Research Network of Canada studying the admission and treatment of hospitalized patients with respiratory syncytial virus.
Congenital heart defect No. 1: bicuspid aortic valve
Normal aortic valve consists of three doors. The valve, consisting of two leaflets, is a congenital heart defect and is a common cardiac anomaly (found in 2% of the population). In boys, this form of congenital heart disease develops 2 times more often than in girls. As a rule, the presence bicuspid valve aorta has no clinical manifestations (sometimes specific murmurs are heard in the heart area) and is an accidental finding during echocardiography (ultrasound of the heart). Timely detection of this congenital heart defect is important from the point of view of preventing the development of complications such as infective endocarditis And aortic stenosis(failure), arising as a consequence of the atherosclerotic process.
Severe respiratory syncytial virus infection among otherwise healthy preterm infants: what are we trying to prevent? Does Ribavirin have an effect in the hospital of children with respiratory syncytial virus infection? Respiratory syncytial infections in hospitalized patients. Collaborative Network of Pediatric Infection Researchers in Canada.
Hospital-acquired respiratory syncytial virus infection in Canadian pediatric hospitals: The Canadian Pediatric Infection Research Network. Impact of respiratory syncytial virus infection on surgery for congenital heart disease: postoperative course and outcome.
In the uncomplicated course of this congenital heart defect, treatment is not carried out, and physical activity is not limited. Mandatory preventive measures are an annual examination by a cardiologist, prevention of infective endocarditis and atherosclerosis.
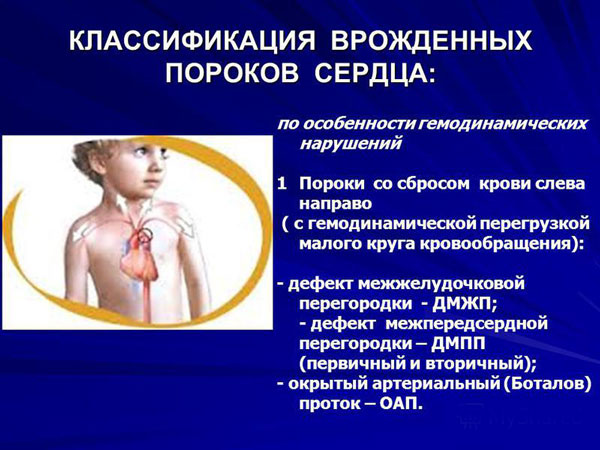
Congenital heart defect No. 2: ventricular septal defect
Under defect interventricular septum understand such a congenital malformation of the septum between the right and left parts of the heart, due to which it has a “window”. In this case, communication occurs between the right and left ventricles of the heart, which should not normally exist: arterial and venous blood in the body healthy person never mix.
Respiratory syncytial virus in patients with congenital heart defects: modern look on the epidemiology and success of preoperative screening. Prophylactic administration of respiratory syncytial virus immune globulin for children and children with high risk. Respiratory syncytial virus immune globulin research group.
Safety assessment of palizuzumab in the second season of exposure in children early age, at risk severe respiratory syncytial virus infection. Risk primary infection and reinfection with respiratory syncytial virus. The term congenital means congenital or present at birth. A congenital heart defect occurs when the heart or blood vessels near the heart do not normally develop until birth. Congenital heart defects affect about 1% of live newborns and are the most common congenital malformations in newborns.
Ventricular septal defect is in 2nd place among birth defects heart by frequency of occurrence. It is detected in 0.6% of newborns, is often combined with other anomalies of the heart and blood vessels, and occurs with approximately equal frequency among boys and girls. Often the occurrence of a ventricular septal defect is associated with the presence of diabetes mellitus and/or alcoholism. Fortunately, the “window” quite often closes spontaneously during the first year of a child’s life. In this case ( normal indicators, characterizing the functioning of the cardiovascular system), the baby recovers: he does not require either outpatient observation by a cardiologist or restriction of physical activity.
In most cases, we don't know what the reason is. Treatment of congenital heart defects has advanced significantly. Nowadays, most congenital heart babies can enjoy an active and busy life. There are several types of congenital heart defects. To help you better understand them, you may need to look at the anatomy of the heart.
Obstruction of blood circulation. This is an obstruction or narrowing that partially or completely blocks blood circulation. This obstruction can occur in the heart valves, arteries, or veins. The three most common forms. Pulmonary stenosis The pulmonary valve narrows. Therefore, the lower right chamber of the heart must pump harder than usual to overcome this obstacle. This can overload the right ventricle and cause an increase in its volume.
The diagnosis is established based on clinical manifestations and confirmed by echocardiography.
Character treatment of this congenital heart defect depends on the size of the ventricular septal defect and the presence of its clinical manifestations. If the size of the defect is small and there are no symptoms of the disease, the prognosis for the disease is favorable - the child does not need drug treatment and surgical correction. Such children are shown preventive therapy antibiotics before performing interventions that can lead to the development of infective endocarditis (for example, before performing dental procedures).
Aortic stenosis The aortic valve, which controls blood flow between the lower left cavity of the heart and the aorta, narrows the large artery that contains oxygenated blood from the heart and to the rest of the body, making it more difficult for the heart to pump blood into the body.
Aortic coarctation The aorta becomes pinched or tightened, affecting blood flow to lower limbs body and causes an increase blood pressure above the constricting area. Septic defects development. When a baby is born with a perforation in the wall that separates the right ventricle from the left ventricle, blood circulates between the two ventricles rather than moving normally to the rest of the body. This problem can cause the heart to become enlarged. It is better called a “hole in the heart.” The two most common forms are.
If there is a defect in the middle and large size in combination with signs of heart failure, conservative therapy with the use of drugs that reduce the severity of heart failure (diuretics, antihypertensive drugs, cardiac glycosides) is indicated. Surgical correction of this congenital heart defect is indicated for large sizes defect, lack of effect from conservative therapy(continuing signs of heart failure), if signs are present pulmonary hypertension. Usually surgical treatment carried out for children under 1 year of age.
This allows blood in the left atrium to return to right atrium through this hole. Some of the blood that was pumped into the left ventricle after passing through the lungs passes through this opening into the right ventricle, instead of being pumped into the aorta to the rest of the body. The arterial canal, a circulating pathway that normally closes after birth, does not close completely and causes too much blood flow into the lungs. The severity of the problem depends on the size of the opening and the level of prematurity.
Currently, there are drugs that can close the arterial canal without resorting to surgery. However, if none of these drugs work, surgery is required. Cyanogenic congenital disease hearts. In the presence of this type of anomaly, the blood pumped into the body contains lower than normal level oxygen, a condition called "cyanosis", which is a bluish discoloration of the skin caused by low concentrations of oxygen in the blood. The term "blue baby" is often used to describe cyanotic babies.
If there is a small defect that is not an indication for surgery, the child is under medical supervision by a cardiologist and must undergo preventive therapy for infective endocarditis. Children who have undergone surgery to correct this congenital heart defect should also be examined regularly (twice a year). pediatric cardiologist. The degree of limitation of physical activity in children with various ventricular septal defects is determined individually, according to the examination of the patient.
A large hole in the wall that separates the two lower chambers of the heart and which allows oxygen-rich blood to mix with oxygen-rich blood; a narrowing in or just above the pulmonary valve that blocks blood flow between right side heart and lungs; the lower right cavity is more muscular than normal; The aorta is supported directly against the lower chambers of the heart and allows oxygenated blood to flow into the aorta. Transpose large vessels The position of the pulmonary artery and aorta was reversed.
Additionally, there is a hole between the left and right sides of the heart. The aorta communicates with the right ventricle, and therefore most of the blood returning to the heart is recirculated without first passing through the lungs. As for the pulmonary artery, it communicates with the left ventricle, so that blood from the lungs returns directly to the lungs.
Vascular congenital heart disease: patent ductus arteriosus
Patent ductus arteriosus is also a common congenital heart defect. The patent ductus arteriosus is a vessel through which prenatal period development, blood is discharged from the pulmonary artery into the aorta, bypassing the lungs (since the lungs do not function in the prenatal period). When, after the birth of a child, the lungs begin to fulfill their function, the duct becomes empty and closes. Normally, this occurs before the 10th day of life of a full-term newborn (more often the duct closes 10-18 hours after birth). In premature babies, the patent ductus arteriosus may remain open for several weeks.
Ebstein's disease. In this rare deformity, the tricuspid valve, which controls the flow of blood from the upper right chamber of the heart to the lower right cavity, lower than normal, making the ventricle too small and the atrium too small. big. The most common signs of congenital heart defects are: a heart murmur.
A bluish tint to the skin, lips and nails; accelerated breathing; dyspnea; poor nutrition, especially in infants, because they get tired quickly during feeding; low weight gain in infants; fatigue during exercise or during physical activity. A congenital anomaly may be discovered during pregnancy, after birth, or mature age when the body needs more heart. If heart failure is suspected, the child is referred to a pediatric cardiologist who will review the family history and medical history, conduct medical examination and request tests, which may include.
If the closure of the aortic duct does not occur within the prescribed time frame, doctors talk about non-closure of the aortic duct. The detection rate of this congenital heart defect in full-term children is 0.02%, in premature and low-birth-weight children - 30%. In girls, a patent aortic duct is detected much more often than in boys. Often this type of congenital heart defect occurs in children whose mothers had rubella or abused alcohol during pregnancy. The diagnosis is established based on the identification of a specific cardiac murmur and is confirmed by echocardiography with Doppler ultrasound.
Electrocardiogram Echocardiogram Chest X-ray treatment cardiac catheterization. Most birth defects can be treated with medication or surgery. Lifestyle choices are important. Source: Heart and Stroke Foundation Dilated cardiomyopathy is a disease that affects the heart muscle and compromises the heart's ability to effectively pump blood to the rest of the body.
What is dilated cardiomyopathy?
Dilated cardiomyopathy is a disease that primarily affects the left ventricle, the part of the heart that sends blood to the rest of the body through the aorta. This is an enlarged ventricle that is associated with a decreased ability to pump blood.
Treatment Patent aortic duct begins from the moment of detection of congenital heart disease. Newborns are prescribed drugs from the group of nonsteroidal anti-inflammatory drugs (indomethacin), which activate the process of closing the duct. In the absence of spontaneous closure of the duct, surgical correction anomalies during which the aortic duct is ligated or excised.
What are the causes of dilated cardiomyopathy?
In many cases, it is impossible to trace the causes of cardiac enlargement, so dilated cardiomyopathy is defined as idiopathic. There are various reasons why the heart can grow: genetic mutations, birth defects, infections, alcohol or drug abuse, some chemotherapy agents, exposure toxic substances such as lead, mercury and cobalt, and cardiovascular diseases, such as for example.
What are the symptoms of dilated cardiomyopathy?
In general, symptoms of dilated cardiomyopathy are symptoms of heart failure or due to an arrhythmia and may include weakness, mild fatigue, shortness of breath during sometimes even modest exertion or when lying down, persistent dryness from the legs and, caused by, loss of appetite, palpitations or.
Forecast in children with corrected congenital heart disease, favorable, in physical limitations, special care and such patients do not require observation. In premature babies with open ductus arteriosus Chronic bronchopulmonary diseases often develop.
Coarctation of the aorta
Coarctation of the aorta is a congenital heart defect manifested by narrowing of the aortic lumen. Most often, the narrowing is localized at a short distance from the place where the aorta exits the heart. This congenital heart defect ranks 4th in frequency of occurrence. In boys, coarctation of the aorta is found 2-2.5 times more often than in girls. Middle age a child diagnosed with coarctation of the aorta - 3-5 years old. Often this congenital heart defect is combined with other anomalies in the development of the heart and blood vessels (bicuspid aortic valve, ventricular septal defect, vascular aneurysms, etc.).
How to prevent dilated cardiomyopathy?
The risk of developing dilated cardiomyopathy can be reduced by avoiding smoking, drinking alcohol only in moderation, not using drugs, maintaining correct weight with both healthy and balanced diet and regular exercise adapted to your conditions. health.
If you have symptoms of possible dilated cardiomyopathy, your doctor may prescribe following tests. It may have several changes, including signs of a previous heart attack or signs of left ventricular strain or arrhythmias: This is an imaging test that displays the structures of the heart and the functioning of its moving parts. The device sends a beam of ultrasound into the chest, through a probe lying on its surface, and repeatedly produces ultrasound reflexes that return to the same probe after interacting differently with different components of the cardiac structure. This is a key exam: it allows you to evaluate the size and thickness of the walls of the heart chambers, contractile function and the functioning of the valves, as well as assess the pressure in the lungs. Oxygen consumption stress test: the exam consists of recording an electrocardiogram while the patient performs physical exercise, usually walking on a treadmill or pedaling an exercise bike; The mouthpiece is also used to measure expired gases. This allows you to obtain multiple information, among which the most important are resistance to the exercise of the test item and the appearance of signs of ischemia under stress: it is an exam that allows you to visualize coronary vessels by injecting a radiopaque contrast medium inside them. The exam is carried out in a special radiology room, where all necessary measures sterility. Injection of contrast in the coronary arteries involves selective catheterization of the artery and advancement of the catheter to the origin of the vessels being examined. It serves to exclude the presence significant illness coronary artery. Cardiac catheterization: invasive method, which involves inserting a small tube into a blood vessel, then inserting a catheter into the heart and allowing important information about the flow and oxygenation of blood and about the pressure inside the chambers of the cardiac and pulmonary arteries and veins. Endomyocardial biopsy: Performed during cardiac catheterization using an instrument called a biotome. Biopsies are usually performed with right side interventricular septum. In patients with recent dilated cardiomyopathy and "fulminant" heart failure, the presence and, in the case of, identification of the type of cells that support inflammatory process because it is important prognostic value. Magnetic resonance imaging with contrast: provides detailed images of the structure of the heart and blood vessels by recording the signal emitted by cells subjected to intense magnetic field. In the case of familial dilated cardiomyopathies, one can look for genetic mutations associated with the development of dilated cardiomyopathy; if a mutation is identified that is associated with the development of dilated cardiomyopathy, then "healthy" family members can be studied: those who test negative for the mutation can be confident that they will not develop it. The test is carried out according to predefined protocols. . When the cause of dilated cardiomyopathy is known, it is removed or corrected if possible.
Diagnosis It is often discovered by chance when examining a child for a non-cardiological disease (infection, injury) or during a medical examination. Suspicion of the presence of coarctation of the aorta arises when identifying arterial hypertension(high blood pressure) in combination with specific murmurs in the heart. The diagnosis of this congenital heart defect is confirmed by the results of echocardiography.
Treatment coarctation of the aorta - surgical. Before surgery to correct a congenital heart defect, full examination child, therapy is prescribed to normalize the level blood pressure. Subject to availability clinical symptoms surgical treatment is carried out in as soon as possible after diagnosis and preparation of the patient. If the defect is asymptomatic and there are no concomitant cardiac anomalies, the operation is performed routinely at the age of 3-5 years. Choice surgical technique depends on the patient’s age, the degree of narrowing of the aorta, and the presence of concomitant anomalies of the heart and blood vessels. The frequency of repeated narrowing of the aorta (recoarctation) is directly dependent on the degree of initial narrowing of the aorta: the risk of recoarctation is quite high if it is 50% or more of the normal value of the aortic lumen.
After surgery, patients need systematic observation pediatric cardiologist. Many patients who undergo surgery for coarctation of the aorta must continue taking antihypertensive medications for several months or years. After the patient leaves adolescence, he is transferred under the supervision of an “adult” cardiologist, who continues to monitor the patient’s health throughout his (the patient’s) life.
Acceptable degree physical activity is determined individually for each child and depends on the degree of compensation for the congenital heart defect, blood pressure level, timing of the operation and its long-term consequences. To complications and long-term consequences Coarctation of the aorta includes recoarctation and aneurysm ( pathological expansion lumen) of the aorta.
Forecast. The general trend is this: the earlier coarctation of the aorta is identified and eliminated, the higher the patient’s life expectancy. If a patient with this congenital heart defect is not operated on, average duration his life span is approximately 35 years.
Safe congenital heart defect: mitral valve prolapse
Prolapse mitral valve- one of the most frequently diagnosed cardiac pathologies: according to various sources, this change occurs in 2-16% of children and adolescents. This type of congenital heart disease is a bowing of the mitral valve leaflets into the cavity of the left atrium during contraction of the left ventricle, which leads to incomplete closure of the leaflets of the above valve. Because of this, in some cases there is a reverse flow of blood from the left ventricle into the left atrium (regurgitation), which should not normally occur. Over the past decade, due to the active introduction of echocardiographic examination, the detection rate of mitral valve prolapse has increased significantly. Mainly - due to cases that could not be detected by auscultation (listening) of the heart - so-called “silent” mitral valve prolapse. These congenital heart defects, as a rule, do not have clinical manifestations and are a “find” during medical examination of healthy children. Mitral valve prolapses are quite common.
Depending on the cause of occurrence, mitral valve prolapses are divided into primary (not associated with heart disease and pathology connective tissue) and secondary (arising against the background of diseases of connective tissue, heart, hormonal and metabolic disorders). Most often, mitral valve prolapse is detected in children aged 7-15 years. But if before the age of 10 prolapse occurs equally often in boys and girls, then after 10 years prolapse is found 2 times more often in the fairer sex.
It is important that the incidence of mitral valve prolapse increases in children whose mothers had a complicated pregnancy (especially in the first 3 months) and/or pathological birth(fast, rapid labor, C-section for emergency indications).
Clinical manifestations in children with mitral valve prolapse vary from minimal to severe. Main complaints: pain in the heart area, shortness of breath, sensations of palpitations and interruptions in the heart, weakness, headaches. Often in patients with mitral valve prolapse, psycho-emotional disorders(especially in adolescence) - most often in the form of depressive and neurotic states.
Diagnosis mitral valve prolapse, as already mentioned, is diagnosed on the basis clinical picture and the results of cardiac auscultation, and is confirmed by echocardiography data. Depending on the degree of deflection of the valve leaflets, as well as the presence or absence of disturbances in intracardiac blood flow ( intracardiac hemodynamics) there are 4 degrees of mitral valve prolapse. The first two degrees of mitral valve prolapse are detected most often and are characterized by: minimal changes according to cardiac ultrasound.
The course of mitral valve prolapse is favorable in the vast majority of cases. Very rarely (about 2%) complications such as the development of mitral insufficiency, infective endocarditis, severe violations heart rate etc.
Treatment patients with mitral valve prolapse should be comprehensive, long-term and individually selected, taking into account all available medical information. Main directions in therapy:
- Compliance with the daily routine (a full night's sleep is required).
- Fighting outbreaks chronic infection(e.g. sanitation and, if necessary, removal palatine tonsils if available chronic tonsillitis) - to prevent the development of infective endocarditis.
- Drug therapy (mainly aimed at general strengthening body, normalization metabolic processes and synchronization of the central and autonomic nervous systems).
- Not drug therapy(includes psychotherapy, auto-training, physiotherapy, water procedures, reflexology, massage).
- Movement. Because most children and adolescents with mitral valve prolapse tolerate physical activity, physical activity in such cases is not limited. It is only recommended to avoid sports involving sudden, jerky movements (jumping, wrestling). Limitation of physical activity is resorted to only when prolapse with impaired intracardiac hemodynamics is detected. In this case, in order to avoid detraining, physical therapy classes are prescribed.
Preventive examinations and examination of children and adolescents with mitral valve prolapse should be carried out at least 2 times a year by a pediatric cardiologist.
About the prevention of congenital heart defects
Congenital heart defects, like other developmental defects internal organs, do not arise out of nowhere. There are about 300 reasons that disrupt development little heart, while only 5% of them are genetically determined. All other congenital heart defects are the result of influence on expectant mother external and internal unfavorable factors. These factors include:
- various types of radiation;
- medications not intended for pregnant women;
- infectious diseases(especially viral nature, for example, rubella);
- contact with heavy metals, acids, alkalis;
- stress;
- drinking, smoking and drugs.
Congenital defects in the development of the heart muscle or blood vessels can be identified as early as the 20th week of pregnancy - which is why all pregnant women are advised to undergo planned ultrasound examinations. Certain ultrasound signs allow one to suspect the presence of cardiac pathology in the fetus and refer the expectant mother for additional examination to a special institution that diagnoses cardiac pathologies. If the diagnosis is confirmed, doctors assess the severity of the defect, determine possible treatment. A baby with a congenital heart defect is born in a specialized hospital, where he is immediately provided with cardiac care.
Thus, actions aimed at preventing the occurrence of developmental defects, their timely detection and treatment will help, at a minimum, improve the child’s quality of life and increase its duration, and, at maximum, prevent the occurrence of abnormalities of the cardiovascular system. Take care of your health!
Heart defects are abnormal pathological changes in the valves of an organ, its walls, septa or large vessels.
As a result of such changes, normal blood circulation in the myocardium is disrupted, which leads to the development of failure and oxygen starvation many organs.
Defects in the anatomical structure of the heart occur for many reasons. Pathologies of this kind lead to improper functioning of the body and cause many irreversible complications.
- All information on the site is for informational purposes only and is NOT a guide to action!
- Can give you an ACCURATE DIAGNOSIS only DOCTOR!
- We kindly ask you NOT to self-medicate, but make an appointment with a specialist!
- Health to you and your loved ones!
Types by etiological factor
Heart defects are divided into two main types regarding the mechanism of occurrence: and.
Each of them is divided into its own groups, types and classifications, however, they all have a common place of localization:
- in the valve apparatus;
- in the walls of the heart muscle;
- in large cardiac vessels.
Danger of this disease is that any pathological change in the heart lead to poor circulation. It is caused by a slowdown in blood flow and its stagnation in vascular system. All this provokes many diseases associated with hypoxia and nutritional deficiencies.
Both types of heart defects arise for almost the same reasons. But their development occurs at completely different times.
| Congenital |
|
| Purchased | Such defects can occur at any age. The classification of acquired heart defects is divided according to the causes of the disease, which can be organ trauma or serious illnesses. infectious diseases, a complication of which is rheumatism, namely:
Among other things, acquired defects often develop as a result of injuries to the walls of the heart, coronary disease, chronic hypertension, etc. |
Types according to defects in the anatomical structure of heart structures
In addition to the mechanism of occurrence, heart defects are also usually divided into types based on the location of the defect, their complexity and characteristics of the consequences.
Thus, cardiac anomalies among doctors are divided into the following types:
Based on the location of the defects, the disease is classified into the following classification:
- valve defects;
- defects of the interventricular septum;
Which, in turn, are divided into:
Also for defects in anatomical structure heart diseases distinguish the following diseases:
In addition, all these types and types are distinguished by their combinations, when the patient has two or more anatomical changes listed above.
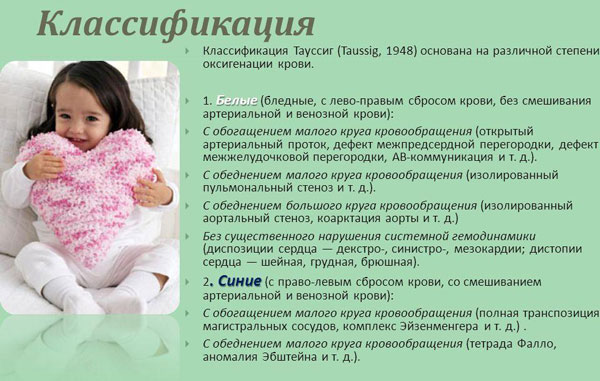
Division by hemodynamics
Based on hemodynamics, heart defects are divided into four degrees, differing in the existing changes and their development:
- minor changes;
- moderately manifested;
- sudden changes;
- terminal.
All these degrees are characterized by the presence of symptoms that occur when there is a lack of oxygen in a certain place in the body.
Based on the characteristics of the consequences, cardiac anomalies of this kind are grouped into the following types:
White defects according to the degree of development and localization of hypoxia are divided into four types:
Blue defects, unlike white ones, have only two types, characterized by enrichment or depletion of the pulmonary (pulmonary) circulation.
In addition, heart defects are divided into four degrees, determined based on circulatory disorders.
Each of them is characterized by worsening symptoms, the presence of complications and the severity of treatment:
- slight deterioration in blood circulation;
- moderate change;
- noticeably obstructed blood flow;
- terminal damage to the blood flow.
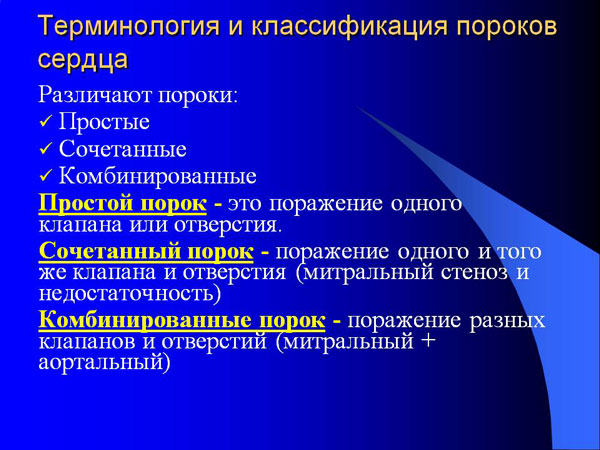
Combined
Combined cardiac defects are quite common. Their clinical and anatomical picture consists of a set of signs present in each defect individually. But at the same time, some symptoms still change, which is manifested by their weakening or worsening.
Combined defects are classified into:
|
|
| Triad of Fallot | Pathology is determined by stenosis on the side pulmonary trunk, changes in the septum separating the ventricles, and hypertrophy of the right ventricle. |
| A disease that has a defect in the atrial septum, combined with the pathologies of Tetralogy of Fallot. | |
| Congenital defects characterized by the presence of heart failure from the tricuspid valve and. |
To determine combined anomalies, several methods must be used instrumental diagnostics. Most often, X-rays are used for this. chest, electrocardiogram, echocardiography and cardiac catheterization.
In case of ventricular septal defects and coartation of the aorta, the following signs will be observed:
- dyspnea;
- headaches;
- causeless fatigue;
- swelling of the veins in the neck;
- pulsation and enlargement of the liver;
- weakness in the legs;
- nosebleeds;
- angina pectoris.
Tetralogy of Fallot and patent arteriosus are manifested by swelling of the veins in the extremities, erythrocetosis, swelling, shortness of breath and rapid heartbeat. Besides, combined defects Symptoms include extraneous noises in the chest area, cough, heart pain and cyanosis of the skin.
Classification of heart defects by location of defects
Regardless of the etiology, types and types of heart defects, they are also usually divided according to the location of the defects:
- in the mitral valve;
- in the aortic valve;
- in the tricuspid;
- pulmonary;
- in the foramen ovale.
Each location of pathology is responsible for a certain malfunction in the functioning of the vascular and cardiac systems, and also has its own clinical manifestation and complications.
Such vices are divided according to anatomical changes. Among which are stenosis, insufficiency, hypoplasia and atresia. All of them have a direct effect on blood circulation and cause irreparable harm to health.
Let's consider heart defects by localization of anomalies in more detail:
| Mitral valve | The mitral valve is located between the left ventricle and the atrium. It consists of several parts, each of which can undergo anatomical changes, namely:
Each of these defects provokes mitral valve stenosis, manifested by a narrowing of the lumen between the sections near which it is located. With this defect, the valve flaps thicken and fuse together, which reduces the area of the normal opening to 1.5–2 cm. Most often, the causes are previous infectious diseases and some congenital anomalies in the heart. |
| Aortic valve |
|
| Tricuspid valve |
|
| Pulmonary valve |
|
| Oval hole |
|

